Article highlights
- Clinical Presentation: A 22-month-old with sickle cell disease exhibited acute facial swelling, fever, and lesions. Initial differential included vaso-occlusive crisis, infected hematoma, insect bite, or abuse.
- Diagnostic Evaluation: Imaging and lab tests supported subgaleal hematoma (SGH) suspicion, possibly due to non-accidental trauma. MRI revealed SGH and signs consistent with abuse. Secondary infection was suspected.
- Management: Treatment involved vancomycin. Despite self-resolving hematoma, antibiotics were administered. Child Protective Services were involved, leading to foster care placement.
- Outcome: The patient was discharged with pediatric hematology follow-up. Early detection and intervention are vital in suspected child abuse cases to prevent severe complications.
A 22-month-old female with sickle cell disease on folic acid and penicillin prophylaxis with a 3-day history of nasal congestion, rhinorrhoea, fever and decreased oral intake presents to the emergency department (ED) for acute facial swelling noted when she woke up from a nap. Facial swelling is on the left side, diffuse erythematous and tender involving the left temporal region.
The edematous swelling continues to the back of the ear and feels boggy on palpation. Mother denies history of blood transfusion, vaso-occlusive crisis (VOC), witnessed insect bites, recent travel history, sick contacts, or trauma. Mother discloses being abused by her ex-partner but denies patient being subjected to any physical or sexual abuse.
Vitals in the emergency room are temperature of (103° F), pulse of 163 bpm, respiratory rate of 28 bpm, blood pressure 115/73 mmHg. Physical examination is also evident for extensive erythema and raised lesions over the perineum, labia majora, lower extremities and evident fungal infection on the left nail bed. No patterned abrasions or ptosis observed.
Laboratory workup done in the ED shows hemoglobin (Hb) level 9.4 g/dL, hematocrit (Hct) 27.9%, platelet count 339×103/µL (339×109/L), white blood cell count 10.7×103/µL (10.7×109/L), neutrophil count 84.8% (0.85), lymphocytes 6.5% (0.07). CMP, PT/PTT/INR are all negative and blood cultures are drawn. Imaging workup is done in ED: CT head without contrast (Figure) shows extensive predominant left-sided extracranial soft tissue swelling and is concerning for an abscess within the left inferior temporal extracranial soft tissues. No visible underlying calvaria osteomyelitis or any acute intracranial process. CT of maxillofacial bones shows left-sided soft tissue swelling with limited view due to patient’s positioning.
Due to the acute onset of facial swelling and imaging results concerning for facial abscess, IV ampicillin-sulbactam is started and patient is admitted to inpatient pediatric service for further management. Over the next 24 hours, fever persists, and facial swelling rapidly expands in size now covering left eye, left temporal area and continues to the post-auricular area, boggy in nature, causing left pinna to be pushed anteriorly. Left eye on examination appears swollen, tender and ecchymotic with difficulty in opening.
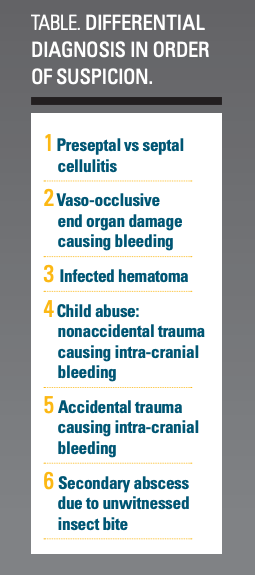
Differential diagnosis
Given the history of HbSS in the patient the possibility of her presentation being an initial symptom of vaso-occlusive crisis causing end organ damage was considered. As the pain predominantly involved the eyelids coupled with the maintenance of vital signs and absence of infarct on imaging the likelihood of vaso-occlusive crisis is diminished. As the concomitant CT imaging obtained in the ED pointed to a facial abscess, an unwitnessed event like an insect bite as a possible cause was considered on the differential.
For our patient, as the facial lesion rapidly progressed causing ptosis and ocular ecchymosis with inability to open her eyes, it became evident that the underlying cause was hemorrhage which could be due to an accidental trauma leading to orbital cellulitis (pre- or postseptal) or nonaccidental trauma due to possible abuse. Hence the differential of an insect bite was rejected. Due to absence of entry wound at the site of lesion the possibility of accidental trauma was diminished. Considering the onset of the high-grade fever, a secondary infected hematoma was now on top of the list.
Adding to this, the presence of other erythematous lesions on the patient’s groin, lower extremities and nails, our suspicion of non-accidental trauma with possible physical abuse leading to intracranial bleeding was heightened. This bleed could be easily infected due to an already increased infectious burden in the patient. Therefore, this scenario appears more cogent when compared to the other aforementioned causes (Table).
Diagnostic evaluation
Infectious disease consult was done due to persistent fevers and recommendation was to start intravenous vancomycin for MRSA coverage. Ophthalmology evaluation ruled out orbital septal cellulitis but could not rule out trauma due to ecchymosis of upper and lower eyelid. Repeat lab work done on day 3 of admission showed: Hb 8.3 g/dL, Hct 24.4%, white blood cells 5.2 ×103/µL (5.2×109/L), neutrophil count 53.4% (0.55), lymphocytes 26.9% (0.27), platelets 271 ×103/µL (271×109/L), CRP 2.10 mg/dL (21 mg/L) and blood culture reported no organism growth for 72 hours. The drop in hemoglobin could be explained by an underlying hematoma. Hence an extensive workup for suspected physical abuse including MRI brain for suspected bleeding, skeletal survey for previous lesions, abdominal USG for other covert bleeding sites was done.
Diagnosis: MRI brain done showed streaky T2 hypointense soft tissue fullness with interspersed edema and streaky internal and peripheral enhancement more towards the left parietal region. This presumably represents subgaleal hematoma, the degree of which is significantly decreased since last CT. Administration for Children's Services (ACS) was notified.
Management/Treatment: As the imaging showed reducing size of subgaleal hematoma, and other radiographs came back negative, patient was kept under observation and frequent neurological checks. Temperature spikes responded well to vancomycin and hence medications were stopped after 5 days. Social services follow-up with ACS revealed that the child was at imminent risk under the current caregiver. The mechanism by which these injuries were sustained was deemed most consistent with hair pulling, a form of child physical abuse causing rupture of emissary veins leading to a subgaleal hematoma (SGH).
Additionally, upon review of photos provided by ACS due to the previously open case revealed the patient had two encounters of sustained extensive abdominal and back bruising. Thus, as the patient had known encounters and potentially other encounters of physical abuse that maybe unknown, it became imperative to intervene as cases of missed abuse can result in death in about 30% of children in the patient’s age group.1
Discussion: infected subgaleal hematoma
A subgaleal hematoma forms when there is bleeding in the potential space between the periosteum and the scalp aponeurosis. This space crosses suture lines and extends from the orbital regions anteriorly to the ears laterally and the neck posteriorly; hemorrhages into this space can cause significant blood loss and sometimes can be life-threatening.2 SGH is rare beyond the neonatal period and is typically associated with head trauma resulting in rupture of emissary veins traversing the subgaleal space.3
A comprehensive literature review confirms the rare incidence of SGH in pediatric population. Of the handful number of cases reported, a varied range of causes including VOC in sickle cell patients, blood dyscrasias like platelet disorders, accidental and non-accidental trauma were seen. Some of the likely clinical presentations in such cases included fluctuant head swelling, isolated headaches, accidental trauma while braiding or combing hair accompanied by coagulation defects to non-accidental intentional physical abuse with hair pulling.3,4,6 Complications of SGH, though rare, can be serious like vision impairment due to extension of hematoma into the orbit resulting in proptosis as seen in our patient or secondary infection with organisms like staphylococcus aureus, streptococcus pneumoniae etc. as suspected in our patient.4-6 The fatal complications of shock and eventual death have also been reported in neonatal cases.3,7 Treatment/management of SGH: thorough history and physical examination are the most important tools for a physician. Laboratory evaluation should consist of hematological profile CBC, coagulation profile, CMP. Co-existing symptoms of fever, erythema and lab finding of raised inflammatory markers should alert the physician to consider secondary infection of the hematoma even without overlying entry wound. Aspiration with cultures and antibiotics may be warranted on a case-by-case basis.
However, due to paucity of such presentations, a well-documented treatment course is unavailable and hence requires a multi-disciplinary approach.4 Although it is not necessary to make the clinical diagnosis, optimal imaging studies for subgaleal hemorrhage include CT or MRI. Radiographs of the skull can be done to identify accompanying fractures.8
Due to the rare presentation of SGH in pediatric age group, keeping a high index of suspicion for evaluation of possible child abuse including but not limited to skeletal survey, abdominal imaging and occult blood testing9 should be considered. As physicians are mandatory reporters of suspected child abuse, it is important to involve local child protective services in your area in such cases. Although most cases of subgaleal hemorrhage resolve spontaneously in 1-5 weeks, a close follow-up is highly recommended.3 In case of expanding hematoma or clinical signs of neurological deficits, involving surgical specialties for drainage is deemed necessary. In our patient, secondary infection of SGH due to non-accidental trauma was likely. As the lesion was self-resolving and child responded well to vancomycin, the decision to drain the hematoma was deferred. The mechanism of secondary infection was postulated to be entry via micro-vasculature due to close proximity to infected nasal sinuses and general increased disease burden in our patient. This hypothesis of microorganism spread was consistent with previously documented case even in the absence of local entry wound and negative blood cultures.4
Patient outcome: Patient was discharged home with foster mom with f/u appointments for pediatric hematology.
Click here for more from the October 2023 issue of Contemporary Pediatrics®.
References:
1. Child Maltreatment 2019. Published May 11, 2021. Accessed March 25, 2023. https://www.acf.hhs.gov/cb/report/child-maltreatment-2019
2. Westphal K, Bakalemwa R, Groothuis E. Scalp swelling and headache in a 12-year-old boy. Pediatr Rev. 2021;42(5):258-261. doi:10.1542/pir.2019-0071
3. Patchana T, Ghanchi H, Taka T, Calayag M. Subgaleal hematoma evacuation in a pediatric patient: A case report and review of the literature. Surg Neurol Int. 2020;11:243. doi:10.25259/SNI_207_2020
4. Salloum S, Sit W, Walton MM, Kamian K. Infected subgaleal hematoma in a 4-month-old girl. Am J Emerg Med. 2021;39:250.e5-250.e6. doi:10.1016/j.ajem.2020.05.090
5. Slap F, Jeurissen A, Van Havenbergh T, Deckers F, Mariën P, Van Mol C. Late onset subgaleal hemorrhage infection with Streptococcus pneumoniae? Eur J Pediatr. 2009;168(6):647-650. doi:10.1007/s00431-009-0922-3
6. Chen CH, Hsieh WS, Tsao PN, Chou HC. Neonatal subgaleal abscess. Eur J Pediatr. 2004;163(9):565-566. doi:10.1007/s00431-004-1481-2
7. Amar AP, Aryan HE, Meltzer HS, Levy ML. Neonatal subgaleal hematoma causing brain compression: report of two cases and review of the literature. Neurosurgery. 2003;52(6):1470-1474; discussion 1474. doi:10.1227/01.neu.0000065180.07961.54
8. Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164(10):1452-1453.
9. Lane WG, Dubowitz H, Langenberg P. Screening for occult abdominal trauma in children with suspected physical abuse. Pediatrics. 2009;124(6):1595. doi:10.1542/peds.2009-0904