A newborn with fever and tremors
In a newborn nursery, a newborn boy shows signs of irritability, high tone, and tremors on day of life 1. His mother’s past medical history is significant for preeclampsia, previous opiate and cocaine abuse, and current tobacco use and she was incarcerated during the pregnancy. What's the diagnosis?
The case
A 40-and-2/7 week gestational age boy was born to a 30-year-old G4P0121 mother via vaginal delivery. The mother’s past medical history is significant for preeclampsia, previous opiate and cocaine abuse, and current tobacco use. Social history is significant as mother was incarcerated during this pregnancy. The mother reports being drug-free throughout this pregnancy despite prior opiate and cocaine use, and her urine drug screen on admission was negative. She received morphine on the maternity ward for pain. In the newborn nursery, the infant showed signs of irritability, high tone, and tremors on day of life 1, at which point he became febrile to 100.4 °F. Upon further inquiry, the mother admitted to cigarette smoking daily in pregnancy, and now admits to daily vaping, as much as 2 vaporized pods daily. The patient was transferred to the neonatal intensive care unit (NICU) for further evaluation.
Physical examination
The physical examination revealed a newborn who was alert, irritable, and difficult to console. He was tachycardic and tachypneic with lungs clear to auscultation bilaterally. His abdomen was soft with active bowel sounds. On neurologic exam, he had increased tone with tremors.
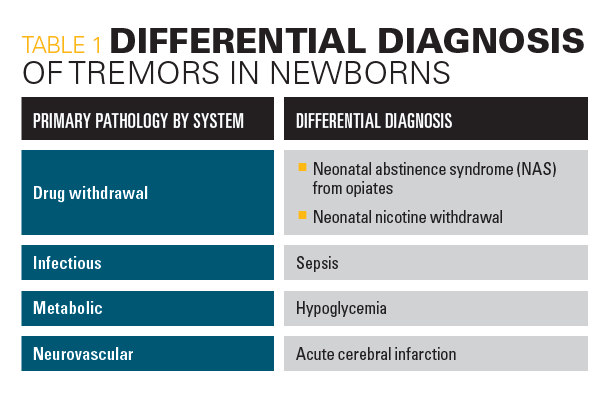
Differential diagnosis
Given the patient’s age, physical exam, and maternal history, a drug withdrawal syndrome was the leading diagnosis. Table 1 shows the differential diagnosis for a newborn with fever and tremors which includes infectious, metabolic, and neurovascular etiologies.
Laboratory studies
A metabolic panel revealed sodium 143 mmol/L, potassium 4.4 mmol/L, chloride 110 mmol/L, CO2 18 mmol/L, BUN 14 mg/dL, creatinine 1.42 mg/ dL, and glucose 75 mg/dL. Urine drug screen was positive for opiates (after maternal morphine was given). Meconium drug screen was negative. C- reactive protein 0.02 mg/dL and blood culture showed no growth for 5 days. Urine nicotine level was less than 2 ng/mL (ref: 2 ng/mL) and urine 3-OH cotinine level was 1399 ng/dL (ref: < 50 ng/dL).
Hospital course
In the NICU, the patient underwent a septic work-up and evaluation for drug exposure. He was started on ampicillin and gentamicin for a 48-hour sepsis rule-out. Because maternal cocaine use is associated with neonatal cerebral infarction, a CT of the head was performed and was unremarkable. A lumbar puncture was attempt- ed but was unsuccessful. The patient was treated with supportive care, including ad lib breast and bottle feedings, swaddling, and a low stimulation environment and improved. Anticonvulsant medications (phenobarbital) were considered, but not needed.
Diagnosis
Nicotine can cross the placenta and cause a significant withdrawal syndrome in newborns. Nicotine metabolite levels, particularly 3-OH cotinine, can be measured in the urine and may be the only positive lab result in a withdrawing infant. In our patient, the urine 3-OH cotinine level of 1399 ng/ dL (ref: < 50 ng/dL) is 28 times the upper limit of normal. All other lab work/ imaging were within normal limits.
Discussion
Vaping, or electronic cigarette use, is a popular mode of nicotine consumption among young adults. Many vaping-related illnesses have been described in the medical literature.1-3 Vaping can affect more than just the individuals who participate. In this case report, we describe the clinical course of a newborn exposed to a significant amount of nicotine in utero secondary to maternal vaping. Because of the popularity of vaping among young adults, it is likely that clinicians will see an emergence of vaping-related complications in both the young adults who vape, and their children.
Differential diagnoses were considered and systemically ruled out. Neonatal abstinence syndrome from opiates is a common etiology for neonatal drug withdrawal symptoms; this was ruled out with the negative maternal urine drug screen and negative newborn meconium drug screen. Neonatal sepsis remains high on the index of suspicion for all newborns with fever. For this reason, the patient was started on empiric antibiotic therapy for 48 hours; however sepsis secondary to bacteremia was ruled out when blood cultures were no growth for 5 days. Hypoglycemia is a common cause of tremors in a newborn; this was ruled out with normal glucose levels. Those who consume nicotine may abuse other drugs simultaneously. The use of maternal cocaine during pregnancy is associated with neonatal cerebral infarction.4 This was on the differential diagnosis for our patient and was ruled out with a normal head CT. In the presence of an elevated urine 3-OH cotinine level and negative work-up for other causes, our patient was given a diagnosis of neonatal nicotine withdrawal.
Nicotine is an addictive substance that is small enough to cross the placenta.5 In the brain, nicotine binds to nicotinic acetylcholine receptors (nAChRs), which are highly expressed in dopaminergic and GABAergic neurons in the ventral tegmental area and the nucleus accumbens.6 Mouse models of nicotine withdrawal have demonstrated that the nAChRs in the medial habenula of the diencephalon and its projection to the interpeduncular nucleus are particularly important mediators of nicotine withdrawal symptoms.7 Multiple organs in the fetus are adversely affected by nicotine exposure. This may manifest as orofacial defects, growth restriction, preterm birth, stillbirth, sudden infant death syndrome, or neonatal withdrawal symptoms.8 In the newborn, withdrawal from nicotine can present in a similar way to opiate withdrawal including irritability, high tone and tremors. Both opiate and nicotine withdrawal will result in high Neonatal Abstinence Scoring System/Finnegan Scores, making the 2 difficult to distinguish. The mother in our study consumed 2 vaporized pods per day, roughly equivalent to 2 packs of tobacco cigarettes per day. The patient’s urine metabolite result of 1399 mg/dL represents a value 28 times the upper limit of normal. This value correlated with the severity of our patient’s withdrawal syndrome.
Among teenagers, e-cigarette use has more than doubled between 2017 and 2019.9 A 2018 survey10 showed 3.6 million middle and high school students had used an e-cigarette in the past 30 days. Nicotine is the most commonly abused substance during pregnancy. Given the popularity of vaping, physicians will encounter more cases of nicotine-related complications than in recent decades. In the newborn nursery or NICU, this may manifest as neonatal nicotine withdrawal.
Providers must maintain a high index of suspicion when evaluating newborns with signs of withdrawal, especially when initial testing for opiates is negative. Meconium drug screening identifies substances that can elicit newborn withdrawal symptoms. Including nicotine and/or its metabolites in the meconium drug screen helps discern the level of exposure and assists in the management of withdrawal symptoms. Here, a urine level of 3-OH cotinine was measured. Although not a routine newborn screen for drug withdrawal, measuring urine 3-OH cotinine was invaluable in confirming the diagnosis of nicotine withdrawal. With this lab result, we were steered away from opioid-related interventions such as methadone and morphine. Measurement of nicotine and/or its metabolites (either in the urine or meconium) should be considered in routine screening tests for newborns with withdrawal symptoms.
Treatment and patient outcome
Nicotine withdrawal in newborns should be managed with supportive care and will self-resolve in days. Phenobarbital may be considered for seizures related to severe withdrawal. IV fluids may be administered if symptoms interfere with feeding and result in dehydration. Our patient’s symptoms resolved over 4 to 5 days. He was followed by a pediatrician for outpatient evaluation and management. Understanding the prevalence of nicotine abuse via e-cigarettes and the severity of the neonatal withdrawal syndrome are essential components of care for exposed newborns.
References
- Layden JE, Ghinai I, Pray I, Kimball A. pulmonary illness related to e-cigarette use in Illinois and Wisconsin- final report. N Engl J Med.2020;382(10):903-916. doi: 10.1056/NEJMoa1911614.
- Christiani DC. Vaping-induced acute lung injury. N Engl J Med.2020;382(10):960-962. doi:10.1056/NEJMe1912032.
- Maddock SD, Cirulis MM, Callahan SJ, et al. Pulmonary lipid-laden macrophages and vaping. N Engl J Med.2019;381(15):1488-1489. doi:10.1056/NEJMc1912038.
- Chasnoff IJ, Bussey ME, Savich R, Stack CM. Perinatal cerebral infarction and maternal cocaine use. J Pediatr. 1986;108(3):456-459. doi:10.1016/s0022-3476(86)80896-4.
- Bailey NA, Diaz-Barbosa N. Effect of maternal substance abuse on the fetus, neonate and child. Pediatr Rev. 2018;39(11):550-558. doi:10.1542/pir.2017-0201.
- Picciotto MR, Kenny PJ. Mechanisms of nicotine addiction. Cold Spring Harb Perspect Med.2021:11:a039610. doi:10.1101/cshperspect.a039610.
- Salas R, Sturm R, Boulter J, De Biasi M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J Neurosci.2009; 29:3014-3018. doi:10.1523/JNEUROSCI.4934-08.2009.
- Mc-Grath-Morrow SA, Gorzkowski J, Groner JA, et al. The effects of nicotine on development. Pediatrics.2020;145(3): e20191346. doi:10.1542/peds.2019-1346.
- Miech R, Johnston L, O’Malley PM, Bachman JG, Patrick ME. Trends in adolescent vaping, 2017-2019. N Engl J Med. 2019;381(15):1490‐1491. doi:10.1056/NEJMc1910739.
- Glasser AM, Johnson AL, Niaura RS, Abrams DB, Pearson JL. youth vaping and tobacco use in context in the United States: results from the 2018 National Youth Tobacco Survey. Nicotine Tob Res. 2021;23(3):447-453. doi:10.1093/ntr/ntaa010
11-year-old boy with testicular pain and rash
January 19th 2024An 11-year-old boy presented to the emergency department complaining of left testicular pain for 2 days, described as intermittent and stabbing, which ranged between 5 and 8 of 10 in intensity. Read the full case to see if you can correctly diagnose the patient.
Newborn with midline neck lesion
December 21st 2023A 4-day-old boy with a midline neck lesion was born at term by normal vaginal delivery. After birth, mid line lesion had the configuration of a linear cleft with a cephalocaudal orientation, extending from the level below the hyoid bone to the suprasternal notch with a length of 2.5 cm and a width of 0.5 cm. What's the diagnosis?
A 13-year-old girl with well-demarcated rash on back and chest
October 19th 2023A healthy 13-year-old girl presented with a 1-month history of an asymptomatic, well-demarcated rash on her back and upper chest. The eruption consisted of discrete, dark brown papules that coalesced into large, flat-topped plaques with mild superficial scale and accentuation of skin markings. What's the diagnosis?
Suspicious facial swelling in a 22-month-old girl
October 11th 2023A 22-month-old female patient with sickle cell disease on folic acid and penicillin prophylaxis with a 3-day history of nasal congestion, rhinorrhea, fever and decreased oral intake presents to the emergency department (ED) for acute facial swelling noted when she woke up from a nap. What's the diagnosis?
Friction-induced blistering on a child’s feet
July 14th 2023You are called to the hospital nursery to evaluate a healthy full-term newborn boy who developed painful flaccid blisters and erosions on the tops of his feet and ankles shortly after birth. His mother had a history of similar recurrent skin lesions that healed with scarring. She also had oral and gastrointestinal tract involvement. What's the diagnosis?