A case of shin guard dermatitis?
A healthy 14-year old boy was evaluated for an intensely pruritic shin rash that developed 2 weeks prior and had been treated with oral antibiotics for 10 days.
The case
A healthy 14-year old boy was evaluated for an intensely pruritic shin rash (Figure) that developed 2 weeks prior and had been treated with oral antibiotics for 10 days. On examination, the rash appeared more severe, with discrete, confluent, crusted, red papules and plaques on the shins, with relative sparing of the knees and ankles, progressing to the trunk and parts of the face and ears. He was upset because the rash interfered with his ability to play soccer.
Figure

Additional history taken from the patient’s father revealed that the boy was a goalkeeper on his school soccer team. The father explained that the inner lining of the boy’s protective shin guards was frayed. Owing to the initial location of the eruptions and lack of improvement on antibiotics, a diagnosis of allergic contact dermatitis due to a component of the shin guards was suspected. The dissemination of the rash was caused by autoeczematization. Patch testing to standard allergens and components of the patient’s soccer shin guards was planned.
Diagnosis: Shin guard allergic contact dermatitis to acetophenone azine now with generalized autoeczematization
Details of the diagnosis
Contact dermatitis is a common inflammatory skin condition characterized by erythematous, scaly, crusted, pruritic, and/or painful skin lesions after contact with a foreign substance. The condition can be irritant or allergic. Irritant contact dermatitis is caused by nonimmune-modulated chemical damage to the skin. Allergic contact dermatitis is a delayed hypersensitivity reaction (type 4) to contact antigens, and skin changes occur with reexposure.1
Autoeczematization, or id reaction, is a disseminated eczematous reaction that occurs when the antigen is released after exposure to a stimulus at a primary site, with the reaction spreading to distant sites.2
Differential diagnosis
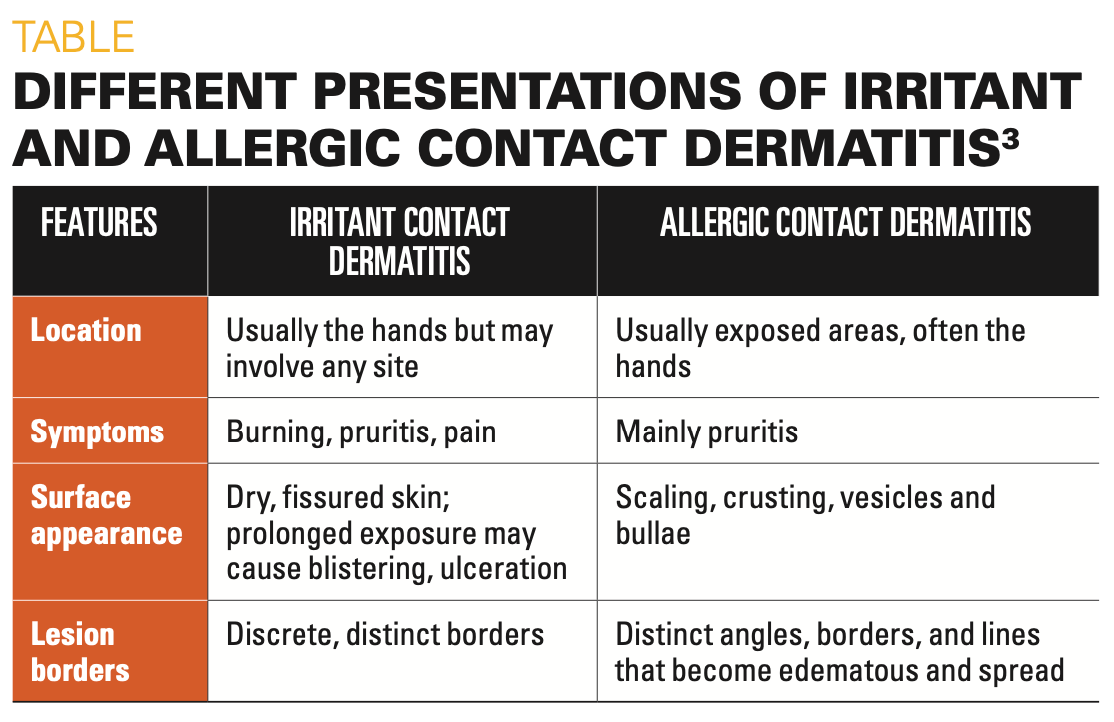
When determining the diagnosis, irritant contact dermatitis due to friction and sweat generally comes to mind first. However, the reaction is typical of allergic contact dermatitis, and this patient’s history favors the contact allergen acetophenone azine, a relatively new allergen, from his shin guards. The differential also includes atopic dermatitis, fungal infection, and psoriasis. The differences in the presentation of irritant and allergic contact dermatitis are summarized in the Table.3
Table
When must one suspect acetophenone azine contact dermatitis? The distribution of the primary rash and history of fraying shin guards should make this a high priority. Patch testing with a piece of the shin guard and the specific allergen, if available, should be considered and is recommended when avoiding the suspected allergen fails to bring improvement.
Management
Avoidance of the allergen is the mainstay of prevention of recurrent allergic contact dermatitis. In this case, using shin guards and shoes made of other materials and/or placing barriers between the skin and the shin guards can help treat the patient and confirm the diagnosis. Acetophenone azine is presently unavailable as a commercial patch-test preparation.
Cool compresses and calamine lotion can soothe the acute symptoms. Localized lesions are often successfully treated with mid- or high-potency topical steroids, such as triamcinolone 0.1% or clobetasol 0.05% applied twice a day for 2 to 3 weeks.4
If allergic contact dermatitis involves an extensive area of skin, the symptoms are extremely severe, or there is autoeczematization, systemic steroid therapy is often required and generally offers relief within 12 to 24 hours. If the allergen is removed and no effective therapy is instituted, it can take 2 to 3 weeks for the reaction to resolve, so an initial course of at least 5 to 7 days of prednisone, 0.5 to 1 mg/kg daily, is recommended. The dose may be tapered over the next 7 to 10 days.4
With severe dermatitis, oral prednisone should be tapered over 2 to 3 weeks with emollients and cool compresses with high-potency topical steroids applied to the worst areas. Emollients, moisturizers, or barrier creams are secondary treatment to help avoid continued exposure.4
What is known about acetophenone azine
A case report published in 2016 recognized the occurrence of severe, dramatic shin contact dermatitis in a young football player that progressed to generalized dermatitis.5 On further investigation and patch testing, acetophenone azine was found to be the culprit. High-performance liquid chromatography (HPLC) identified the chemical substance at concentrations of approximately 20 μg/g of shin pad samples. Patch tests gave strongly positive reactions to pieces of shin pads and to acetophenone azine down to dilutions of 0.001% in acetone.5
It was later recognized the potent new allergen caused rash even on exposure to footwear containing ethylene vinyl acetate (EVA).6 Acetophenone azine is not a component that is directly added to EVA during the manufacture of shin guards, shoe insoles, flip-flops, and other athletic gear and footwear. Though the exact chemical reactions that lead to its formation are unknown, it is presumed that it is due to cross-reactions with other materials added during EVA synthesis.5 Acetophenone azine may arise from the degradation of dicumyl peroxide and hydrazine in the foaming agent azodicarbonamide.6
On patch testing with materials including rubber, plastic, and shavings from the inner foam lining the shin guards, the only positive reaction was to the foam shavings that contained EVA. This material was sent to a laboratory, where HPLC revealed the allergen to be acetophenone azine.
Treatment and recovery
The antibiotic was continued for 4 more days, and oral prednisone at 1 mg/kg/day was added. He improved dramatically over the next 48 to 72 hours, at which point the antibiotics were discontinued. The prednisone was tapered over the next 10 days.
References
1. Usatine RP, Riojas M. Diagnosis and management of contact dermatitis. Am Fam Physician. 2010;82(3):249-255.
2. Bertoli MJ, Schwartz RA, Janniger CK. Autoeczematization: a strange id reaction of the skin. Cutis. 2021;108(3):163-166. doi:10.12788/cutis.0342
3. Usatine RP, Riojas M. Diagnosis and management of contact dermatitis. In: Usatine RP, Smith MA, Mayeaux EJ, Chumley H Jr, Tysinger J, eds. The Color Atlas of Family Medicine. McGraw-Hill; 2009:249-255.
4. American Academy of Allergy, Asthma and Immunology; American College of Allergy, Asthma and Immunology. Contact dermatitis: a practice parameter. Ann Allergy Asthma Immunol. 2006;97(3 suppl 2):S1-S38. Published correction appears in Ann Allergy Asthma Immunol. 2006;97(6):819.
5. Raison-Peyron N, Bergendorff O, Bourrain JL, Bruze M. Acetophenone azine: a new allergen responsible for severe contact dermatitis from shin pads. Contact Dermatitis. 2016;75(2):106-110. doi:10.1111/cod.12579
6. Raison-Peyron N, Bergendorff O, Du-Thanh A, Bourrain JL, Bruze M. Two new cases of severe allergic contact dermatitis caused by acetophenone azine. Contact Dermatitis. 2017;76(6):380-381. doi:10.1111/cod.12777
7. De Fré C, Bergendorff O, Raison-Peyron N, et al. Acetophenone azine: a new shoe allergen causing severe foot dermatitis. Contact Dermatitis. 2017;77(6):416-417. doi:10.1111/cod.12843
8. Darrigade AS, Raison-Peyron N, Courouge-Dorcier D, et al. The chemical acetophenone azine: an important cause of shin and foot dermatitis in children. J Eur Acad Dermatol Venereol. 2020;34:e61-e62. doi:10.1111/jdv.15911
9. Acetophenone azine: The 2021 American Contact Dermatitis Society Allergen of the Year. Cutis. 2021;107(5):238-240.doi:10.12788/cutis.0252
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.