A 2 ½-year-old with red spots
You are asked to evaluate a 2 ;½-year-old healthy boy with a 2-day history of a generalized asymptomatic skin eruption.
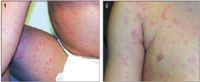
Diagnosis: Morbilliform reaction
Adverse drug reactions can be divided into immunologic and non-immunologic, and occur in approximately 6.7% of hospitalized patients.2 Only 6% to 10% of all drug reactions are immunologic in nature. Most of these are due to metabolites of drug.2 Amoxicillin is one of the more common drugs causing adverse reactions, both immunologic and nonimmunologic.2-4 The rash from a course of amoxicillin usually occurs within two weeks of initiation of the drug.4 The generalized symmetric lesions, which may involve the buccal mucosa, are usually pink to red, discrete macules and papules less than 1 cm in diameter.3,4 Lesions may become confluent and produce large erythematous patches and plaques. Drug fever and peripheral eosinophilia may accompany the eruption.3
Differential diagnosis
Atypical pityriasis rosea can present similarly, but the lesions are scaly. A morbilliform viral eruption and Kawasaki syndrome can also present similarly, but patients usually have other signs and symptoms (eg, fever, rhinorrhea, gastroenteritis, or adenopathy).4 Measles and rubella should be considered in nonimmunized children. Immunization reactions can result in similar lesions within three weeks of administration.
Secondary syphilis and allergic contact dermatitis may occasionally mimic a morbilliform eruption.3 Widespread blistering and/or erosions of the mucous membranes and skin preceded by a morbilliform eruption should suggest the possibility of Stevens-Johnson syndrome or toxic epidermal necrolysis.3
Management
The eruption usually resolves when the offending drug is discontinued.5 However, lesions may worsen before improving, and healing may not be complete for one to two weeks. There is no evidence to support the use of topical corticosteroids or oral antihistamines. Although patients may redevelop a similar rash on rechallenge,4 they are usually not at risk for an IgE-mediated hypersensitivity reaction.2
(Photos are for illustration purposes only and may not be of the patient described in the article.)
Please see Dr. Cohen's Web site, http://www.dermatlas.org/, for additional images
References
1. Barbaud AM, Bene MC, Schmutz JL, et al: Role of delayed cellular hypersensitivity and adhesion molecules in amoxicillin-induced morbilliform rashes. Arch Dermatol 1997;133:481
2. Boguniewicz M: Adverse reactions to drugs, in Behrman RE, Kliegman RM, Jenson HB (eds): Nelson Textbook of Pediatrics. ed 17. Philadelphia: Saunders, 2004, p 783
3. Fitzpatrick TB, Johnson RA, Wolff K, et al: Color Atlas & Synopsis of Clinical Dermatology: Common and Serious Diseases. 4th ed. New York: McGraw Hill, 200, p 1552
4. Breathnach SM: Drug Reactions, in Champion RH, Burton JL, Burns DA, et al (eds): Rook/Wilkinson/Ebling Textbook of Dermatology, Vol 4. ed 6. Malden, Mass: Blackwell Science, 1998, p 3368

The photograph included in the article, "Dermatology, What's Your Diagnosis: A persistent crusted plaque on the lower eyelid," May 2007, was described as being a photograph of a 17-year-old boy with HIV/AIDS. In fact, it was a photograph of a 34-year-old man with HIV/AIDS. The text of the article is otherwise accurate. The reader is reminded that cases presented in this column are published as teaching cases and may very well include in formation and photographs from an amalgam of cases.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.