Animal study reveals causes and consequences of how bone cells “age”
Premature cellular aging induced by glucocorticoids during puberty may cause children’s bone loss, osteoporosis, and fracture risk later in life.
Mei Wan, PhD
Glucocorticoid use
Research into the mechanisms underlying bone growth rate change in young mice is providing critical information on factors that affect bone growth and mineral accrual in children, including the profound effects of corticosteroid use on bone aging and fracture risk in children and young adults.1
“Adolescence is a critical period for optimizing bone growth and mineral accrual,” says Mei Wan, PhD, professor of Orthopaedic Surgery at Johns Hopkins University School of Medicine, Baltimore, Maryland. “During childhood, those with genetic bone disorders or chronic diseases have bone growth and mineral accrual that are often compromised and lead to bone loss, osteoporosis, and a high rate of bone fracturing.”
One such factor contributing to this loss of bone, osteoporosis, and bone fracturing in children is the use of glucocorticoids to treat chronic inflammatory childhood illnesses such as rheumatoid arthritis, Crohn disease, nephrotic syndrome, acute lymphoblastic leukemia, and rarer conditions such as muscular dystrophy.
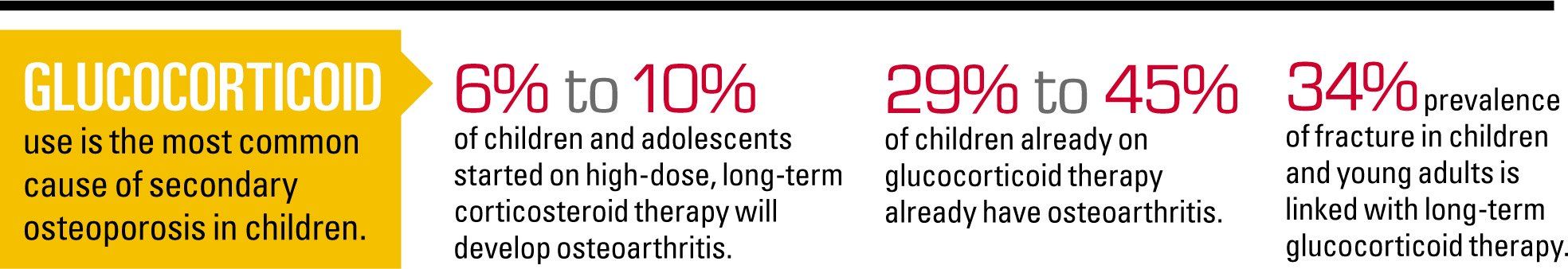
Glucocorticoid use is the most common cause of secondary osteoporosis in children, and Wan highlights that 6% to 10% of children and adolescents started on high-dose, long-term corticosteroid therapy will develop osteoarthritis, and between 29% to 45% of children already on glucocorticoid therapy already have it.2
In addition, she points out that epidemiologic data show that long-term glucocorticoid therapy is associated with a 34% prevalence of fracture in children and young adults.
“Even though it is known that glucocorticoids adversely affect the skeleton, I think sometimes pediatricians neglect focusing on the bones in children until there is a bone fracture,” says Wan. “For children who use long-term glucocorticoids, especially at high doses, they need guidance on bone health to offset the adverse effects of glucocorticoids.”
As the lead investigator of the study that looked at the mechanisms underlying bone growth and aging in young mice, Wan emphasizes that what she and her colleagues found sheds light on potential new therapies to treat secondary pediatric osteoporosis, for whom current therapies with frontline bisphosphonates are limited at best.
Mechanisms of bone growth change
Because of the importance of bone growth in adolescence on bone mass and strength, Wan and her colleagues at Johns Hopkins Medicine wanted to better understand the mechanisms underlying how bone cells change during adolescence and the regulatory mechanisms underlying these changes.
To do this, they focused on a region in long bones (legs and arms) that sits underneath the growth plate on either end of the long bone. Called the primary spongiosa, this region of rich bone precursor cells supports bone growth by containing the blood vessels and mesenchymal stem cells (MSCs) that mature into bone-forming osteoblasts.2
Building on what is already known about bone growth in adolescence-that is, long bones rapidly elongate during adolescence and taper off in later puberty primarily driven by the division of (or lack of) cartilage cells in the growth plate-they questioned whether the primary spongiosa contributed to changes in the growth rate of bones and mineral accrual.
To answer this question, the researchers looked for cellular senescence in the primary spongiosa in femurs of adolescent mice. Cellular senescence, or aging cells, is a mechanism that stops cellular division and is an important contributor to aging and age-related disease. Wan’s study suggests that cellular senescence may also be used by the body to control tissue growth.
The research team found that the number of senescence cells increased with the age of the mice, with mice in late puberty showing 3 to 4 times as many senescent cells compared with mice in early puberty.
Importantly, they found that the senescence of the bone precursor cells (or mesenchymal stem/progenitor cells in the area of the primary spongiosa) are controlled by epigenetic factors.“This is a very new finding,” says. Wan. “We found the novel cellular mechanism on how the precursor cells change in bone during adolescence and then we figured out the mechanisms that control that change.”
In addition to discovering the importance of cellular senescence in primary spongiosa as a marker for the transition from the rapid-growing phase to the slow-growing phase of long bones in mice, Wan and colleagues also identified a key protein in the cellular senescence in the primary spongiosa of long bones that is lost in late puberty. Called nestin, the protein is needed for self-renewal, proliferation, and cell cycle progression of the cells. Wan and colleagues found that deletion of a key marker (Ezh2) in nestin-expressing cells during early puberty increases the risk of osteoporosis in later adulthood.
“This suggests that premature cellular senescence in the primary spongiosa region during the prepubertal or early pubertal phase may also be a major cause of osteoporosis/bone loss in later life,” state the authors in the conclusion of their study.1
Importantly, one of the variables that can induce premature cellular senescence in the primary spongiosa region is the use of glucocorticoids.
Better therapies on the horizon
What this research points to is a new direction for treating bone loss in children induced by glucocorticoid therapy. According to Wan, she and her researchers are now looking at the efficacy of an anabolic drug to stimulate bone formation. Findings so far show that use of an epigenetic inhibitor in mice has led to increased bone mass with no obvious adverse effects. Currently, the inhibitor is used to treat malignant brain tumors in young large animals.
To date, Wan and her colleagues are working toward submitting their preliminary findings of whether this anabolic agent can prevent or reduce the adverse effects of glucocorticoids on bones. Further study will then be needed in large animals to see its full potential use for preclinical and clinical trials, she says.“The message of our work is that pediatricians should be aware that the use of an anabolic drug to stimulate bone formation is more ideal to treat pediatric osteoporosis [than the current frontline therapy with bisphosphonates],” she says.
References:
1. Li C, Chai Y, Wang L, et al. Programmed cell senescence in skeleton during late puberty. Nat Commun. 2017;8(1):1312. Available at https://www.nature.com/articles/s41467-017-01509-0. Accessed March 23, 2018.
2. Johns Hopkins Medicine. Link found between pediatric osteoporosis and anti-inflammatory drugs [press release]. Available at: https://www.hopkinsmedicine.org/news/media/releases/link_found_between_pediatric_osteoporosis_and_anti_inflammatory_drugs. Published March 6, 2018. Accessed March 23, 2018.