Beating bad breath
Bad breath is no laughing matter for the child or adolescent who has it. Most cases can be alleviated by relatively simple measures, but not before the cause is pinpointed by a targeted history and physical exam.
Beating bad breath
By Mel Rosenberg, PhD, Gary Robinson, MBChB, and Erica Amir, DMD
Bad breath is no laughing matter for the child or adolescent who has it. Most cases can be alleviated by relatively simple measures, but not before the cause is pinpointed by a targeted history and physical exam.
A 3-year-old brought in for an office visit has a terrible odor emanating from all over his body. Where do you begin your examination?
A 17-year-old complains of very bad breath, but neither you nor her parents can smell anything. What's wrong?
A 14-year-old tells you that he coughs up whitish "stones" that smell awful. What are they?
Although bad breath is rarely the primary presenting complaint in pediatric practice, it's not unusual for it to be mentioned during the consultation. Bad breath is a symptom of any number of conditions, from poor dental hygiene to sinusitis, and it can have serious social consequences for the affected child. Kids pull no punches, and a child with bad breath is often ridiculed by peers.
Sometimes referred to as halitosis, fetor oris, fetor ex ore, or oral malodor, bad breath is any detectable, offensive smell carried on the breath. One of the most frustrating aspects of this condition is not being able to tell whether or not one actually has it.1,2 Children and adults who do have halitosis are usually unaware of the problem unless alerted by others. At the other extreme, some teenagers (and adults) develop halitophobiaan exaggerated fear that they have bad breath when, in fact, they have only mild malodor or none at all. This fear may be accompanied by social withdrawal, depression, and even thoughts of suicide.3 Because halitophobics do not always voice their worries in this regard, this phobia can be particularly insidious.
There are many types of bad breath, including the rare fishy odor that accompanies trimethylaminuria.1,4 The large majority of cases encountered by the pediatrician, however, involve odor that comes from the teeth, gums, tongue, nose, or tonsils.3
Children of almost any age can have halitosiswe have detected bad breath in patients as young as 2 years. The prevalence of bad breath increases with age and may be as high as 65% among adults.5 The prevalence of severe halitophobia in the general population is reported to be 0.5% to 1% (Stein M: Personal communication, May 1999).
This article aims to throw light on the subject of bad breath. The information presented is based on available studies (most of them performed on adults) and our clinical and research experience.
A bacterial basis
Almost 70 years ago, Grapp showed that bad breath in adults often comes from the far back region of the dorsum of the tongue.6 We postulated several years ago that this is largely due to the accumulation of postnasal drip on the back of the tongue.3,5 That is probably also true in most cases of bad breath in otherwise healthy children. Unless there is frank nasal infection, postnasal drip does not smell immediately upon reaching the tongue; it becomes putrid upon degradation of the mucus by copious bacteria on the far back reaches of the dorsum.3
As a child gets older, more dental plaque accumulates on the teeth, and the likelihood of bad breath coming primarily from subgingival and interdental sites increases.7 As with bad breath caused by postnasal drip, bad breath from dental sites involves bacterial activity.
Bacteria in the mouth degrade proteins there, yielding amino acids that are further degraded and produce odorous volatile gases. The breakdown of methionine and cysteine yields, respectively, hydrogen sulfide and methylmercaptangases both implicated in bad breath.8 Other products of amino acid breakdown, such as indole and skatole (products of the breakdown of tryptophan) and cadaverine (a product of the breakdown of lysine), may contribute to oral malodor.9 Because the various kinds of bad breath are quite different in character (nasal odor differs from interdental odor, for example), dozens of types of molecules are likely involved.
Gram-negative anaerobic proteolytic bacteria (such as Porphyromonas gingivalis, Fusobacterium nucleatum, Prevotella intermedia, and spirochetes) have been implicated as a cause of oral malodor.10 These microorganisms are thought to cause periodontal disease in adults, and studies have shown a correlation between bad breath and periodontal disease.11 A child may harbor these microorganisms interdentally, on the dorsum of the tongue, and in the throat.
Primary causes of bad breath
The most common causes of halitosis involve the mouth, nose, and throat.
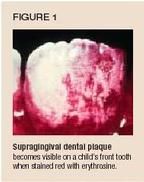
Dental conditions that contribute to malodor include not only dental plaque but also impacted food, advanced dental decay (food can get trapped and putrefy), and inflamed gingivae. The most common of these is dental plaque, which can accumulate on both the readily visible buccal (Figure 1) and lingual surfaces and between the teeth.
The connection between dental health and breath underscores how important it is for children to receive regular, professional dental care and to faithfully follow a rigorous oral hygiene regimen at homeone that includes brushing the teeth at least twice daily. More detailed recommendations for dental-related bad breath are discussed in the section on treatment.
Postnasal drip, whether transient or chronic, is common in children, and, as noted, is probably the leading cause of bad breath. In a study of 52 children with chronic sinusitis,12 90% were considered to suffer from purulent nasal discharge and 63% from postnasal drip. Sixty-seven percent of the children were judged to have bad breath. Postnasal drip may also help account for the oral malodor that accompanies chronic rhinitis in young children. In the case of allergic rhinitis, "allergic salute" (nose rubbing) and "allergic shiners" (swollen, inflamed, ecchymotic eyelids) may be present.
The odor of postnasal drip is detected most strongly from a child's mouth, and can often be reproduced by taking a sample (with, say, a small spoon) from the very posterior region of the dorsum (Figure 2). Wait a few seconds, and then smell the contents of the spoon.

About one in three healthy children harbors the nasal microorganism Staphylococcus aureus on the tongue.13 And, a recent study of bad breath in healthy children found that odor from the back of the tongue (judged by sampling material taken from the lingual dorsum with a plastic spoon) was indeed associated with both oral and nasal odor.7 These data, taken together, suggest that the mouth-nose bad breath association may be even more pronounced in children than in adults, possibly because of the close anatomic connection between the nose and oral cavity (Figure 3).

Breathing through the mouth rather than the noseas when the nose is congestedis a risk factor for bad breath in people of all ages (see the discussion of saliva, below). Adenoidal hypertrophy, a common problem in childhood that may lead to mouth breathing, may present with chronic intermittent purulent or watery rhi- nitis, snoring, dry mouth, and bad breath.
Nasal passages are the second most common source of bad breath after the mouth, accounting for about 5% to 10% of cases of bad breath in adults.14,15 Typical nasal malodor has a slightly cheesy character and differs appreciably from other types of bad breath. It is easy to distinguish from oral malodor because most of the odor exits the nose rather than the mouth.5
Odor from the nose may indicate a frank nasal infection, such as sinusitis, or a problem affecting airflow or mucous secretions, such as polyps. In some cases, a craniofacial anomaly, such as cleft palate, may be involved.16
Nasal odor often comes and goes for no apparent reason. In a study of 24 healthy children examined over three appointments,7 nine had nasal odor at one appointment, eight at two appointments, and one at all three appointments. Only six children had no nasal odor at any of the appointments!
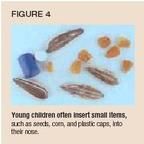
Nasal foreign bodies. Very young children tend to stick things in their nose.17 These objects can be almost anything that fits in the nostrils: food (corn, peas, sunflower seeds, beans), pieces of tissue, tacks, small toys, buttons, and outdoor objects (parts of plants and even small animals such as snails) (Figure 4). If the foreign body is absorbent, it putrefies relatively quickly, and the child often smears the ensuing purulent exudate over his skin and hair. This can give the physician the mistaken impression that the odor is coming from all over the child's body (as is likely the case with the 3-year-old in the opening scenario).
If the foreign body is hard and impervious to moisture, it does not readily putrefy and can remain undetected for a long time. We once traced a case of mild nasal odor to a calcified plastic bead embedded in the nose of a 28-year-old woman who had apparently placed it there some 25 years earlier!3
On rare occasions, children may ingest a foreign body that then gets caught in the upper gastrointestinal tract, resulting in halitosis. In addition, any obstruction of the nasal passages that leads to mouth breathing will likely increase oral malodor.
Tonsils. The role of tonsils in chronic malodor in children is unclear. In adults, tonsils have been estimated to cause about 3% of cases of bad breath, although some ear, nose, and throat specialists believe tonsils play an even greater role than this figure indicates. Parents commonly report a transient oral malodor with the onset of sore throat in their children, an odor that can be sensed by the attending physician as well.5,18 Transient bad breath following tonsillectomy has also been reported. Clearly, further investigation is necessary to assess the role of tonsils in pediatric oral malodor.
Tonsilloliths. Some patients complain of small, foul-smelling stones on their tongue or tonsils when they cough. These stones are "tonsilloliths"partially calcified deposits of bacteria and debris that originate in crypts of the tonsils (Figure 5).

Based on our experience, we estimate that about 3% of the adult population have, or have had, tonsilloliths. Despite their foul odor, tonsilloliths do not necessarily cause bad breath. But because people often squeeze the stones between their fingers and become horrified by the smell, tonsilloliths may lead to halitophobia.
The formation of these deposits can be prevented by laser cryptolysis, which seals the crypts. This is not a common clinical procedure, however.5,16
Saliva contains antibacterial agents and continually washes away bacteria from oral surfaces. When the mouth dries out, odor increases, not only because of increased proliferation of bacteria but also because gases escape into the air when the liquid dries. Bad breath gets worse during the day when saliva flow is lowestseveral hours following a meal, for exampleand at night, when the flow of saliva is negligible. Factors that dry out the mouth, such as mouth breathing, certain medications, prolonged talking, lack of sufficient fluid intake, and stress, increase the likelihood of bad breath.
The breakdown of proteins in the oral cavity that leads to malodor usually takes place under neutral or alkaline conditions. Therefore, acidity in the mouth probably reduces oral malodor; on the down side, it promotes dental caries.5
Diet. Surprisingly little is known about the relationship between diet and breath, particularly in children. Since most cases of malodor involve proteolysis, one might surmise that proteinaceous foods can cause bad breath, particularly if they remain in the mouth a long time after eating (as with impacted meat between teeth). Investigators have suggested that milk products and coffee can lead to bad breath, although this hypothesis has not been clinically investigated. Foods containing garlic and onion can, of course, cause bad breath following ingestion. Although some of this odor enters the bloodstream and percolates out through the lungs, most of the odor is related to the oral cavity. In a recent experiment at Tel Aviv University, students were instructed to either chew and swallow a sandwich containing garlic or chew the sandwich and spit it out. No difference in odor level was found between the two regimens. Furthermore, odor exiting the mouth was consistently stronger than odor exiting the nose (Hoffman D, Greenstein R: Unpublished data, June 2000).
Since oral malodor is generally worst in the morning, eating a good breakfast can help reduce bad breath. The increased saliva flow, together with the mechanical action of chewing and swallowing, helps lower oral microbial levels and, in turn, decrease odor.
Interestingly, researchers have found elevated levels of bad breath in hyperactive children, who also had other possible predisposing factors such as allergy and stuffy nose.19 In one study,20 24 children who had attention deficit hyperactivity disorder were fed a special diet (Alberta Children's Hospital Diet; "ACH") that eliminated food dyes, food flavors, preservatives, monosodium glutamate, chocolate, and caffeine; reduced the amount of simple sugars; and provided multivitamin supplements. The diet resulted in a significant reduction in bad breath (P <.01) and a less significant reduction in rhinitis (P = .07).
People who diet or fast often complain of bad breath. It is unclear whether their bad breath is caused by ensuing changes in the oral cavity (the mouth drying out or lack of mastication) or by altered body metabolism.
Among those who have the rare genetic condition trimethylaminuria ("fish odor syndrome"), diets high in choline can result in self-perceived fishlike breath and body odor caused by buildup of trimethylamine in sweat, saliva, and urine.4
Tobacco. People have long smoked cigarettes to mask their bad breath, a practice that results in its own unpleasant odor. Cigarette odor can linger for more than a day. In some cases, the odor of cigarette smoke can be detected on the breath of people who don't smoke but who are continually exposed to the smoke of others.5
In the United States, the use of smokeless tobacco has been cited as an important cause of bad breath in adolescents. 21 Indeed, tobacco-use prevention programs should emphasize the risk of bad breath as a deterrent to smoking.
Menstruation. In postpubertal girls, bad breath may occur during the menstrual cycle. This may be caused by transient gingivitis.22
Illness. Many illnesses have been reported to cause bad breath, including untreated diabetes, bronchial and lung infections, kidney or liver failure, various carcinomas, metabolic dysfunction, and biochemical disorders. These are rare causes in the ambulatory population, however, and are usually accompanied by more obvious symptoms.1,23
In the case of diabetes, older literature on bad breath often cites ketone (acetone) odor as a sign of the disease. In modern societies, ketone odor is rare among diabetics whose disease is well managed (Hollenberg C: Personal communication, May 1990). In less developed countries, in indigent populations, and among diabetic teenagers away from home (who might binge on pizzas and other taboo foods then), ketone odor may still be a telltale sign of diabetes.
The stomach. Contrary to popular belief, bad breath almost never arises from the esophagus, stomach, or intestines. The esophagus is normally collapsed and closed; an occasional belch may carry odor up from the stomach, but the possibility of air escaping continuously is remote. Nevertheless, several gastroenterologists have proposed a relationship between Helicobacter pylori and bad breath, a hypothesis that requires further study. In general, performing gastroscopy solely because of bad breath should be strongly discouraged.17 Reports in the literature of cases of bad breath related to gastric conditions, such as congenital hypertrophic pyloric stenosis, are rare.24
Arriving at a diagnosis
When evaluating bad breath, the input of a confidantsomeone close to the patient who is aware of the problemis invaluable. The confidantusually a parent, older sibling, close friend, or relative is often the person who has complained about the patient's bad breath. He (or she) should be present at the consultation for several reasons:
- Bad breath is often a subjective complaint. People who complain they have bad breath are notoriously incompetent at judging their own malodor. Similarly, parents who complain about their child's bad breath may be exaggerating the problem. At the office appointment, the physician should verify the objective nature of the problem and the complaint.
- The confidant can attest to whether the odor present at consultation represents, in both intensity and character, the odor of the breath at other times. Bad breath varies with the time of day (saliva flow), day of month (menstruation), weather (allergies), and so on.
- Patients are usually unaware of changes in their breath. The confidant can help monitor the situation, report any changes, and build confidence that the situation is improving (which it hopefully is).
Patients should refrain from any oral activity, including eating, drinking, chewing, smoking, or brushing, for at least three hours before the appointment. Reschedule patients who are either on antibiotics or who have taken them during the past month; because malodor is often bacterial in origin, it usually decreases transiently during and directly after antibiotic therapy.
History. Begin the evaluation with a medical history. Concentrate on finding out whether the patient maintains good oral hygiene, is a mouth breather, and has any history of allergy or nasal problems. Ask the confidant where he thinks the odor is coming from and why. Two scenarios that may be encountered during history taking are:
- "Our daughter Judy (5 years old) has bad breath, especially when she wakes up in the morning and sometimes in the late afternoon. Her older brother and sister never had this problem."
- "Nobody has actually told me I have bad breath, but I know I do because people cover their mouths when they talk to me." (Or: people open windows in my presence; people touch their nose when talking to me; I have a bad taste in my mouth; my father had bad breath.)
That second group of answers is typical of halitophobics, who are often well groomed and commonly break into tears during the patient history. They frequently need psychological intervention but tend to resist it, convinced that their problem is organic.16,25
Physical examination. Although several manufacturers are developing "electronic noses" to analyze bad breath, no instrument is as yet able to replace the human nose. So clinicians must still rely upon their sense of smell to distinguish the main types of oral odors, summarized in Table 1. With practice and experience, these odors become distinct and recognizable, even when found in various combinations.
TABLE 1
What's that smell?
Ask the patient to breathe out through the mouth. Smell the odor from about 5 to 10 cm away and make a quantitative judgment (for example, on a scale of 0 to 5, where 0 is no odor, 1 is barely detectable odor, 2 is slight odor, 3 is moderate odor, 4 is foul odor, and 5 is is unbearably foul odor). Also make qualitative judgments (for example, typical/atypical, periodontal/ lingual). When simple breathing through the mouth is inadequate to make an assessment, ask the patient to count out loud to 20 while you evaluate his breath; sometimes the odor is more obvious when speaking. In children younger than 4 years or so, simply lean toward them and smell the expirate.
After evaluating mouth odor, ask the patient to breathe out through the nose with the mouth closed. We often ask young children to pretend they are an elephant and to breathe out through their "trunk." Assess as above.
Based on your assessment findings:
- Suspect an oral or pharyngeal origin to the bad breath when the odor is largely confined to the mouth.
- Suspect nasal involvement when the odor is largely confined to the nose or has a different character than the oral odor.
- Suspect a systemic origin in those rare cases when odor emanates both from the mouth and nose and has the same quality.
Evaluate the tongue by asking the patient to stick it out as far as possible while holding his breath. Use the spoon to scoop up some of the mucus at the very back of the dorsum of the tongue, toward the throat. In older children, you can hold the tip of the tongue with a piece of gauze in one hand and collect the sample with the spoon in the other hand. Wait a few seconds before smelling the spoon and scoring the odor. Ask the confidant to smell the spoon and tell you whether this is the odor the patient suffers from. (If it is, gentle tongue cleaning and gargling should resolve the problem.)
Sulfide monitors. The level of intraoral volatile sulfur compounds (VSC) produced by oral bacteria can be estimated using a portable sulfide monitor (Figure 6). Readings are obtained by inserting a plastic straw attached to the monitor into the patient's partially closed mouth and asking the patient to breath normally through the nose while the instrument sucks the air through the sensor.

The association between sulfide monitor results and odor judgment scores is significant (coefficient correlations in studies range from about 0.45 to 0.65, P <.001) and relatively reproducible.26 Sulfide monitor readings are sensitive to a reduction in mouth odor level following use of a rinse. Nevertheless, although these measurements can be helpful (such as to apprise the patient of any improvements in breath odor), they do not obviate the need for the clinician to smell the breath emanating from the patient's mouth, nose, and tongue.
Additional clinical and laboratory tests for measuring VSC and other bad breath-associated parameters are under development. For example, oral isolates can be plated onto selective agar that indicates by color those colonies that produce VSC. Our laboratory is working on a rapid color test to identify the presence of high levels of bacterial activity associated with the production of malodor.
Treating the problem
Most cases of bad breath can be alleviated by relatively simple measures (Table 2), such as maintaining proper dental care and oral hygiene. Encourage older children to floss their teeth, to smell the floss between each passage, and to clean the malodorous sites carefully. The ability to manipulate the floss depends largely on eye-hand coordination and age; children younger than about 8 or 9 years are usually not able to floss on their own. Time and supervision are needed to ensure that flossing is done properly.27
TABLE 2
Measures for alleviating bad breath
Maintaining proper dental care and oral hygiene
Gently cleaning the posterior portion of the tongue
Rinsing and gargling with an effective mouthwash
Eating (particularly fibrous foods) or chewing gum briefly
Drinking enough liquid to keep the mouth from drying out
Treating relevant medical conditions
Similarly, the ability to brush one's teeth depends on the motor development of the small muscles of the hand. The parent should brush the child's teeth until the child can brush efficiently on his own, which is usually the case by school age. Young children should use fluoridated toothpaste but in only a pea-sized amount; this is to avoid dental fluorosis that could result from inadvertently swallowing toothpaste.
The back portion of the dorsum of the tongue can be gently cleaned with a tongue cleaner or with a spoon or small toothbrush. Dozens of different kinds of tongue cleaners are available; patients should be able to find one that feels comfortable (Figure 7). Patients should avoid using brittle plastic tongue cleaners that might break. Because the odor comes from the posterior region of the tongue, the patient must clean all the way back. The goal is to sweep forward the mucus, desquamated cells, and other debris. Make sure the patient does not traumatize the tongue in the process. Also, practice is necessary to overcome the gag reflex.

If mechanical cleansing does not reduce odor sufficiently, rinsing and gargling with mouthwash can be advised for children older than about 6 years. Younger children are more likely to accidentally ingest mouthwash. (Mouthwashes can poison children when ingested and should be kept out of reach of toddlers. Also, be aware that some mouthwashes contain componentssuch as alcohol, sodium dodecyl sulfate, and strong oxidizing agentsthat may harm soft oral tissues.) Many dentists recommend fluoride mouth rinses, which may have some antimalodor activity. Advise patients to get the liquid as far back as possible without swallowing it; one way is to extend the tongue while gargling.
It is particularly important that children with physical disability or psychomotor retardation (cerebral palsy, for example) have an annual dental exam. During these visits, the clinician should provide appropriate instruction to parents or health providers in the techniques of oral health maintenance as well as dental treatment. If necessary, dental therapy may have to be done under general anesthesia.
Carefully monitor the oral hygiene of children who are unable to maintain personal oral health. Consider bad breath in mentally retarded children an important potential sign of oral and, in turn, general neglect. Children wearing orthodontic appliances are also more likely to have difficulty maintaining oral hygiene, so carefully monitor these patients' oral health too.
Children with acute or subacute rhinitis and halitosis do not typically need therapy, because halitosis usually disappears once the rhinitis resolves. Chronic rhinitis with postnasal drip and halitosis presents a more challenging therapeutic problem. Suspect chronic sinusitis in such cases, particularly if additional symptoms of headache, frequent nocturnal coughing, malaise, fatigue, or low-grade fever are present. The diagnosis may be made clinically or with the aid of plain radiographs or computed tomography scans of the sinuses. Attempt to rule out disorders that predispose to chronic rhinitis or sinusitis (Table 3), especially in children with severe, recurrent episodes. A broad spectrum antibiotic, particularly one of those effective against ß-lactamase producing organisms and anaerobes, should be administered for at least three weeks, followed by a second three-week course if symptoms do not resolve. An intranasal corticosteroid spray may also be tried to relieve chronic nasal mucosal inflammation and improve sinonasal drainage. Antihistamines may be helpful only in patients who have predisposing allergic disease.
TABLE 3
Detecting chronic rhinitis and sinusitis
Adenoidectomy may be indicated for chronic sinusitis when medical therapy has failed, particularly if signs of upper airway obstruction are present.28 Deviated septum, nasal polyps, and nasal tumor may require surgical treatment as well. A foreign body should be removed immediately once detected. It should be emphasized that halitosis without significant associated symptoms is not an indication for surgery.
Other treatment recommendations include briefly eating (particularly fibrous foods) or chewing gum, and drinking enough liquids to keep the mouth moist.
Because most cases of bad breath are caused by microbial activity, physicians and parents may notice a transient improvement in bad breath after a course of an antibiotic (for whatever problem). Nevertheless, prescribing antibiotics solely for bad breath is inadvisable.
The need for vigilance
Bad breath isn't life-threatening, but it does cause extreme embarrassment in children and can be a sign of poor oral health. In most cases, the source of the problem can be readily identified. Because the large majority of cases are amenable to treatment, pediatricians should be on the lookout for halitosis in their patients.
REFERENCES
1. Attia EL, Marshall KG: Halitosis. Can Med Assoc J 1982;126:1281
2. Rosenberg M, Kozlovsky A, Gelernter I, et al: Self estimation of oral malodor. J Dent Res 1995;74:1577
3. Rosenberg M, Leib E: Experiences of an Israeli malodor clinic, in M Rosenberg (ed): Bad Breath: Research Perspectives. Ramot Publishing, Tel Aviv University, 1995, pp 137148
4. Ayesh R, Mitchell SC, Zhang A, et al: The fish odour syndrome: Biochemical, familial and clinical aspects. BMJ 1993;307:655
5. Rosenberg M: Clinical assessment of bad breath: Current concepts. J Am Dent Assoc 1996;127:475
6. Grapp GL: Fetor oris (halitosia). A medical and dental responsibility. Northwest Med 1933;32:375
7. Amir E, Shimonov R, Rosenberg M: Halitosis in children. J Pediatrics 1999;134:338
8. Tonzetich J, Richter VJ: Evaluation of volatile odoriferous components of saliva. Arch Oral Biol 1964;9:39
9. Goldberg S, Kozlovsky A, Gordon D, Gelernter I, Sintov A, Rosenberg M: Cadaverine as a putative component of oral malodor. J Dent Res 1994;3:1168
10. Persson S, Claesson R, Carlsson J: The capacity of subgingival microbiotas to produce volatile sulfur compounds in human serum. Oral Microbiol Immunol 1989;4:169
11. Kozlovsky A, Gordon D, Gelernter I, Loesche WJ, Rosenberg M: Correlation between the BANA test and oral malodor parameters. J Dent Res 1994;73:1036
12. Parsons DS, Phillips SE: Functional endoscopic surgery in children: A retrospective analysis of results. Laryngoscope 1993;103:899
13. Miyake Y, Iwai T, Sugai M, et al: Incidence and characterization of Staphylococcus aureus from the tongues of children. J Dent Res 1991;70:1045
14. Delanghe G, Ghyselen J, van Steenberghe D, et al: Multidisciplinary breath-odour clinic. Lancet 1997; 350:187
15. Rosenberg M: Introduction, in M Rosenberg (ed): Bad Breath: Research Perspectives, Ramot Publishing, Tel Aviv University, 1995
16. Finkelstein Y: The otolaryngologist and the patient with halitosis, in M Rosenberg (ed): Bad Breath: Research Perspectives. Ramot Publishing, Tel Aviv University, 1995
17. Katz HP, Katz JR, Bernstein M, et al: Unusual presentation of nasal foreign bodies in children. JAMA 1979;241:1496
18. Nakar S, Kahan E, Weingarten M: Can you smell the strep? The Lancet, 1994;343:729
19. Kaplan BJ, McNicol J, Conte RA, et al: Physical signs and symptoms in preschool-age hyperactive and normal children. J Dev Behav Pediatr 1987;8:305
20. Kaplan BJ, McNicol J, Conte RA, et al: Dietary replacement in preschool-aged hyperactive boys. Pediatrics 1989;83:7
21. Christen AG, McDonald JL Jr, Olson BL, et al: Smokeless tobacco addiction: A threat to the oral and systemic health of the child and adolescent. Pediatrician 1989;16:170
22. Lee WC, Sharp JF: Complications of paediatric tonsillectomy post-discharge. J Laryngol Otol 1996; 110:136
23. Tonzetich J, Preti G, Huggins GR: Changes in concentration of volatile sulphur compounds of mouth air during the menstrual cycle. J Int Med Res 1978;6:245
24. Madarikan BA, Rees BI: Halitosis and gastric outlet obstruction in infants. Br J Clin Pract 1990;44:419
25. Eli I, Baht R, Kozlovsky A, Rosenberg M: The complaint of oral malodor: Possible psychopathologic aspects. Psychosomatic Medicine 1996;58:156
26. Rosenberg M, Kulkarni GV, Bosy A, et al: Reproducibility and sensitivity of oral malodour measurements with a portable sulphide monitor. J Dent Res 1991; 70:1436
27. Wei SHY: Mechanical and chemical plaque control, in Pediatric Dentistry: Total Patient Care. Lea & Febiger, 1988
28. Pizzuto MP, Volk MS, Kingston LM: Common topics in pediatric otolaryngology. Pediatric Clinics of North America 1998;45:973
DR. ROSENBERG is professor of microbiology, department of oral biology, the Maurice and Gabriela Goldschleger School of Dental Medicine, Tel-Aviv University, Tel Aviv, Israel. He developed the application in the Interscan sulfide monitor (discussed in this article) that measures bad breathassociated volatile sulfides.
DR. ROBINSON is clinical pediatrician, Ramat-Aviv Child Health Centre, Kupat Holim Clalit, Israel.
DR. AMIR is senior teacher in pediatric dentistry, the Maurice and Gabriela Goldschleger School of Dental Medicine, Tel-Aviv University.
Oral malodor through the ages
Bad breath as a social problem has been around for thousands of years. Ancient writings on halitosis date to the Egyptian Ebers papyrus, Roman manuscripts, and Jewish Talmud. In the days of the Jewish temple, priests were not allowed to perform holy tasks if they had bad breath. The Koran of Islam stresses fresh breath in the context of good oral hygiene.1
Many ancient folk remedies for bad breath are still in use. For centuries, Iraqis have chewed clove, moving it around the mouth to prevent burning. Inhabitants of Mediterranean countries commonly chewed gum mastic before the advent of modern chewing gum. These folk cures are not without scientific merit, as both clove and mastic gum have potent antibacterial components. Other folk cures include mint (commonly used in commercial toothpastes and mouth rinses even though it has only weak antimalodor activity), parsley (used in Italy), guava peels (Thailand), and even eggshells (China).1
More recent literature on bad breath dates to a monograph published by Howe in the late 19th century,2 and experimental research on the subject dates back more than 60 years. Among investigations that examined bad breath in children, studies on upper respiratory tract infections and tonsillectomies predominate.36
REFERENCES
1. Rosenberg M: Clinical assessment of bad breath: Current concepts. J Am Dent Assoc 1996;127:475
2. Howe JW: The Breath and The Diseases Which Give It a Fetid Odor, ed 4, New York, D. Appleton and Co, 1898
3. Parsons DS, Phillips SE: Functional endoscopic surgery in children: A retrospective analysis of results. Laryngoscope 1993;103:899
4. Rosenfeld RM: Pilot study of outcomes in pediatric rhinosinusitis. Arch Otolaryngol Head Neck Surg 1995;121:729
5. Telian SA, Handler SD, Fleisher GR, et al: The effect of antibiotic therapy on recovery after tonsillectomy in children. Arch Otolaryngol Head Neck Surg 1986;112:610
6. Lee WC, Sharp JF: Complications of paediatric tonsillectomy post-discharge. J Laryngol Otol 1996;110:136
Mel Rosenberg, Gary Robinson, Erica Amir. Beating bad breath.
Contemporary Pediatrics
2002;3:139.
Infant RSV hospitalization rates 28%, 43% lower this season vs pre-COVID seasons
May 9th 2025"These findings support Advisory Committee on Immunization Practices’ recommendations for maternal vaccination or nirsevimab to protect against severe RSV disease in infants," wrote the MMWR study investigators.