Biological terrorism and warfare: Not sci-fi any longer
When otitis and toilet training were at the top of parents& worry list, pediatricians knew how to respond. Today, parents want to know how to keep children safe from terrorists with biological weapons, and pediatricians have no ready answers. This review should make you better informed.
Biological terrorism and warfare:
Not sci-fi any longer
By J. Thomas Cross, Jr., MD, MPH
When otitis and toilet training were at the top of parents' worry list, pediatricians knew how to respond. Today, parents want to know how to keep children safe from terrorists with biological weapons, and pediatricians have no ready answers. This historical perspective and summary of what's known about the most likely bacterial and viral weapons should make you better informed.
In 1932, when Aldous Huxley was looking for an image sufficiently appalling to explain why a war-weary society had accepted the scientific Utopia of his Brave New World, he described "the explosion of anthrax bombs, hardly louder than the popping of a paper bag." In the 70 years since Huxley's classic novel was published, the silent, annihilating weapon became a staple of science fiction, a titillating image that gave audiences a satisfying frisson of horror. On October 5, when the first case of pulmonary anthrax in many years was diagnosed in a Florida man, fiction became reality. In the weeks since, Americans have come to the realization that an unknown enemy is spreading anthrax bacteria, not from the air, as Huxley imagined, but through the mail.
The anthrax attack is not a discrete event, but one that continues to unfold as this article is being written. By the end of November, the Centers for Disease Control and Prevention (CDC) were reporting 23 cases of anthrax (18 confirmed and five suspected). Of these 23, 11 have been diagnosed as inhalational anthrax, the rest as the less deadly cutaneous form of the disease that responds well to antibiotic therapy. Six of the patients with inhalational anthrax are recovering.1 Five have died. Thousands of people who might have been exposed are receiving prophylactic antibiotics. Federal offices and postal facilities where anthrax spores were found were shuttered while decontamination procedures were carried out.
To public health professionals, this is a trifling outbreaknot worth speaking of in the same breath with prevalent, deadly diseases like AIDS, malaria, or influenza. Anthrax, if detected early enough, is treatable, unlike some forms of highly resistant tuberculosis or viral diseases like Ebola. It is not contagious. A vaccine exists. And yet, the attack is terrifying, as it was meant to be. The information presented here may make it less so. And the historical narrative that runs concurrently may surprise you with, first, just how far back the antecedents of this terrorist strike go and, second, how busy an industry biological weaponry has been in the past 100 years.
What we know: A biological warfare primer
Physicians responding to public concern about biological warfare are in the uncomfortable position of having to make pronouncements on the basis of limited knowledge. Public health officials are feeling their way, andas the delayed response to the dangers faced by postal workers indicatedare not always prepared with adequate answers. Pediatricians will need to review the literature and keep up with new publications and educational programs as they are produced. (See "Resources for pediatricians" for leads on where to look for information.) With that caveat, here is what we know now.
Resources for pediatricians
Reference
Committee on Infectious Diseases, American Academy of Pediatrics: Red Book 2000. Elk Grove Village, IL, AAP, 2000. Table 2.2, p 85, provides a list of recommended diagnostic procedures, isolation guidelines, and treatment protocols for children in the event of a biological attack.
Updates
www.hopkins-biodefense.orgThe Johns Hopkins Center for Civilian Biodefense Studies
www.aap.orgThe American Academy of Pediatrics
www.bt.cdc.orgThe biological terrorism site of the Centers for Disease Control and Prevention
www.idsociety.orgThe Infectious Disease Society of America
www.asm.org
The American Society of Microbiology
www.cdc.govCDC: Update: Investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy, November 2001. MMWR 2001; 50(45):1008
Biological weapons: Disease reviews
Arnon SS, Schechter R, Inglesby TV, et al: Botulinum toxin as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 2001;285:1059
Dennis DT, Inglesby TV, Henderson DA, et al: Tularemia as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 2001;285:2763
Henderson DA, Inglesby TV, Bartlett JG, et al: Smallpox as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 1999;281 (22):2127
Inglesby TV, Henderson DA, Bartlett JG, et al: Anthrax as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 1999;281(18):1735
The first question to ask is which pathogens are of concern in such a discussion. Of the thousands known to cause disease, a fairly limited number make the list of agents that are:
- easy to produce
- easy to disperse
- able to inflict severe disease on a community or nation.
The CDC strategic planning group lists the agents in Table 1 as "high-priority" agents of concern.16 The big four on this list, say most experts, are smallpox, anthrax, botulism, and plague. According to Donald A. Henderson, MD, MPH, of the Center for Civilian Biodefense Studies at Johns Hopkins University, bioweapons research has indicated that the problems of producing and dispersing enough of the latter two are virtually insurmountable so that "...smallpox and anthrax are virtually alone at the top of the list among potential agents."17 What follows is a summary of current knowledge on how to recognize and treat all four of these diseases when they occur and how to protect the general population from infection.
TABLE 1
Biological terrorism: Most likely suspects
Variola major (causes smallpox)
Bacillus anthracis (anthrax)
Yersinia pestis (plague)
Clostridium botulinum toxin (botulism)
Francisella tularensis (tularemia)
Filoviruses
Ebola hemorrhagic fever
Marburg hemorrhagic fever
Arenaviruses
Lassa (Lassa fever)
Junin (Argentine hemorrhagic fever)
Adapted from MMWR 200016
Smallpox
When infectious smallpox virus makes contact with mucous membranes, individuals contract the disease. The incubation period is 10 to 14 days, making "silent" dissemination easy. Initially, patients present with an influenza-like illness with high fever and pain. Two to three days later small papules develop over the face and spread to the extremities. Vesiculation then occurs. Pustules form on Day 7 or 8 and scab at about Day 12. In past eras, when populations were not vaccinated, an estimated 25% to 30% of those who contracted smallpox died of the infection.
In a triumph of global public health efforts, the disease had been eradicated worldwide by 1977. In the United States, smallpox vaccination was halted in 1972. Research cultures of the virus were locked up in two places, a CDC laboratory in Atlanta and in the Soviet Union. American clinicians have never seen a case, a blessing thatin a situation of biological warfaremay turn out to be a considerable liability.
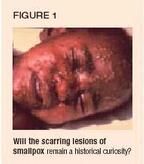
A physician who has never seen an actual smallpox lesion can easily confuse it with chickenpox, especially during the first few days of infection (Figure 1). Whereas smallpox lesions develop at the same stage simultaneously (all papules, then all vesicles, and so on) and appear identical, chickenpox lesions appear in crops, are more dense over the trunk, and rarely involve the palms and soles. Smallpox is most dense on the face and extremities, including palms and soles, and the lesions are deeper and tougher to break than chickenpox lesions. There is no antiviral treatment for smallpox, although some animal and tissue culture data suggest that cidofovir may be of some use if taken soon after exposure.
Vaccination before or within two or three days after exposure affords almost complete protection against disease. Vaccination as late as four or five days after exposure may prevent death. At this time, however, no one in this country is protected. American children have not been vaccinated in decades, and even people old enough to have been vaccinated in childhood are not immune because the smallpox vaccine may not provide protective immunity beyond 10 or 20 years.
Smallpox is quite contagious and, once introduced as a bioweapon, would spread quickly. Even when the US population was well vaccinated, isolated caseslike that of a Canadian child who contracted smallpox in Brazil and traveled through New York State on his way home to Toronto in 1962provoked panicky reactions and proposals for extreme protective measures. (In fact, proposed mass vaccinations were never carried out and no cases of contagion were recorded.)
If smallpox were used in biological warfare, the weapon would likely be an aerosolized form of the virus. We have no real-world or experimental data on how effective this might be. However, we should consider a 1970 incident in Germany, in which a patient returning from Pakistan was hospitalized with an initial diagnosis of typhoid fever.18 By the time smallpox was diagnosed and the patient transferred to an isolation hospital, 19 peoplemany of them not even on the same floor of the hospital as the patientwere infected. One was a visitor who had spent fewer than 15 minutes in the hospital to open a corridor door, 30 feet from the patient's room, and ask directions. By the time this incident was over, patients and staff had been quarantined for four weeks and more than 100,000 people had been vaccinated.
We cannot know for certain how a bioterrorist attack using smallpox would unfold, but the following scenario postulated by Henderson and colleagues of the Working Group on Civilian Biodefense is worth serious consideration11:
"A small aerosol of smallpox virus is released into a crowded area. The infection is silent in the incubation phase until nine to 10 days later when a rash develops. Initially, physicians would see a case or two of an unusual 'viral exanthem' and dismiss the initial cases as 'atypical chicken pox or some other unusual virus syndrome.' Several days would pass before a correct diagnosis of smallpox is made. Let's assume in a community of 250,000 that 100 persons became infected and required hospitalization. We know that many more will become ill and receive an uncertain diagnosis of 'viral exanthem.' Likely this community has inadequate respiratory isolation for the 100 already infected. Few hospital staff have immunity. Contacts of confirmed cases would likely number tens of thousands."
In the event of an actual attack, the keys to diminishing the spread of smallpox will be to isolate cases and their contacts and administer vaccine as quickly as possible. Isolating contacts is not as daunting as it might appear. Smallpox patients are not contagious until the rash appears (unlike chickenpox and measles where virus is released before the rash appears). So following an attack, all patients with fever (or any possible exposure) could be quarantined at home until it was clear whether they had smallpox. A consensus statement recommends considering home care in a mass attack because isolation in the hospital requires negative pressure isolation with exhaust filters, which are few and far between.19
Pediatricians who suspect a mass exposure can play a key role in identifying sentinel cases and notifying local and state authorities. The key component, however, is recognizing that a biological agent has been identified in the community and then moving quickly to isolate those who may be at risk of spreading the infection.
Mass vaccination, unlike isolation, presents a serious problem. Smallpox vaccine has not been manufactured since the mid-1980s. Parents asking about vaccination for their children will have to be told that existing stocks held by the CDC are not available to civilians. Even if they were, the quantity in storage is considered inadequate to control an outbreak of the sort under discussion here. Furthermore, that vaccine was made by an outmoded process that involves infecting animals. This process is now considered too prone to contamination to be acceptable.
The federal government has entered a contract with a biotechnology company to make a vaccine with tissue culture methods. The goal, as announced by the US Secretary of Health and Human Services, is to accelerate the manufacturing process and to stockpile 300 million doses of the new vaccine, enough to protect every American if that should be necessary. But no matter how rapidly manufacturing and clinical testing proceeds, the fact remains that, at this time, an acceptable vaccine in sufficient supply is not available.
The pediatrician's role, and it is crucial, is to be part of the early warning system, identifying sentinel cases that raise the possibility of a mass attack and activating an appropriate public health response. To do that effectively, pediatricians and pediatric residents will need to be educated in recognizing smallpox and in appropriate modes of containment.
Anthrax
Until October, veterinarians were the only health-care professionals with much awareness of anthrax, although it was known to be an occupational hazard for those who work with cattle. Even though students of biological warfare placed it very high on the list of potential agents, knowledge of the symptoms and course of anthrax infection in humans was limited.20 The last known outbreak in the US occurred in the 1950s, in some New Hampshire mill workers who contracted the disease from the goat hair they processed. Moreover, much of what infectious disease specialists thought they knew, before the current outbreak, is turning out to be less solid than they supposed. At this moment, the uncertainties include the amount of spores necessary to produce infection, risk factors that could predict susceptibility, how the current outbreak is spreading, whether cross contamination is possible, what prophylactic and therapeutic agents should be recommended, andmost puzzlingwhere and by whom the agent is being manufactured.
The causative agent, Bacillus anthracis, is an aerobic, Gram-positive, spore-forming species of Bacillus. Anthrax spores can live in the earth for indefinite periods but are believed to be readily killed by exposure to sunlight and can be eradicated by the application of bleach. Laboratory identification of the organism takes several days, and few US laboratories have experience identifying it. We saw the disastrous effects of this delay in diagnosis early in the current outbreak, although the situation seems to be improving.
Humans can contract anthrax by one of three routes:
- intestinal anthrax, from ingesting spores
- cutaneous anthrax, when a cut or scrape in the skin allows entry by the bacillus
- inhalation anthrax, when the spores are inhaled.
So far, no cases of intestinal anthrax have been seen in this outbreak, although some bioterrorism experts are very worried about this possibility. Cutaneous anthrax has occurred as an occupational disease in workers engaged in processing animal hair or hides, and about half the cases in the current outbreak are of this type. Cutaneous anthrax usually responds well to antibiotic therapy. Inhalation anthrax, however, is highly lethal. The five deaths that have been recorded thus far in this attack have been attributed to the inhalational form of the disease.
Anthrax is easy to produce in large quantities and extremely stable in dried form. In the Sverdlovsk accident described in the box below, people within 4 km south and east of the facility were affected. Reports show that about 100 people became symptomatic and 66 died. Patients became ill within a week to as late as six weeks after exposure. Death followed one to four days after onset of illness. Penicillin prophylaxis and vaccination were reportedly helpful in stemming the tide of this epidemic, but little hard information was made available by the Soviet authorities.21
The current, apparently mail-disseminated outbreak, has generated much fear but few victims. In one expert group's scenario for airborne anthrax dissemination, 50 kg of aerosolized anthrax dispensed 2 km upwind from a population of 100,000 in ideal meteorologic conditions could kill 33,000 people.22
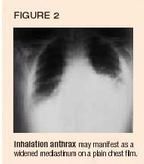
In the current situation, within a few days of exposure to spores carried through the mail, patients presented to primary care physicians with high fever and difficulty breathing. They reported a nonspecific, flu-like illness with malaise, myalgia, and a nonproductive cough.23 A second phase then occurred, marked by rapid deterioration with continuing high fever, dyspnea, cyanosis, and shock. The only unusual manifestation of the disease process is the appearance of a widened mediastinum on chest radiograph (Figure 2). Skin biopsies or sputum samples (in the case of inhalational disease) will show Gram-positive bacilli.
The anthrax bacillus is susceptible to antibiotic therapy. Even resistant forms developed in laboratories here and in the former USSR respond to ciprofloxacin and a number of other antibiotics. Supplies of ciprofloxacin are limited, the cost is high (though lowered recently through negotiation between the manufacturer and the federal government), and the possibility of inducing resistance by massive prophylactic use of the drug has become a serious concern. For all these reasons, the CDC has changed its recommendation for initial treatment to include doxycycline as an alternative to ciprofloxacin. After initial treatment, if the organism is not shown to be resistant, a switch to a more common antibiotic is now recommended. Appropriate antibiotic therapy is thought to be lifesaving for exposed patients in the early stages of respiratory illness.
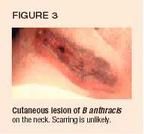
Cutaneous manifestations are generally easier to diagnose, and physicians are learning what the lesion looks like. Henderson describes an initially pruritic macule or papule that enlarges into a round ulcer by the second day. Vesicles may appear subsequently and discharge fluid containing numerous organisms visible on Gram stain. The black eschar shown in Figure 3 then develops. The lesion is painless and often associated with extensive local edema. The eschar dries, loosens, and falls off in the next few weeks. It does not usually leave a scar.19
While antibiotic therapy does not appear to change the course of the cutaneous illness, it is thought to decrease the likelihood of systemic disease. With the use of antibiotics, death from cutaneous anthrax is rare. The CDC is continually updating its guidelines for antibiotic therapy of both inhalational and cutaneous anthrax as the current crisis unfolds.1
As with smallpox, a vaccine that protects against infection with anthrax exists but is not currently available. Supplies are held entirely by the armed forces and are not given to civilians, even those like postal workers who appear to be at high risk of exposure. The vaccine is unwieldy, requiring a course of six shots followed by yearly boosters. Further, the manufacturer was forced to cease production several years ago because of problems with contamination, and although the federal government has contracted with a different manufacturer to produce new stocks of a better vaccine, those have not yet materialized.
Plague
Yersinia pestis, the organism that causes plague, is third on most lists of potential biologic weapons. The more familiar form of the disease, bubonic plague, has a reservoir in animals, usually rodents, and is transmitted to humans by flea bites. The classic presentation of bubonic plague involves development of lymphadenopathy in the form of buboes usually found in the groin or neck. During World War II, Japan is said to have dropped fleas infected with plague over populated areas of China, causing outbreaks.24
If plague were used as a biologic weapon today, it would most likely be dispersed in an aerosolized form that would produce the pneumonic form of the disease. According to the World Health Organization, 50 g of Yersinia pestis, dispersed in an aerosol over a city of 5 million residents, would result in 150,000 cases of pneumonic plague and 36,000 deaths. Two to four days after exposure, people would develop early symptoms of fever, cough, dyspnea, and production of bloody or watery sputum. Gastrointestinal symptoms might also be present. The disease could spread from those initially infected by means of respiratory droplets.
Early diagnosis would require a high index of suspicion, responding to a sudden outbreak of illness presenting as severe pneumonia and sepsis. Tetracycline or doxycycline has been recommended by the Working Group on Civilian Biodefense for treatment of diagnosed cases and prophylaxis of those known to be exposed. No vaccine is currently available in the US.
Botulism
The fourth biological agent with the characteristics that would make a likely weapon is botulinum toxin, the single most poisonous toxin known. A single gram of crystalline toxin, evenly dispersed and inhaled, would kill more than 1 million people.25 No such attack has been recorded, although in the aftermath of the Gulf War the government of Iraq admitted producing the toxin and loading it into bombs. The concentrated toxin produced by Iraq has not been fully accounted for and constitutes approximately three times the amount needed to kill the entire current human population by inhalation. Research in the use of the botulinum toxin as a weapon has also been carried out, at one time or another, by the governments of Japan, the former USSR, and the United States.
Clostridium botulinum, the causative agent, is a spore-forming anaerobe living naturally in the soil. It is not contagious, although Soviet research into the production of microbes intentionally modified to produce botulinum toxin has been reported, and such microbes could be contagious. Natural botulism is caused by ingestion of contaminated food. It is a rare disease; a median number of 26 cases per year occur in this country. Laboratory diagnosis is fairly lengthy. Clinical diagnosis is based on the presence of the following triad:
- symmetric, descending flaccid paralysis with prominent bulbar palsies
- occuring in an afebrile patient with
- a clear sensorium.
Unfortunately, the diagnosis is often missed by physicians who confuse the symptoms with those of Guillain-Barré syndrome or diseases of the central nervous system.
According to the Working Group on Civilian Biodefense, the following features of an outbreak of botulism would suggest a bioterrorist attack:
- large numbers of cases of acute flaccid paralysis with prominent bulbar palsies
- toxin type not usually seen in a natural outbreak
- common geographic factor without a common dietary exposure
- multiple simultaneous outbreaks with no common source.
Therapy includes prompt treatment with equine antitoxin and supportive care that is likely to include weeks or even months of assisted ventilation. Limited availability of antitoxin and limited critical care and mechanical ventilator capacity severely limit our current ability to respond to a mass attack.
What is to be done?
A bioterrorist attack on the US is no longer a theoretical possibility. It is today's reality, and very possibly tomorrow's. Much of the response is a matter for government action, and we can all see in the daily news what measures government is taking. What can the individual pediatrician contribute to this effort?
First, we need to include bioterrorism in the differential for unusual presentations or multiple cases of any unusual disease. Table 2 lists indications of a possible biowarfare attack.26 It makes sense to consider the possibility of an attack whenever a cluster of patients presents with similar but unusual signs and a natural cause is not evident or when a common disease occurs in much higher numbers than usual or leads to a high morbidity and mortality rate in healthy people.
TABLE 2
Early indicators of possible biowarfare attack
Disease is unusual for geographic area
Multiple diseases seen in a single patient
Large numbers of civilian and military casualties
Data indicating massive point-source attack (large numbers of victims from a single event or area)
Apparent aerosol route of infection
High morbidity and mortality relative to the number of personnel at risk (unexpectedly high rate of serious illness or death relative to small number of people exposed)
Illness limited to fairly localized geographic area
Low attack rate among those who work in areas with filtered air supply
Sentinel dead animals of multiple species
Absence of a natural vector in the area of outbreak
In any such situation, do not wait until you are sure of the diagnosis; contact your local health department and law enforcement agency immediately. Pediatricians should be part of a community effort to set up response plans for biological attack, working with local schools and child-care facilities. They will have a key role in identifying sentinel cases, raising their index of suspicion when unexplained clusters of illness appear. Most states are now setting up contingency plans and means to address these issues systematically. Most involve utilizing local health departments, police departments, fire departments, and National Guard units, as well as federal agencies such as the CDC and FBI.
Pediatricians should be aware that the release of biological agents would affect children disproportionately, for physiologic and developmental reasons. Children are at higher risk physiologically because of their increased respiratory rate, increased skin permeability, and the likelihood of receiving a higher inoculum per kilogram of body weight in an attack. Developmentally, children are less capable of avoiding exposure and more vulnerable to emotional stress. Because pediatricians know children's needs best, they should be part of planning for dealing with biological attack. Last, pediatricians and pediatric residents must be educated in effective response to the medical and disaster-management aspects of a biological attack.15
References
1. Centers for Disease Control and Prevention: Update: Investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy, October 2001. MMWR October 26,2001;50(42):909
2. Poupard JA, Miller LA: History of biological warfare: Catapults to capsomeres. Ann NY Acad Sci 1992;666:9
3. Robertson AG, Robertson LJ: From asps to allegations: Biological warfare in history. Mil Med 1995;160:369
4. Christopher GW, Cieslak TJ, Pavlin JA, et al: Biological warfare: A historical perspective. JAMA 1997;278:412
5. Harris S: Japanese biological warfare research on humans: A case study of microbiology and ethics. Ann NY Acad Sci 1992;666:21
6. Harris R, Paxman JA: A Higher Form of Killing. New York, Hill and Wang, 1982, pp 79
7. Manchee RJ, Braster MG, Melling J, et al: Bacillus anthracis on Gruinard Island. Nature 1981;294:254
8. Mobley, JA: Biological warfare in the twentieth century: Lessons from the past, challenges for the future. Mil Med 1995;160(11):547
9. Mills J, Drew D: Serratia marcescens endocarditis: A regional illness associated with intravenous drug abuse. Ann Intern Med 1976;84:203
10. Zalinskas RA: Iraq's biological weapons: The past as future? JAMA 1997;278:418
11. Henderson DA: Bioterrorism as a public health threat. Emerg Infect Dis 1998;4:488
12. Miller J, Broad WJ: The germ warriors: A special report. The New York Times, December 8, 1998
13. Torok TJ, Tauxe RV, Wise RP, et al : A large community outbreak of salmonellosis caused by intentional contamination of restaurant salad bars. JAMA 1997;278:389
14. Cole LA: The specter of biological weapons. Scientific American December 1996;275(6):60
15. American Academy of Pediatrics: Chemical-biological terrorism and its impact on children: A subject review. Pediatrics 2000;105:662
16. Centers for Disease Control and Prevention: Biological and chemical terrorism: Strategic plan for preparedness and response. MMWR 2000;49(RR-4):1
17. Henderson DA: The looming threat of bioterrorism. Science 1999;283:1279
18. Wehrle PF, Posch J, Richter KH, et al: An airborne outbreak of smallpox in a German hospital and its significance with respect to other recent outbreaks in Europe. Bull World Health Organ 1970;4:669
19. Henderson DA, Inglesby TV, Bartlett JG, et al: Smallpox as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 1999; 281:2127
20. Inglesby TV, Henderson DA, Bartlett JG, et al: Anthrax as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 1999; 281:1735
21. Meselson M, Guillemin V, Hugh-Jones M, et al: The Sverdlovsk anthrax outbreak of 1979. Science 1994; 266:1202
22. Kaufmann AF, Meltzer MI, Schmid GP: The economic impact of a bioterrorist attack: Are prevention and postattack intervention programs justifiable? Emerg Infect Dis 1997;3:83
23. Pile JC, Malone JD, Eitzen EE, Friedlander AM: Anthrax as a potential biological warfare agent. Arch Intern Med 1998;158:429
24. Inglesby TV, Dennis DT, Henderson DA, et al: Plague as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 2000;283:2281
25. Arnon SS, Schechter R, Inglesby TV, et al: Botulinum toxin as a biological weapon: Medical and public health management. Working Group on Civilian Biodefense. JAMA 2001; 285:1059
26. Wiener SL, Barrett J: Biological warfare defense, in Trauma Management for Civilian and Military Physicians. Philadelphia, WB Saunders,1986, pp 508509
THE AUTHOR is associate professor, departments of internal medicine and pediatrics, Louisiana State University Health Sciences Center, Shreveport, La.
A short history of biological warfare
One reason for the disproportionate fear this outbreak has inspired is its apparent uniqueness. Deliberately infecting one's enemies as a means of warfare is, most Americans think, something new under the sun. Not so. Biological warfare has a long, long history.
From antiquity to the 12th century.According to Poupard and Miller, historians of biological warfare, the first recorded instance of such warfare was perpetrated by the ancient Greeks.2 As long ago as 300 BC, contamination of the enemy's wells with the bodies of dead animals was part of Greek military campaigns. Since antiquity, the tactic has been refined. In the 12th century, Frederick Barbarossa used the rotting corpses of dead soldiers as well as animals to pollute wells. A higher-tech version was employed during the Renaissance; in the siege of Carolstein in 1422, the attacking army used catapults to propel diseased bodies into walled fortifications.
This era of corpses, pollution, and catapults was followed, in the 18th century, by a period that Poupard and Miller call the era of specific disease application. They cite the case of the French and Indian war, in which the British were fighting to preserve their North American colony's boundaries against attack by French troops and their Indian allies. In the spring of 1763, one Colonel Henry Bouquet, the ranking British officer on the Pennsylvania frontier, wrote to Sir Jeffrey Amherst, the British commander-in-chief, describing the siege of Fort Pitt and noting an outbreak of smallpox in the garrison. In reply, Amherst suggested, "Could it not be Contrived to Send the Small Pox among those Disaffected Tribes of Indians?" Bouquet wrote back, "I will try to inoculate the ____________ with Some Blankets that may fall in their Hands, and take care not to get the disease myself."
Significantly, Bouquet added this postscript himself, in different ink. It is possible he did not want to alert his clerk to the plan, and official copies of the letter would not have contained the added note. Drawing a line instead of naming the Indians may have been an additional precaution. Amherst apparently approved the plan, noting in his response: "You will Do well to try to Inoculate the Indians, by means of Blankets, as well as Try Every other Methode, that can Serve to Extirpate this Execrable Race."
World War I and the Geneva Protocol.In succeeding centuries, the developing science of bacteriology expanded the scope of potential biological warfare agents. Evidence exists that Germany used glanders and anthrax to infect horses and cattle, respectively, in Bucharest in 1916 and employed similar tactics to infect 4,500 mules in Mesopotamia the next year.3 Although no large-scale battlefield use of biological weapons occurred in World War I, numerous allegations were made in the years following the war. Britain accused Germany of dropping plague bombs, and the French claimed the Germans had dropped disease-laden toys and candy in Romania. Germany denied the accusations.
General awareness of the potential of biological weapons led delegates to the Geneva Convention to include biological agents in the 1925 Protocol for the Prohibition of the Use in War of Asphyxiating Poisonous or Other Gases, and of Bacteriological Methods of Warfare.4 The Geneva Protocol, as it has come to be known, banned the use of biological and chemical agents in war but did not address the issues of research, development, production, or stockpiling of these agents. While most nations ratified and signed the treaty, it was the subject of bitter debate in the United States, and was withdrawn from the Senate agenda by President Truman in 1947. Congress did not ratify the treaty until 1975.
Revving up for World War II.In 1929, the Union of Soviet Socialist Republics opened a biological warfare research facility north of the Caspian Sea. In the 1930s, both Japan and the United Kingdom initiated biological warfare research programs. The Japanese program was developed and run by Dr. (Major) Shiro Ishii, whose rationale was that biological weapons must be effective or the Geneva Protocol would not have banned them. In 1932, Dr. Ishii established a laboratory in Manchuria called the Zhong Ma Camp. Human testing at Zhong Ma involved plague, cholera, glanders, and typhus.
In 1936, Dr. Ishii was appointed Chief of the Kwantung Army's Water Purification Units. These units, known to number at least 18, were all involved in biological warfare research. By the end of the war, they had studied the effects on humans of virtually every known pathogen, chemical pesticide, and plant or animal poison. During the years of Japanese biological weapon research more than 10,000 human subjects were involved, all of whom either died or were killed.5 A small group of human remains studied by American researchers in 1947 showed that anthrax accounted for 31 deaths; cholera, 50; dysentery, 12; glanders, 20; mustard gas, 16; tetanus, 14; plague, 106; salmonella, 11; tuberculosis, 41; typhoid, 22; and typhus, 9.6 At least 12 large-scale field tests (cholera, typhoid, anthrax, typhus, plague) were carried out in China.
After the war, many of the Japanese scientists went into the academic world. More than 5,000 Japanese were tried as war criminals, but not one high-level Japanese biological warfare expert was ever charged with a crime.
Preparations for biological warfare were not limited to the Axis powers. Between 1937 and 1940, Britain began to stockpile vaccines, fungicides, and insecticides against biological attack. The British biological warfare laboratory was established in 1940 at Porton Down. In the summer of 1942, scientists from Porton tested a bomb filled with anthrax spores in Gruinard, a small island off the northwest coast of Scotland, against lines of tethered sheep. In 1943, a bomber was used to scatter spores over the island. The Gruinard tests proved that biological warfare was feasible. A total of 4 x 1014 spores were released in these tests.7 The island was still contaminated with anthrax spores in 1979. It was finally decontaminated in 1987.
In 1941, the British Secret Service, in conjunction with the Special Operations Executive and a group representing Czech exiles in Great Britain, decided to have Reinhard Heydrich (Hitler's choice as his successor) killed. On May 23, 1942, in Prague, Heydrich was attacked with a grenade filled with botulinum toxin. He died on June 4 with classic symptoms of botulism.8
That same year, the US and Canada joined Britain in a joint program of biological warfare research and development. Camp Detrick, Md., became operational as the center of biological weapons research in 1943. In the winter of 1943, the Allies began to manufacture a biological bomb; it weighed four pounds and was filled with anthrax spores. The bomb was given the code name "N." In May 1944, an initial batch of 5,000 anthrax bombs came off the production line at Fort Detrick. The facility could produce 50,000 bombs per month. The main center for US production was built at Vigo, Ind. It was capable of producing 500,000 anthrax or 250,000 botulism-filled bombs a month. After the war, the Vigo facility was leased for the production of antibiotics.8
In time of peace. Following World War II, biological warfare experimentation continued at a rapid clip. The diseases considered most suitable as weapons were anthrax, brucellosis, tularemia, psittacosis, Q fever, and Venezuelan equine encephalitis. In the 20 years following World War II, more than 200 experiments using surrogate markers for biological warfare agents were conducted in the US against military and civilian targets. One such experiment occurred in September 1950, when two Navy minesweepers released a purportedly harmless aerosol of Bacillus globigii and Serratia marcescens outside San Francisco's Golden Gate Bridge. Six mock attacks took place over a six-day period. One hundred seventeen square miles were exposed, and nearly every one of the 800,000 people of San Francisco inhaled more than 5,000 particles. In the years that followed, cases of endocarditis caused by Serratia developed in intravenous drug users in the exposure area. However, it has not been confirmed that the strains were similar.9
In 1966, supposedly harmless Bacillus subtilis bacteria were released through gratings in the roofs of the New York subway tunnels in a field trial to demonstrate how quickly biological agents could spread. Within minutes, the turbulence caused by speeding trains in the system's tunnels carried organisms throughout the system.
Despite these successful field trials, by 1969 the US military had concluded that biological warfare had little strategic value on the battlefield. In an age of nuclear weapons, defense experts believed, its impact would be insignificant. On November 25, 1969, President Richard Nixon announced that the US would unilaterally renounce biological warfare and eliminate stockpiles of biological weapons. Once military leaders had discounted the value of biological weapons, it became possible to persuade other countries to go out of the biological warfare business. In 1972, the Convention on the Prohibition of Development, Production, and Stockpiling of Bacteriological (Biological) and Toxic Weapons and on Their Destruction was signed by 140 nations, including the US and the entire Warsaw Pact membership.
The current era. For all practical purposes, biological warfare was not a "front-burner" issue again until the Persian Gulf War (19901991). After the war, Iraq confirmed that it had produced, filled, and deployed bombs, rockets, and aircraft spray tanks containing Bacillus anthracis and botulinum toxin.10 Iraq's biological warfare work force and technologic infrastructure remain wholly intact to this day.
What remains of the former Soviet Union is also ground for considerable worry. The Soviet investment in biological warfare was extensive. The 1979 accidental release of anthrax spores from a military facility in Sverdlovsk that resulted in 79 cases of infection and 68 deaths has provided US researchers with what little they now know about the pathophysiology of pulmonary anthrax in humans.
In the early 1990s, the USSR maintained a large, sophisticated bioweapons facility known as Vector.11 Vector was a 30-building facility employing more than 4,000 people and housing both specimens and human cases of disease that reportedly included smallpox, Ebola, and Marburg viruses. At that time the facility was protected by electric fences and an elite guard. When Vector was revisited in 1997, after the collapse of the Soviet Union, observers found a half-empty facility, a handful of guards who had not been paid in months, and no sign of the scientists. At that time, Vector was thought to be the only storage site for smallpox outside the CDC.
The biologic agents once kept at Vector, and the scientists who worked with those agents, could be used by terrorist groups or so-called rogue states for biological warfare. According to a special report published in the New York Times in 1998, the Iranian government is known to have approached top Russian germ warfare researchers with offers to work for Iran, and some Russians are said to have accepted the invitation.12
In recent years, interest in biological weapons has not been limited to governments. Aum Shinrikyo, the Japanese cult known for releasing the nerve gas sarin in the Tokyo subway in 1995, had plans for biological terrorism as well. Large quantities of nutrient media, botulinum toxin, anthrax cultures, and aircraft with spray tanks were found in the cult's compound. Members of the group had reportedly traveled to Zaire in 1992 to obtain Ebola virus samples for possible use as a weapon. In 1984, in Oregon, followers of a cult leader, Bhagwan Shree Rajneesh, deliberately contaminated restaurant salad bars, leading to 751 cases of salmonella poisoning.13
Individuals acting alone also can be bioterrorists, like Larry Harris, a lab technician from Ohio who ordered samples of Yersinia pestis from a Maryland biomedical supply firm in 1995. He drew suspicion only because he called the firm four days later to complain that he hadn't received his order yet. Harris, who was found to be a member of a white supremacist group, needed only a credit card and false letterhead to place the order. He claimed he wanted to counteract Iraqi rats carrying "supergerms."14
Concern with domestic terrorism following the Oklahoma City bombing in 1996 prompted Congress to pass legislation providing the federal government with a broad range of investigative, prosecutory, and regulatory powers dealing with biological, chemical, and other weapons. On April 15, 1997, the CDC's new regulations governing hazardous biological agents went into effect. Those regulations have four major goals:
- identification of biological agents that could be hazardous to the public
- creation of procedures for monitoring these agents
- implementation of safeguards for transport of these agents
- development of a system to alert authorities when attempts are made to acquire restricted agents.
In pursuit of these goals, the 1996 Defense Against Weapons of Mass Destruction Act envisioned a unified system under which the Federal Bureau of Investigation and the Federal Emergency Management Agency took the lead in responding to a biological attack. These two agencies were to work closely with other federal agencies and the US Public Health Service in activating the National Disaster Medical System.15 In April of this year, the CDC published a "Strategic Plan for Preparedness and Response" to biological and chemical terrorism, outlining the recommendations of a strategic planning workgroup for reducing US vulnerability to biological and chemical terrorism.16 The current emergency is the first real-world trial of the system.
Bio-anxiety puts a pediatric ED on alert
The reality of bioterrorism has hit close to home at our institution, the A. I. du Pont Hospital for Children, and its emergency department. Even in a relatively small city like Wilmington, Del., news of anthrax and the threat of other potential pathogens and toxins is real and powerful; we are, after all, within the Megalopolis, not that far from New York or Washington, D.C. (In fairness, every ED in the country, no doubt, feels threatened the way we do.) To date during this terrorist strike, only one child has been infected with Bacillus anthracis, but the potential for more cases is real. As a government official said recently, however, now is the time to be alert, not alarmed.
At our hospital, the ED is under pressure to "be prepared" to be the front line, to identify cases of infection or toxicity caused by bioterrorism, and to make decisions about initial management and appropriate referrals. ED staffphysicians and nursesare eager to learn more about conditions we gave little attention to in the past. Many arrive early for work, or stay late, to hear an update on anthrax or other agents of biowarfare and bioterrorism. Whether the message is delivered by a local speaker or satellite feed, interest remains high. Physicians are passing the latest articles from the literature and Web site addresses to each other as if they were a valued treasure.
Town meetings are taking place in many medical settings; our hospital is no different. At our recent town meeting, all hospital employees had the chance to ask questions, gain knowledge, and express concerns. Most who attended were not only employees but parents as well, and they openly expressed their fears, hopes, and expectations. No one there had all the answers about how to deal with bioterrorism effectively and efficiently, but the town meeting was, at least, helpful as an occasion to share feelings. And, if nothing else, it offered an opportunity to question our current security and infection control practices and to consider whether we need to look at alternatives to what we do now.
Similar to what other hospitals want, we want to be prepared for any emergency. We want to convey to parents, employees, medical staff, and the public at large that we are "ready." Now, we realize, is the time to update all telephone trees. Now, we agree, is also a good time for another disaster drill. In the past, such drills were seen as an obligation, taken seriously by only a few; now, everyone wants to be involvedto learn, to help. We should seize the opportunity to include interested staff members who may otherwise have looked the other way. Community physicians, not only hospital employees, should be invited to participate.
We expect our physicians to put matters in perspective: to consider the most likely diagnoses first, yet maintain an index of suspicion for rare possibilities. Almost all children with flu-like symptoms who we'll evaluate in the next few weeks will have the flu, but we will at least consider the remote possibility of anthrax. Certainly, their parents will remind us of this possibility, and we must address their concerns seriously. As emergency physicians, reassuring the family at this frightening time may still be our most important role.
Concrete actions to prepare for possible bioterrorism
Our hospital is taking steps that may also make sense, in modified form, for community-based clinicians and their practice. For example, we are moving to:
- Create or modify educational pamphlets designed for lay people and, distinctively, for staff and make them readily available
- Post protocols in the ED for postexposure treatment
- Continue to have relevant staff meetings as a way of updating personnel about the threat that these diseases pose as a terrorist weapon
- Become familiar with ways to obtain access to our state's department of public health and the information it offers (telephone numbers, Web site addresses, etc.)
- Seek expertise from hospital infectious disease and infection control specialists
- Remain aware of cases reported in nearby areas.
We should also note that our hospital is involving community pediatricians in issues of disaster management, training them to recognize cases of bioterrorism and to manage the fear associated with this new threat.
Steven M. Selbst, MD, and Kate Cronan, MD
DR. SELBST is vice chairman of the department of pediatrics at A.I. du Pont Hospital for Children, Wilmington, Del., and a member of the editorial board of Contemporary Pediatrics.
DR. CRONAN is director of the division of emergency medicine at A.I. du Pont Hospital for Children, Wilmington, Del.
J. Thomas Cross. Biological terrorism and warfare: Not sci-fi any longer. Contemporary Pediatrics 2001;12:37.