Boy’s “mole” appears overnight
An anxious mother of a 10-year-old boy brings him to the office for evaluation of a new mole that appeared on his back in the last 24 hours. What is causing the rapidly developing pigmented lesion in this patient?

THE CASE
An anxious mother of a 10-year-old boy brings him to the office for evaluation of a new mole that appeared on his back in the last 24 hours (Figure 1). What is causing the rapidly developing pigmented lesion in this patient?
NEXT: What's the diagnosis?
Dermcase diagnosis: EMBEDDED LONE STAR TICK
âª
Amblyomma americanum, or Lone Star tick, is the most common tick in the mid-Atlantic and southern Atlantic states that feeds on humans. Larva, nymph, and adult stages are known to bite humans.1 Nymphs and adult ticks are known to be vectors of a variety of human pathogens including Rickettsia rickettsii, Francisella tularensis, and at least 3 ehrlichial human pathogens. The A americanum tick also is associated with the development of southern tick-associated rash illness (STARI), which produces a Lyme disease-like syndrome that is showing increasing prevalence in the Atlantic states. Studies thus far have not proven that A americanum is a vector for transmitting Borrelia burgdorferi to humans.
More: When rash and fever become an emergency
âªNymphal Lone Star ticks are most prevalent from May through early August with peak activity from May through June. Larvae and nymphs are very small and can be easily overlooked. The nymph stage of A americanum also is much smaller than the adult and in many cases has been misdiagnosed as Ixodes scapularis, the tick that transmits Lyme disease. Studies of biting ticks conducted in Virginia and Maryland as recently as 2005 demonstrated that as many as 98% of human-biting ticks were caused by A americanum, despite the fact that many of the tick-bite victims reported they had been bitten by I scapularis.1
It is believed that the failure to differentiate tick species has contributed to the overdiagnosis of Lyme disease in southern Atlantic states. It is important for clinicians practicing in states where tick populations overlap to be mindful of local tick prevalence and the spectrum of human pathogens local species can transmit.
Differential diagnosis
âªThe differential diagnosis of rapidly developing pigmented lesions in children is broad and may raise concern for a cutaneous malignancy (ie, malignant melanoma). The following nonmelanocytic entities may be considered during the evaluation of these patients: talon noir (small trauma-induced hematoma); pyogenic granuloma; traumatic tattoo (graphite tattoo); embedded hairs; arthropods (ticks, insects); and skin exposure to exogenous inks or dyes.
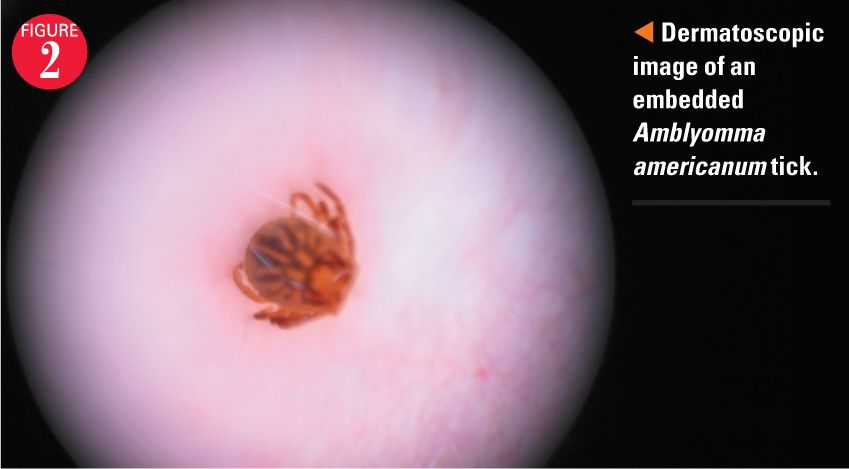
A detailed history and examination is useful in delineation. Diagnosis may be further aided by thorough cleansing of the area with alcohol pads and dermoscopy (illuminated magnification), which would highlight the pertinent features of the diagnoses listed above (Figure 2).âª
âª
Banal nevi have a wide range of dermatoscopic features, but classically will reveal symmetric reticular networks of brown pigment or pigment within the furrows of dermatoglyphics. Talon noir typically presents as a nonblanchable, violaceous to golden-brown homogenous macule on the heel, and represents subcorneal hemorrhage from trauma. This may be easily removed with gentle scraping from a scalpel blade.
Pyogenic granulomas have predilection for the face and extremities of children, pregnant women, and patients on certain medications (isotretinoin). These friable papules arise rapidly and bleed readily. Patients will commonly present to the office with a positive “Band-Aid sign." Pigmented macules and patches that are the result of dye exposure (eg, food coloring, henna tattoos, dirt) may be removed with alcohol pads and do not demonstrate characteristic dermatoscopic findings of nevi.
Under magnification, ticks and their distinctive patterned scuta, embedded hairs, and foreign bodies are readily observable. A skin biopsy is encouraged to evaluate new asymmetric, irregular, changing pigmented lesions that cannot be explained by the innocent diagnoses outlined previously. âª
Our patient
A topical anesthetic was applied to the area around the tick under plastic wrap occlusion for 30 minutes and then removed with a forceps and gentle scraping with a number 15 blade. The boy’s mother was instructed to monitor the site for the development of signs of secondary infection or rash.
REFERENCE
âª1. Stromdahl EY, Hickling GJ. Beyond Lyme: aetiology of tick-borne human diseases with emphasis on the south-eastern United States. Zoonoses Public Health. 2012;59(suppl 2):48-64.
Dr Eccles is a fourth-year dermatology resident, Walter Reed National Military Medical Center, Bethesda, Maryland. Dr Mitchum is a fourth-year dermatology resident, Walter Reed National Military Medical Center, Bethesda. Dr Cohen, section editor for Dermcase, is professor of pediatrics and dermatology, Johns Hopkins University School of Medicine, Baltimore, Maryland. The authors and section editor have nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article. Vignettes are based on real cases that have been modified to allow the authors and section editor to focus on key teaching points. Images also may be edited or substituted for teaching purposes.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.