Child with abnormal eye lesions
A 12-year-old girl is referred to the office after a routine dilated eye exam shows unusual retinal lesions. The child has been having headaches for the past 2 years that are described as mostly in the vertex with no other associated vomiting symptoms. Headaches are intermittent and usually relieved with ibuprofen.
THE CASE
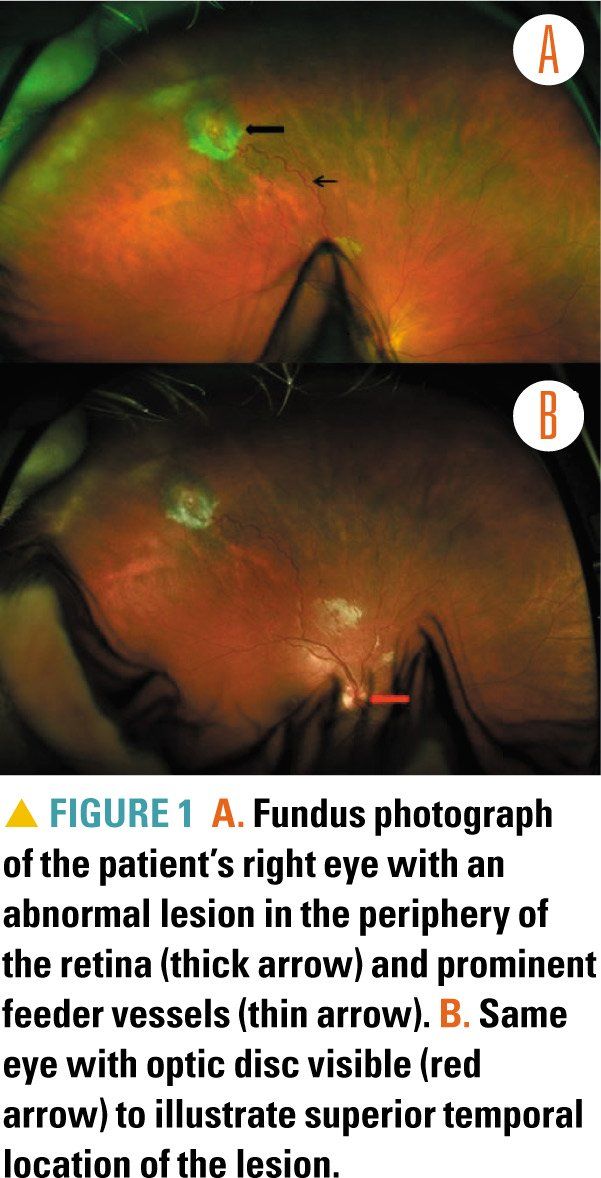
A 12-year-old girl is referred to the office after a routine dilated eye exam shows unusual retinal lesions (Figure 1). The child has been having headaches for the past 2 years that are described as mostly in the vertex with no other associated vomiting symptoms. Headaches are intermittent and usually relieved with ibuprofen.
Family history
The girl’s mother has a history of a cerebellar tumor and hypertensive crisis, which were diagnosed after presenting with a seizure in her late 20s. The maternal grandmother had a sudden death also in her late 20s from transforaminal herniation owing to a cerebellar mass.
The patient’s mother was diagnosed with a genetic disorder through targeted genetic testing given her constellation of symptoms. Because of this family history, the patient was closely monitored to see if she would develop any signs and symptoms of the disease as she was growing up.
Physical exam
On physical examination, the patient’s blood pressure was 122/64 mmHg. She had no neurocutaneous stigmata. Her neurologic exam was unremarkable with normal visual acuity.
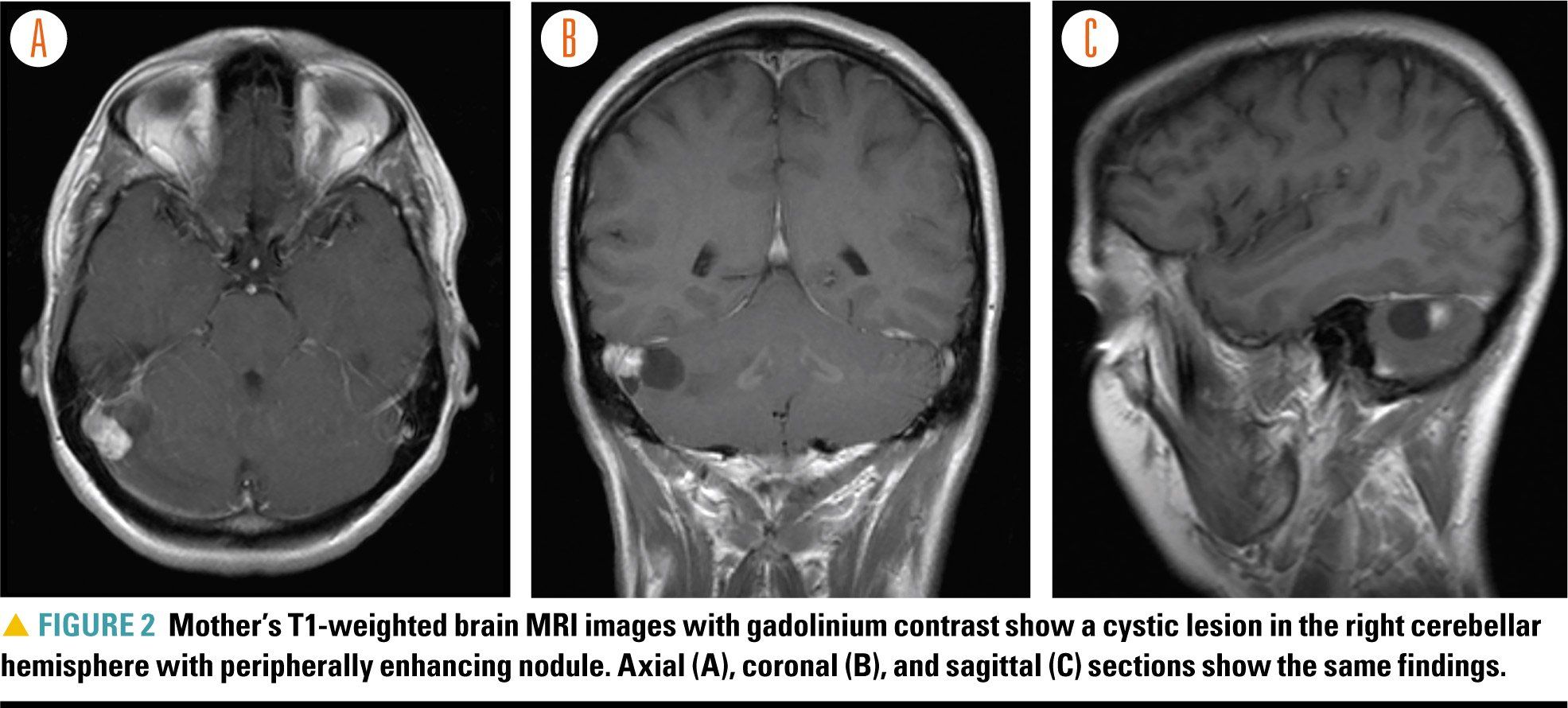
Based on the significant family history, magnetic resonance imaging (MRI) of the brain was done, which was normal. Review of her mother’s brain MRI reveals clues to the diagnosis (Figure 2).
Differential diagnosis
The eyes are commonly referred to as “windows” of the brain. In this particular case, they provide an important clue to the patient’s diagnosis. The retinal lesion presented in Figure 1 shows a vascular tumor of the eye with prominent feeding vessels. This description is consistent with a retinal hemangioblastoma, also known as a retinal angioma.
More: Infant's seizure and skull fracture could point to child abuse
Her mother’s brain MRI illustrates a cystic lesion in the right cerebellar hemisphere with a small mural nodule in the periphery. Brain lesions with this description can be either a pilocytic astrocytoma or hemangioblastoma. Posterior fossa tumors are common in childhood and have distinct features on neuroimaging to help with diagnosis. Certain tumors are sometimes associated with systemic disease or neurologic syndromes that require early diagnosis not only for appropriate management of the tumor but also for surveillance and anticipation of other potential manifestations (Table 11).
NEXT: More on the differential diagnosis
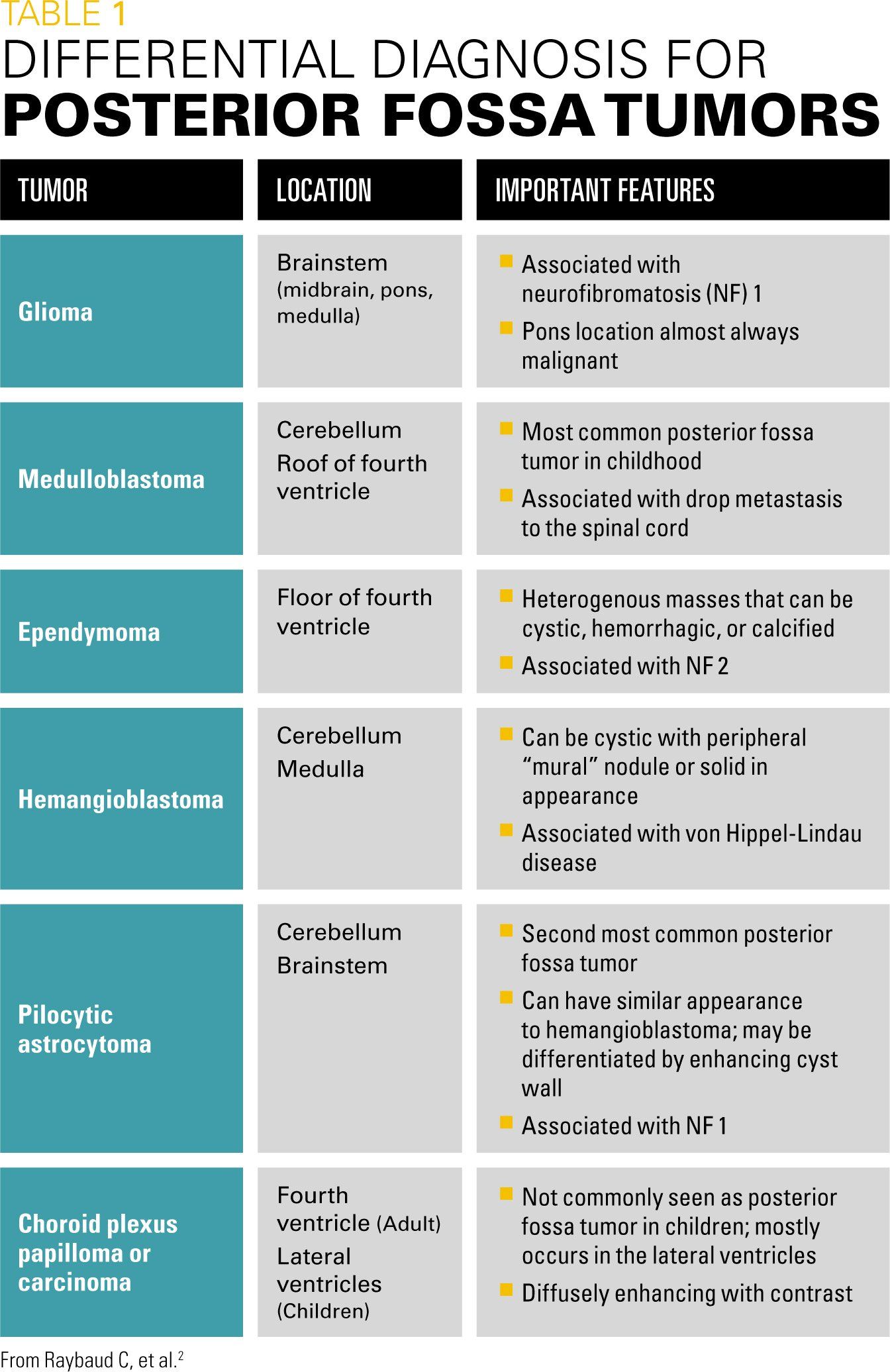
Complications from posterior fossa tumors largely depend on their location. Acute hydrocephalus from blockage of cerebrospinal fluid flow is an important complication that needs prompt recognition. Cranial neuropathies and other brainstem deficits are also common manifestations for tumors that compress or infiltrate these structures. Ataxia and gait instability are prominent with cerebellar lesions.
Recommended: Pediatric high-grade glioma is not one tumor type but many
The presence of hemangioblastomas in the eye and central nervous system raise suspicion for von Hippel-Lindau (vHL) disease. The diagnosis is further supported by the autosomal dominant inheritance pattern. The patient underwent genetic testing for the vHL gene, which showed mutations consistent with the diagnosis and similar gene mutation as her mother.
Discussion
Von Hippel-Lindau disease is an autosomal dominant disorder caused by a mutation in the vHL tumor suppressor gene on chromosome 3, resulting in benign and malignant tumors. A vHL gene abnormality is present in 1 in 36,000 persons.2 Affected individuals may manifest at any age, but most commonly between 18 and 30 years.
The disease was initially described by Eugen von Hippel and Arvid Lindau in the early 1900s.3 The vHL gene codes for a protein called pVHL, which plays a role in tumor suppression. With abnormal or absent pVHL, there can be uncontrolled angiogenesis and tumor growth in susceptible tissue leading to the hallmark tumors of the disease.4
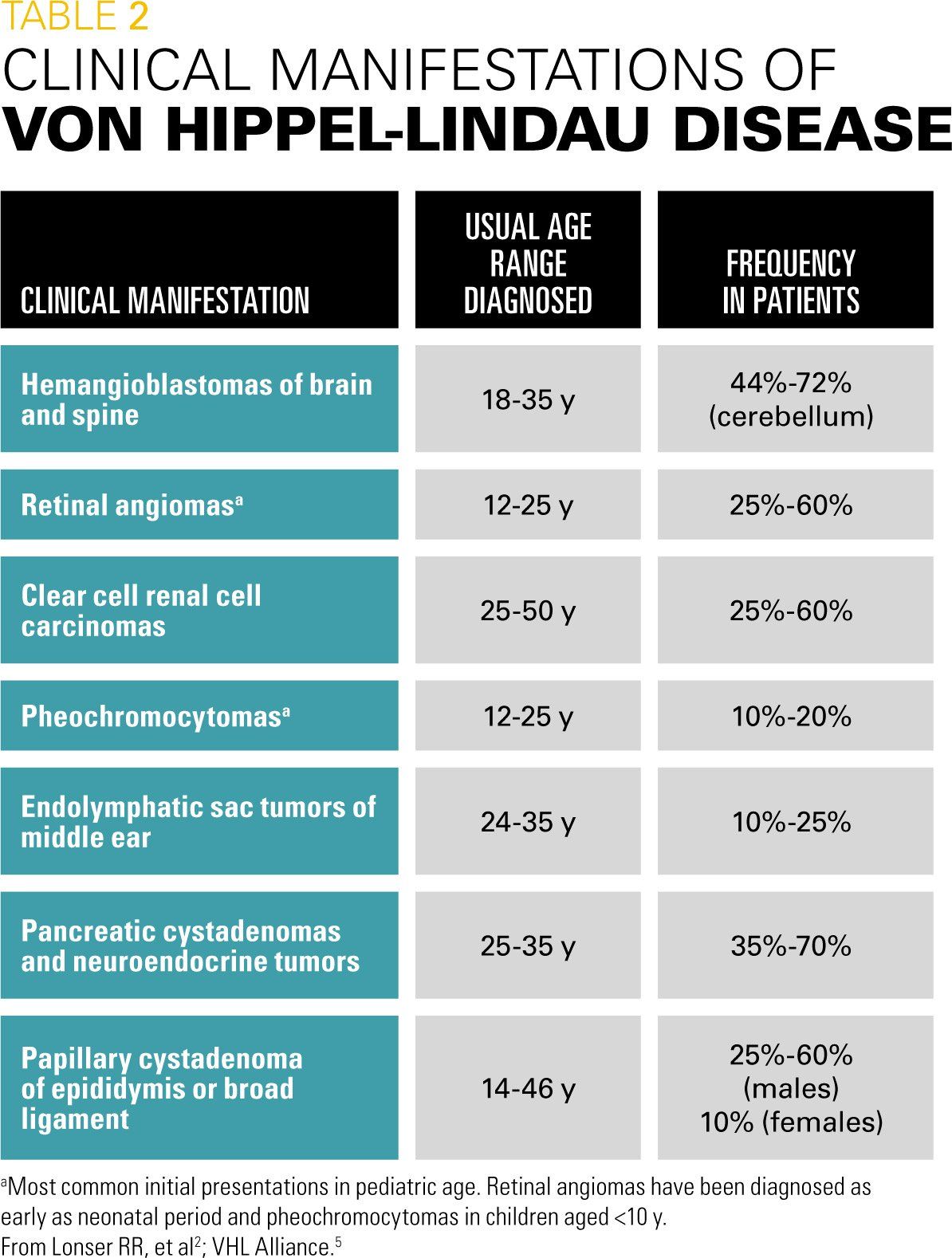
Clinical manifestations of vHL disease include hemangioblastomas of the brain and spine; retinal angiomas; clear cell renal cell carcinomas; pheochromocytomas; endolymphatic sac tumors of the middle ear; pancreatic tumors; and papillary cystadenomas of the epididymis and broad ligament (Table 22,5). Clinical diagnosis can be made if there is 1 major manifestation of vHL disease in patients with a positive family history, or at least 2 major manifestations including 1 hemangioblastoma in sporadic cases. Currently, genetic testing is readily available in cases with suspected vHL disease.
NEXT: Treatment and management of the disease
Gene testing for vHL can be sent as a blood sample for single gene sequencing or deletion/duplication analysis. Also, vHL can be classified into subtypes based on the mutation present. These vHL Type II subtypes are associated with missense mutations and are at higher risk for pheochromocytoma.6
Early diagnosis is key as patients face a lifetime of possible manifestations. Surveillance guidelines are in place so caregivers can be proactive in diagnosing these tumors at the earliest.
Although this disorder manifests clinically in early adulthood, children also have been reported with symptoms/signs. The most common features occurring in the pediatric age group are retinal angiomas, pheochromocytomas, and central nervous system hemangioblastomas. Anticipatory guidance and surveillance by the general pediatrician and appropriate subspecialty referral for intervention are key to management.
In early childhood (aged <5 years) of patients with known vHL disease, pediatricians should perform focused annual evaluation for any neurologic symptoms as well as vision and hearing problems. Because of the risk for pheochromocytoma, patients should have blood pressure monitoring in their visits. Formal ophthalmology evaluation on a yearly basis is recommended.
Between ages 5 to 15 years, additional yearly evaluations should include tests for fractionated metanephrines in blood or a 24-hour urine test. Annual abdominal ultrasound (US) should be done starting at around age 8 years to screen for masses, and even earlier if clinically indicated. If biochemical abnormalities are found on screening tests, then abdominal MRI or metaiodobenzylguanidine (MIBG) scan is recommended. A complete hearing assessment by an audiologist should be done every 2 to 3 years or even more frequently if any hearing loss, tinnitus, or vertigo is found.
Next: Girl's blistering rash spreads to eyes and face
Beyond age 16 years, MRI of the brain and spinal cord is done every 2 years to evaluate for tumors in addition to other surveillance tests previously established.5
Treatment and management
Patients with vHL require a multidisciplinary approach. There is no targeted treatment toward the genetic mutation available as yet. Management is largely directed toward identifying the tumors early and performing surgical resection for symptomatic lesions. In the case of pheochromocytoma specifically, adequate alpha-adrenergic blockade and blood pressure control should be achieved prior to surgery. For symptomatic retinal angiomas, laser photocoagulation or cryotherapy are options for treatment.7 Patients and their families should undergo genetic screening and counseling for at-risk members.
Patient outcome
The patient is currently receiving surveillance monitoring as recommended. Her recent blood metanephrine screening test has been negative. Her headaches are easily managed with rescue ibuprofen. She underwent cryotherapy for retinal angioma in her right eye. She developed another retinal angioma in her left eye and was treated with laser ablation.
References
1. Raybaud C, Ramaswamy V, Taylor MD, Laughlin S. Posterior fossa tumors in children: developmental anatomy and diagnostic imaging. Childs Nerv Syst. 2015;31(10):1661-1676.
2. Lonser RR, Glenn GM, Walther M, et al. von Hippel-Lindau disease. Lancet. 2003;36(9374):2059-2067.
3. Richard S, Graff J, Lindau J, Resche F. Von Hippel-Lindau disease. Lancet. 2004;363(9416):1231-1234.
4. Kim WY, Kaelin WG. Role of VHL gene mutation in human cancer. J Clin Oncol. 2004;22(24):4991-5004.
6. Zbar B, Kishida T, Chen F, et al. Germline mutations in the Von Hippel-Lindau disease (VHL) gene in families from North America, Europe, and Japan. Hum Mutat. 1996;8(4):348-357.
5. VHL Alliance. What You Need to Know About VHL. 5th ed. Available at: https://www.vhl.org/patients/vhl-handbook/. Published 1993. Updated 2015. Accessed January 17, 2018.
7. Singh AD, Nouri M, Shields CL, Shields JA, Perez N. Treatment of retinal capillary hemangioma. Ophthalmology. 2002;109(10):1799-1806.