Child With Difficulty in Walking
A 4-year-old boy with a history of autism presents to his pediatrician’s office with a complaint of right leg pain. He is presumed to have pulled a muscle; an elastic bandage is applied and he is given ibuprofen. Over the next few days, he begins falling and tripping and is unable to maintain his balance. At a return visit, the patient’s mother says her son’s right leg is “like Jell-O” and that he appears to be dragging the leg.
A 4-year-old boy with a history of autism presents to his pediatrician's office with a complaint of right leg pain. He is presumed to have pulled a muscle; an elastic bandage is applied and he is given ibuprofen. Over the next few days, he begins falling and tripping and is unable to maintain his balance. At a return visit, the patient's mother says her son's right leg is "like Jell-O" and that he appears to be dragging the leg. He has not had a fever, but his appetite has been decreased and he has been less active than usual. He denies bowel or bladder symptoms and any history of trauma.
HISTORY
The patient has mild motor and speech delay associated with his autism diagnosis. He was hospitalized as an infant for rotavirus infection but has otherwise been healthy. He had a viral upper respiratory tract infection 2 weeks earlier and received his age 4 immunizations at around the same time. There is no family history of any neurological or muscle disorders. The child lives with his mother, father, 2 sisters, and twin brother, all of whom are healthy. He takes no medications and has had no known abnormal ingestions.
PHYSICAL EXAMINATION
The child is in no apparent distress; he is cooperative and answers questions appropriately. His weight is 20.5 kg (75th percentile); height, 112 cm (75th percentile). Temperature is 36.6°C (98.0°F); heart rate, 118 beats per minute; respiration rate, 28 breaths per minute; and blood pressure, initially 128/65 mm Hg but on a second measurement, 107/61. He is normocephalic, with clear conjunctivae and normal findings on a funduscopic examination. Lungs are clear, heart is normal, abdomen is benign. Examination of the extremities reveals no rashes or deformities and no swelling or erythema of the joints. A neurological examination shows normal strength in the left lower extremity but decreased strength in the right foot. Deep tendon reflexes in the right lower extremity are absent. The patient has a waddling gait and appears to drag his right foot. Truncal stability is normal. Sensation is normal throughout. Cranial nerves II through XII are intact.
LABORATORY AND IMAGING RESULTS
A complete blood cell count and metabolic panel are normal. Erythrocyte sedimentation rate is 15 mm/h; C-reactive protein level is less than 0.5 mg/dL. A series of radiographs of the right foot and ankle, bilateral hip and pelvis films, and a head CT scan are all normal.
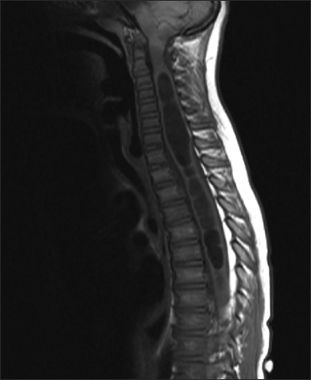
Because of the constellation of symptoms and physical findings, an MRI of the cervical, thoracic, and lumbar spine is obtained, which is as shown.
What is the most appropriate next step in management?
Answer on the Next Page
The correct answer is B
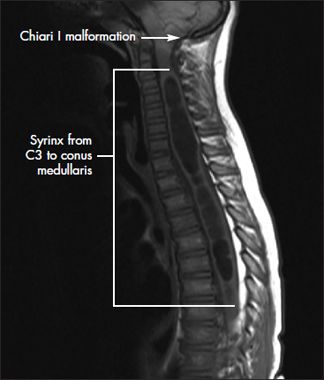
Figure – This T1-weighted MRI scan of the patient's spine shows a syrinx extending from C3 to the conus medullaris and an associated Chiari I malformation.
The MRI of the spine shows a large syrinx extending from the level of the third cervical vertebra to the conus medullaris, leading to a diagnosis of syringomyelia. A Chiari I malformation is also visible (Figure).
Before the laboratory results and MRI were obtained, the differential diagnosis was extensive (Table). Results of the history taking and physical examination-especially the combination of loss of deep tendon reflexes (more of a lower motor neuron problem) and a possible gait disturbance (more of an upper motor neuron problem)-made it difficult to confine the differential to one area of the neurological system. The process of narrowing it was further complicated by the necessity of determining the location of the lesion and assessing gait in a patient with a developmental disability.
Initially, Guillain-Barr syndrome (GBS), acute disseminated encephalomyelitis, and multiple sclerosis seemed the most likely possibilities. Although GBS is usually preceded by a diarrheal illness, the rare variant of GBS called Miller Fisher syndrome typically presents with the classic triad of ataxia, areflexia, and ophthalmoplegia.1 MRI helped to clarify the picture.
Syringomyelia: an overview. Syringomyelia is defined as a fluid-filled cavity within the spinal cord. Its pathogenesis is unclear and controversial. Syringomyelia can either communicate with the central cerebrospinal fluid canal or be localized and noncommunicating. The communicating type is strongly associated (more than 25% of cases) with Chiari I malformations (displacement of the cerebellar tonsils and posterior vermis through the foramen magnum). The noncommunicating type can be associated with spinal neoplasms (such as cystic astrocytomas), trauma, or arachnoiditis.2 Syringomyelia is a classic nontraumatic cause of central cord syndrome.3 Compressive forces from the syrinx have the most damaging effect on the central mass of the cord substance and can affect motor recovery.
Practice Pearl 1: Syringomyelia usually has a chronic, stable clinical course. Asymptomatic patients are often followed conservatively with serial imaging studies and neurological examinations.
Presentation. The presentation of patients with syringomyelia varies with the location and size of the syrinx. A syrinx can be asymptomatic and discovered incidentally on spinal cord imaging. Because of their slow evolution, lesions rarely produce symptoms in childhood. Syringomyelia associated with Chiari I malformations usually presents in young adulthood; the initial symptom is typically a suboccipital headache exacerbated by exertion (eg, coughing) accompanied by diffuse neck pain.4
Interruption of the crossing fibers of the lateral spinothalamic tracts causes loss of pain and temperature sensation at the level of the spinal cord lesion, with preservation of the senses of light touch, vibration, and position. These sensation deficits can lead to the development of fingertip ulcers.
As the cavity expands, involvement of the ventral anterior horn cells can lead to weakness, atrophy, and loss of deep tendon reflexes. Involvement of the posterior dorsal columns can lead to vibration and touch disturbances. Upper motor neuron signs, such as spasticity and hyperreflexia, usually develop in the lower extremities; however, long cavities may produce lower motor neuron signs in all limbs.2,5 Upward extension of the cavity into the lower brain stem, which is known as syringobulbia, can result in dysarthria, nystagmus, and decreased sensation of the face. Patients can also present with progressive scoliosis, torticollis, or neuropathic pain.6
Disease course and treatment. Syringomyelia usually has a chronic, stable, clinical course. Asymptomatic patients are often followed up conservatively with serial imaging studies and neurological examinations.6
In patients with syringomyelia who have progressive scoliosis or progressive motor and/or sensory loss, surgical treatment is appropriate. Emergent surgery (choice A) is usually not warranted. In particular, the absence of syncope, apnea, or a history of aspiration in this child argued against immediate intervention.7 However, waiting 6 months to reevaluate the patient (choice D) would not be appropriate either, since he has had progressive worsening of symptoms.
Practice Pearl 2: Patients with syringomyelia and a Chiari malformation who have worsening symptoms require surgical decompression of the foramen magnum and a laminectomy of the upper cervical vertebrae-along with duraplasty for best results.
In children with an associated Chiari malformation, decompression of the foramen magnum and laminectomy of the upper cervical vertebrae relieves the symptoms caused by compression of the tonsils (eg, posterior neck pain, tussive headache, apneic spells). However, diminishment of the symptoms caused by the syrinx itself (eg, weakness, atrophy, loss of deep tendon reflexes) is variable and unpredictable.8 If decompression does not reduce the size of the syrinx, shunting of the cavity may be required; however this is very rare.1
Syringomyelia unaccompanied by a Chiari malformation may require a posterior fossa decompression. However, this only occurs under special circumstances.9
Intravenous corticosteroids (choice C) do not have a role in the treatment of syringomyelia. Corticosteroid treatment might be considered in a patient whose symptoms were associated with a postinfectious reaction, such as acute disseminated encephalomyelitis or transverse myelitis. However, management of syringomyelia is primarily surgical; muscle relaxants and analgesics can be used for symptom control.
Outcome of this case. This patient underwent posterior fossa decompression with duraplasty the next week. Since decompression, his ambulation has improved; however, he still has mild ataxia. He will need long-term physical and occupational therapy to overcome the residual deficits from his syringomyelia.






References:
REFERENCES:
1.
Snyder LA, Rismondo V, Miller NR. The Fisher variant of Guillain-Barré syndrome (Fisher syndrome).
J Neuroophthalmol
. 2009;29:312-324.
2.
Haslam RH. Syringomyelia. In: Behrman RE, Kliegman RM, Jenson HB, eds.
Nelson Textbook of Pediatrics
. 17th ed. Philadelphia: WB Saunders; 2004:2051.
3.
Brodbelt AR, Stoodley MA. Post-traumatic syringomyelia: a review.
J Clin Neurosci
. 2003;10:401-408.
4.
Perrin RG, Fehlings M. The etiology of syringomyelia in association with lesions of the foramen magnum.
J Neurol Sci
. 2004;220:1-2.
5.
Fenichel GM.
Clinical Pediatric Neurology: A Signs and Symptoms Approach
. 5th ed. Philadelphia: Elsevier Saunders; 2005:216-217.
6.
Haroun RI, Guarnieri M, Meadow JJ, et al. Current opinions for the treatment of syringomyelia and chiari malformations: survey of the Pediatric Section of the American Association of Neurological Surgeons.
Pediatr Neurosurg
. 2000;33:311-317.
7.
Yassari R, Frim D. Evaluation and management of the Chiari malformation type 1 for the primary care pediatrician.
Pediatr Clin North Am
. 2004;51:477-490.
8.
Oldfield EH, Muraszko K, Shawker TK, Patronas NJ. Pathophysiology of syringomyelia associated with Chiari I malformation of the cerebellar tonsils: implications for diagnosis and treatment.
J Neurosurg
. 1994;80:3-15.
9.
Iskandar BJ, Hedlund GL, Grabb PA, Oakes WJ. The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression.
J Neurosurg
. 1998;89:212-216.
For more information on the different types of Chiari malformations, their symptoms, treatment, and prognosis, visit our Web site at www.ConsultantLive.com/pediatrics.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.