COVID-19: A battle plan for pediatricians
Combating the novel coronavirus will motivate pediatricians to make novel changes to their practices.
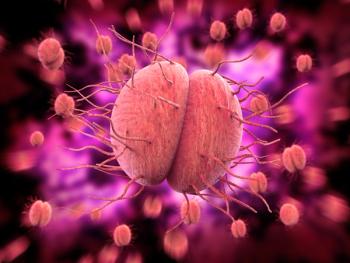
Four months ago, we all were aware there was a novel coronavirus causing an epidemic in the Wuhan region of China, but many experts expected it would be limited in scope and spread, not unlike the severe acute respiratory syndrome (SARS) epidemic and Middle East respiratory syndrome (MERS) outbreaks that occurred years ago.
And then COVID-19 began its march around the world, finally arriving on our shores on January 20th.1 We underestimated the tenacity of the virus and were caught without adequate supplies of personal protective equipment (PPE), had no antivirals with which to combat the virus, and had extremely limited testing capability. Clearly, our government and health care system were woefully ill prepared to deal with COVID-19.
Fast forward to mid-March. Advisories to “stay at home” were issued in a cascading fashion by state governors, and nonessential businesses were closed. Now, weeks later, pediatricians still are utilizing telehealth for ill and health-maintenance visits, seeing fewer patients in our offices, and dealing with the financial impact of the pandemic on our practices. As mitigation efforts begin to diminish novel coronavirus infections, we continue our efforts to care for our patients as well as ourselves.
Although we remain optimistic about eventually emerging from seclusion, the reality of the situation is that, at best, local communities will gradually relax restrictions, but some degree of social distancing will last for weeks if not months. During this time, we need to do our best to keep our practices open and accessible. We also need to plan ahead for accommodating patients in our offices once we start the recovery process.
Ultimately, I expect that our response to the novel coronavirus pandemic will be the development of a novel practice model that will allow our practices to survive adversity in the “here and now” and prosper once PPE, toilet paper, and hand sanitizer become plentiful once again.
Your battle plan
- Assume all patients and parents may be capable of transmitting the novel coronavirus. We know that patients can shed the virus days before they become symptomatic or while remaining asymptomatic carriers. Parents and patients should be screened for COVID-19 risk factors and children should be accompanied by one guardian. Your parking lot is now considered your waiting room. You call the parent in their vehicle when they are ready to be roomed.
- Use services such as the Comprehensive Health and Decision Information System (CHADIS; Total Child Health Inc.; Baltimore, Maryland) so patients and parents can fill out the Modified Checklist for Autism in Toddlers (MCHAT), Parents Evaluation of Developmental Status (PEDS), the Ages and Stages Questionnaire (ASQ), the Patient Health Questionnaire (PHQ), and other forms online with automatic scoring to expedite well visits provided by TH.
- Increase daily visit volume by turning phone calls involving “advice” questions into TH visits for which patients and insurance companies get charged, and your practice generates revenue.
- It is probably prudent to consider utilizing full PPE for all patient visits and not just ill visits. If your PPE is in short supply, you can reuse PPE according to Centers for Disease Control and Prevention (CDC) guidelines (
www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy ). - Be sure to sanitize rooms (
www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-buildingfacility.html ) thoroughly following well visits and “extra thoroughly” following visits involving coughing or febrile patients. Although I have not seen official recommendations from the CDC, and understanding that the novel coronavirus is aerosolized following a cough or sneeze, I personally suggest that offices spray a room in which a febrile coughing child was seen with an air sanitizer such as Lysol Spray or similar product. Patients aged 2 years and older and parents should wear masks whenever possible. - Take copays via credit card over the phone and try not to take cash. Although the novel coronavirus is unlikely to be spread by exchanging cash, it is a possibility that must be considered.
- Take the opportunity to renovate your medical home. Whereas some patients may seek TH care via urgent care facilities, largely because of ease of access, during the pandemic you are just as accessible as community clinics. You should call patients back following an acute illness to check on their status and to arrange follow-up visits when appropriate. Consider starting a newsletter for patients distributed electronically. Also, as you get more comfortable with TH, consider holding Zoom meetings for patients or parents with similar medical problems such as attention-deficit/hyperactivity disorder (ADHD), or just to address concerns regarding the pandemic.
- Be creative in arranging for immunizations via drive-through arrangements or administered in the office at nursing visits.
- Considering partnering with community mental health providers to provide TH mental health services.
- Encourage parents of newborns to purchase baby scales (or provide these by partnering with hospitals and other community resources). Using these Using these for monitoring babies with reflux or formula intolerance will likely reduce the number of in-office visits needed for ensuring these babies are gaining weight appropriately.
References:
1. Holshue ML, Debolt C, Lindquist S, et al; Washington State 2019-nCoV Case Investigation Team. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936.
2. Notario PM, Gentile E, Amidon M, Angst D, Lefaiver C, Webster K. Home-based telemedicine for children with medical complexity. Telemed J E Health. 2019;25(11):1123-1132.
3. McDaniel NL, Novicoff W, Gunnell B, Cattell Gordon D. Comparison of a novel handheld telehealth device with stand-alone examination tools in a clinic setting. Telemed J E Health. 2019;25(12):1225-1230.
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.