Cutaneous clues of child abuse
A skin manifestation can be a pediatrician’s first clue that a patient is being abused. Up to 90% of physical abuse victims present with cutaneous findings, such as bruises, lacerations, abrasions, burns, oral trauma, bite marks, and traumatic alopecia.
Reviewed by Bernard A Cohen, MD
Due to the nature of this topic and its direct implication across specialties, this article was a collaboration with our sister publication, Dermatology Times.
A skin manifestation can be a pediatrician’s first clue that a patient is being abused. Up to 90% of physical abuse victims present with cutaneous findings, such as bruises, lacerations, abrasions, burns, oral trauma, bite marks, and traumatic alopecia.1,2
Yet, there is good evidence that minor signs of child physical abuse are missed regularly by unsuspecting physicians, according to Cindy Christian, MD, chair of Child Abuse and Neglect Prevention, The Children’s Hospital of Philadelphia.
Recommended: 5 steps to a trauma-informed practice
“This is especially true in young infants, who may present with minor bruising or other skin injuries. These infants are at significant risk for further, more serious injury,” Dr. Christian said.3 “Most physicians are aware that patterned injuries and multiple injuries are concerning for physical abuse, but may not consider a minor injury in a young infant as an indicator of abuse.”
Prevalence, urgency
Child abuse is one of the leading causes of death related to injury in infants and children.4 An estimated 1520 children died from abuse or neglect in 2013.5
Physical abuse should be part of the differential diagnosis for all cutaneous and other injuries in children.6 Pediatricians are in unique position to identify and prevent child abuse.7
The earlier the abuse is detected and stopped, the better. An abused child has about a 50% chance of being abused again, and is at an increased mortality risk if the abuse is not detected and stopped after the first presentation.4,8
NEXT: What cutaneous clues may lead to a misdiagnosis?
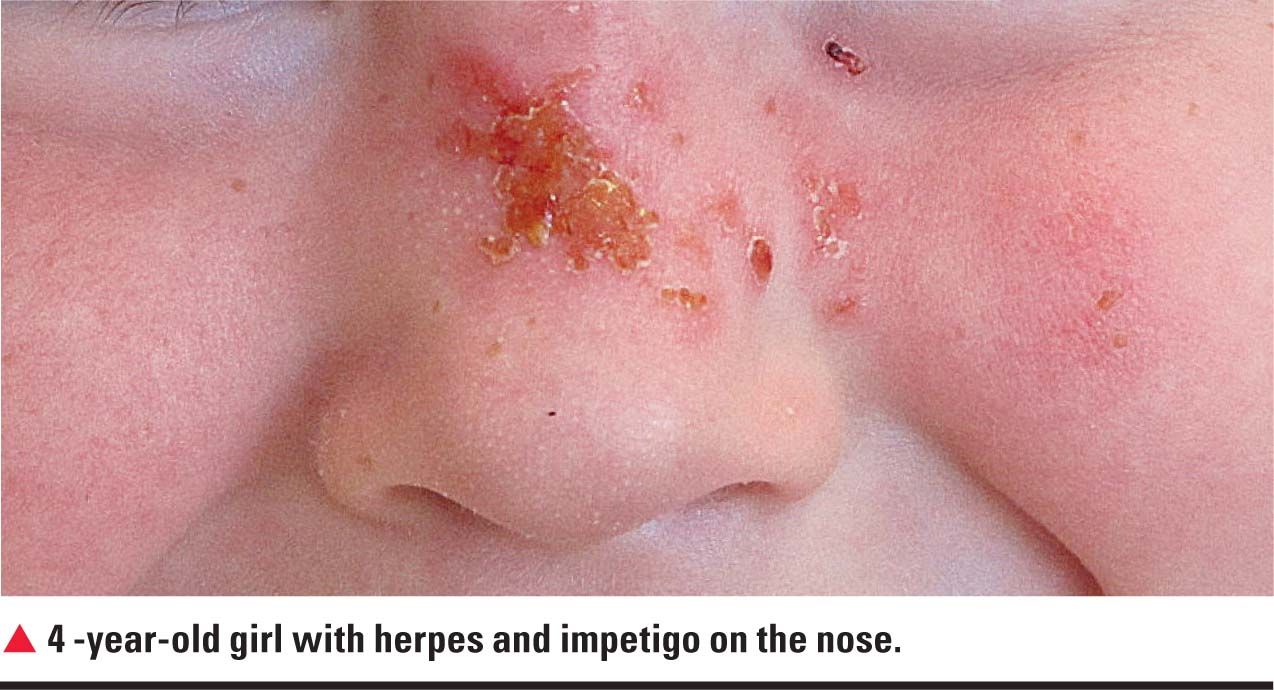
One of the challenges for pediatricians and others who suspect abuse based on cutaneous findings is that several skin disorders may mimic child abuse. Among the numerous categories of findings that can mimic cutaneous signs of abuse are common dermatologic findings, according to Dr. Christian. Abuse mimickers include: Mongolian spots, also known as congenital dermal melanosis; coagulopathies; skin infections such as impetigo, cellulitis, and scalded skin syndrome; and a form of vasculitis called Henoch-Schonlein purpura.9
More: Two-month-old with erythroderma
“In addition, ex-lax [sennosides, Novartis] ingestion can lead to severe buttocks burns in toddlers, so there are many mimics that have been described,” Dr. Christian said.
Pediatricians can avoid diagnostic errors in problematic cases by consulting with forensic pediatrics, pediatric dermatology, pediatric radiology, and others.10
One should realize that only 8% of the 90% of skin abnormalities due to child abuse are pathognomonic, according to Arnold Oranje, MD, PhD, professor emeritus in pediatric dermatology at the Erasmus Medical Center Rotterdam, the Netherlands, who directed the focus section at this year’s American Academy of Dermatology annual meeting on skin abnormalities in the differential diagnosis of child abuse. Therefore, the diagnosis of child abuse should be evaluated by a multidisciplinary team of expert specialists, he said.
Cutaneous clues: bruising
Bruising is the most common cutaneous manifestation of abuse, but abused children also can have burns, scars, lacerations, and abrasions from inflicted injury, according to Dr. Christian.

Researchers found that bruising characteristics predictive of abuse were bruising located on the torso, ear, or neck for a child up to age 4 years, and bruising in any region for an infant younger than age 4 months.11
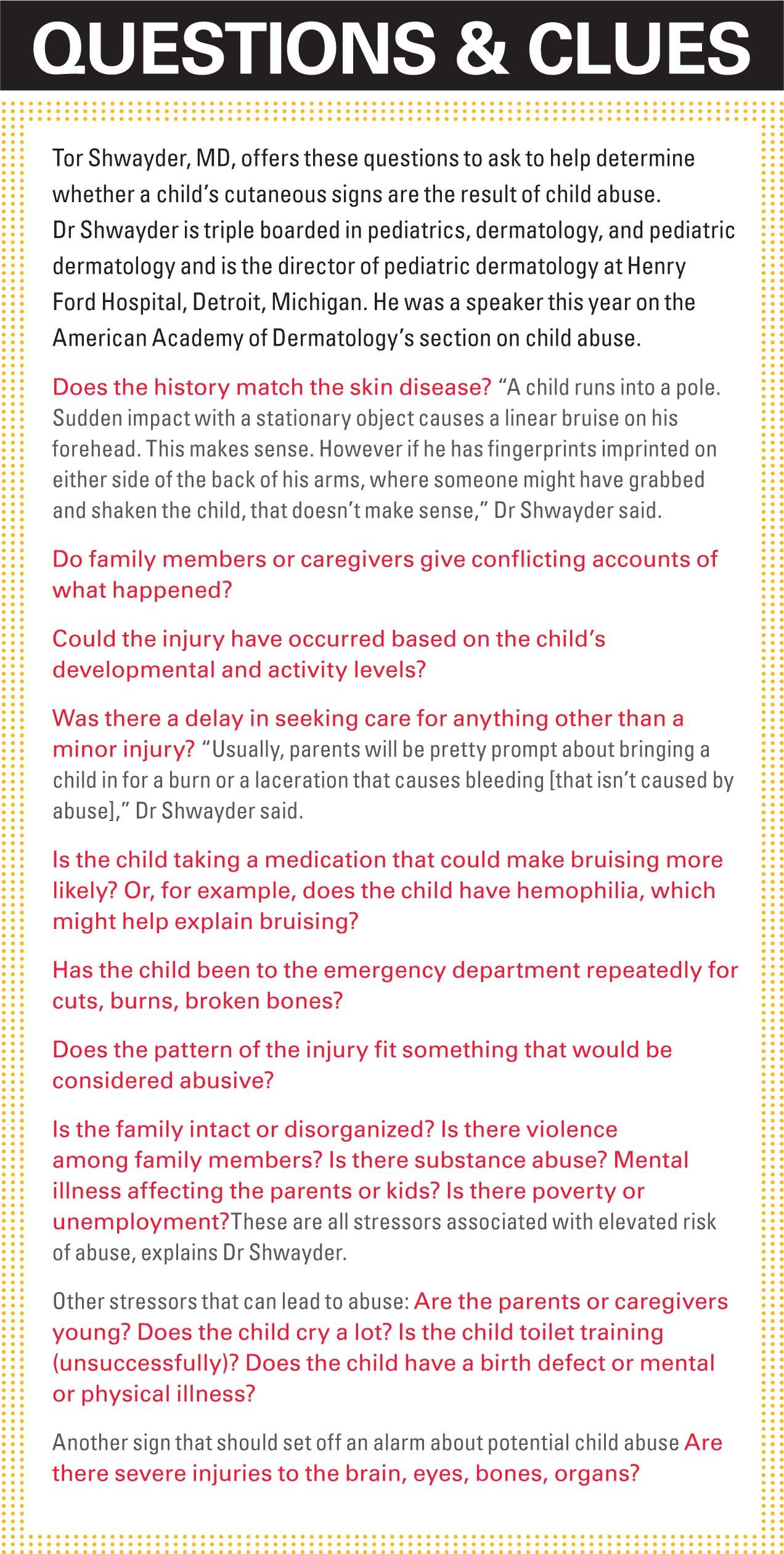
Bruises occurring on the knees, elbows, and forehead tend to be normal, but bruises on other areas should prompt questioning. These include bruising on uncommon areas that are away from bone, multiple bruises in clusters, and certain patterns (like a whip mark). Abusive bruising patterns include hand prints or grab marks, and bruises that mimic such things as belt buckles, hangers, hair brushes, paddles, spoons, and forks, according to Tor Shwayder, MD, the director of pediatric dermatology at Henry Ford Hospital, Detroit, Michigan.
NEXT: Importance of pattern analysis
Careful pattern analysis is necessary, according to Dr. Oranje.
Recommended: When rash and fever become and emergency
“Imagine you’re grabbing a young child. The thumb would be on the front of the arm, and your forefingers would be on the back of the arm,” Dr. Shwayder said. “Lip cuts or lip bruises, where someone is forcing the bottle into the mouth and telling the kid to shut up and stop crying, is another cause for concern.”
Other bruises that should alert include bruises around the eyes or on the jaw’s tip.
“You rarely [bruise the eye] when you fall because it’s protected by the bone,” Dr. Shwayder said. “And it’s pretty rare to land right on the jaw.”
Pediatricians can differentiate bite marks by other children (in a daycare center, for example) from adult bite marks by looking at the distance to the canines (the third tooth to the right or left).
“The distance to the canines is more than 3 cm in an adult and less than 3 cm in a child,” Dr. Shwayder said. “Animal bites are different than human bites. Animal bites tend to tear and they have elongated mouth.”
NEXT: Cutaneous clues from burns
Cutaneous clues: burns
Burns comprise about 5% to 22% of physical abuse, and burn abuse seems more common in children aged younger than 3 years.2
More: Treating and illness in the great outdoors
Clues that a burn might be related to abuse include:
· if the burn is older than the history would suggest;
· burns that exist with other injuries, like bruises or fractures;
· burns that are just a little too symmetrical-like those from cigarettes; and burns located in areas that are unlikely, such as the buttocks.
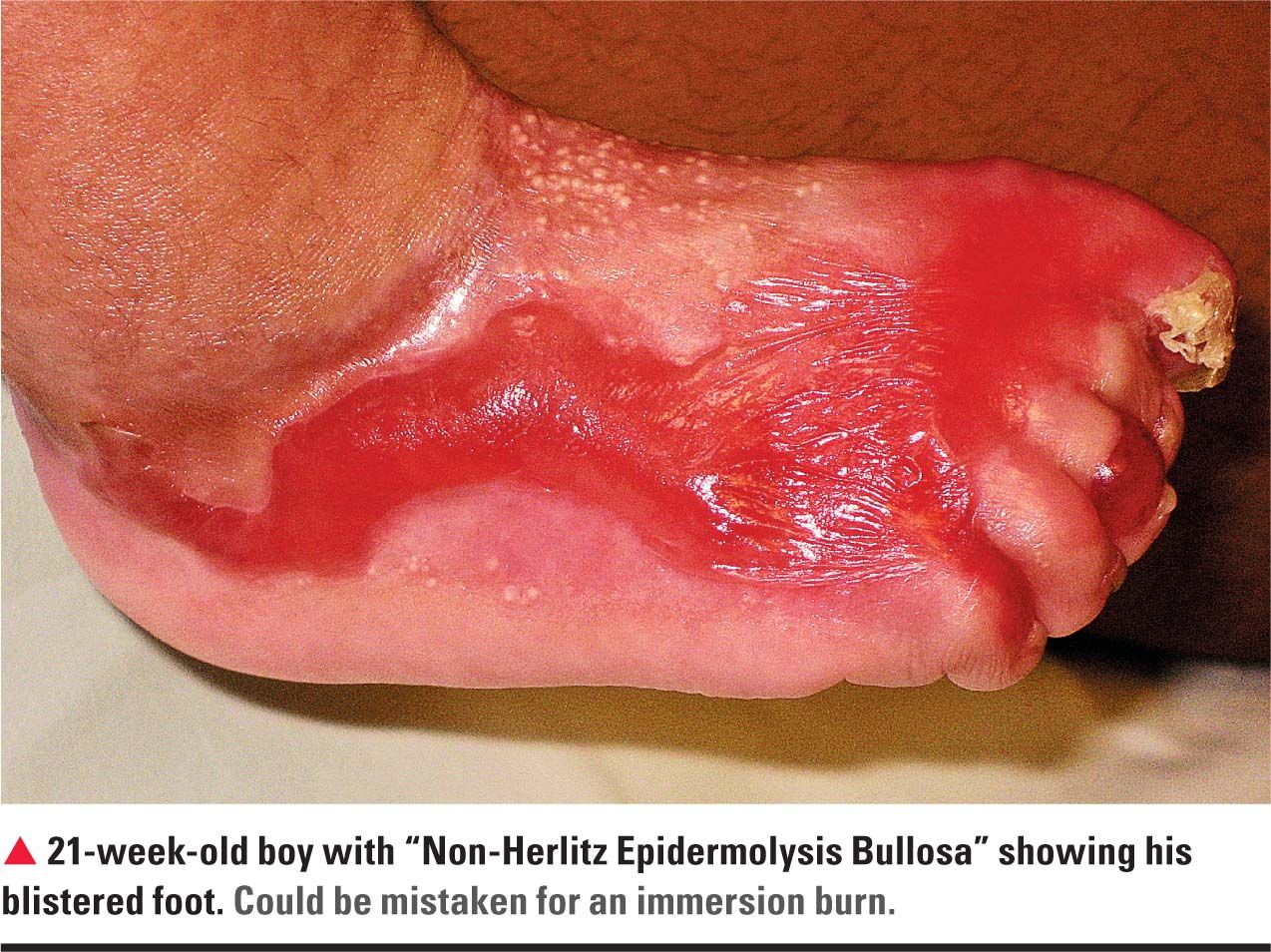
“If, for example, you take a kid and force him into a hot bath, the child will clench his buttocks cheeks together, sparing the inner part and burning the outer part,” Dr. Shwayder said.
Burns to the back of the head or the neck are unlikely, unless these are from child abuse. Additionally, burns in patterns, such as that from the bottom of an iron, can be signals of abuse.
“Burn abuse would include scalds, but you have to be careful because sometimes kids do pull things off a stove. I would say if something has been thrown at the child or the child has been immersed in hot liquid, that would look different than if a cup or pot of hot coffee falls on the child,” Dr. Shwayder said.
NEXT: Other outward signs of abuse
Hair symptoms and signs
It’s one thing to lose hair because of ringworm, traction alopecia, telogen effluvium, or alopecia areata. It’s another to have hair yanked out.
Recommended: Curious bald spot on a young girl's head
“If someone had their hair dragged and yanked out, or if they’ve been grabbed by the hair and dragged, you will see usually hematomas or hemorrhages develop in the area. And it might be tender and an irregular area of localized hair loss,” Dr. Shwayder said.
Oral clues: oral injuries
Among the most likely signs of oral abuse are injuries to the outside of the lip. That might be from a bottle being forced into a baby’s mouth or from forced oral sex. Pediatricians should look for unexplained erythema in the palette, especially in the back of the palette, according to Dr. Shwayder.

Genital area clues: sexual abuse
Sexual abuse manifests in many ways, beyond what’s apparent on the skin. Conversely, normal skin findings-especially in the gentital area-do not exclude child abuse. Pediatricians who suspect sexual abuse should inquire about a family’s history of encounters with police, as well as a child’s abdominal pain, bed wetting, or refusal to go to the bathroom at all. Sometimes, sexually abused children display inappropriate sexual behavior, sexual play, masturbation-things far beyond their years. They might have inappropriate sexual knowledge for their age or sexually aggressive behavior, according to Dr. Shwayder.
Pediatricians who suspect sexual abuse should conduct a thorough exam of the child’s genitalia, looking for bruising, lacerations, and abrasions, according to Dr. Shwayder.
Some signs of potential sexual abuse are controversial. With as prevalent as it is in society, genital herpes in a child’s diaper area might be innocent, Dr. Shwayder said. The same goes for condylomata acuminata, according to Dr. Oranje.
Dr. Oranje said there are several skin manifestations that can confuse physicians. Real skin findings may result from skin disorders not related to abuse.
“Traumatic petechiae misdiagnosed as purpura and lichen sclerosus [are] often misdiagnosed as sexual abuse. Perianal mollusca contagiosa usually have nothing to do with sexual child abuse, while condylomata acuminata sometimes does,” Dr. Oranje said.
NEXT: How can you take action?
Taking action
Pediatricians are among the frontline physicians in a position to identify abuse in their patients. Among their other roles in the protection of abused children, pediatricians report suspected abuse to the child protection agency for investigation; support families who are affected by child abuse; coordinate with multidisciplinary teams of other professionals and community agencies to provide immediate and long-term treatment to victimized children; provide court testimony when needed; provide preventive care and anticipatory guidance in the office; and advocate for policies and programs that support families and protect vulnerable children.7

It is not necessarily the actual injury alone, but the age of the patient, the history provided by the parent, and the presence of other findings that should serve to alert the physician to abuse, according to Dr. Christian.
“…it is important to take a careful, complete history, and to consider the age and developmental ability of the child. Most bruises, burns, and other skin markings on children are not the result of abuse, but these findings can often be an important clue to the diagnosis of abuse-especially, in young infants, who should not have bruises, etc., before they are ambulatory,” Dr. Christian said.
Physicians should take a proper history, according to Kipling’s principle of the 5 Ws-what, when, where, who, and why. They should try to compose a 100% certain diagnosis, sometimes also based on histopathologic findings, according to Dr. Oranje.

“The nonverbal attitude of the child also gives much information. Two examples of nonverbal signs are frozen watchfulness and ostrich behavior [where the child seems to be burying his or her head in the sand],” Dr. Oranje said.
More: Learning to care for mental health
In suspected child abuse cases, pediatricians should consider recommending a skeletal survey to x-ray the child from head to toe, according to Dr. Shwayder.
“When the history or physical examination reveals suspicious injuries, and the pediatrician has a reasonable suspicion that a child has been abused, a report to [a Child Protective Service agency] for further investigation is mandated by law,” according to a recent article in Pediatrics.7

Pediatricians should know how to get in touch and work with local child abuse and neglect teams located at children’s hospitals and in some counties, according to Dr. Shwayder.
Pediatricians don’t always need parental consent to evaluate children for potential abuse. Many states have laws permitting physicians to evaluate children who are suspected victims of abuse, to conduct tests, and to take photographs of children’s injuries without parental consent.7
Even when families might abandon pediatricians who report suspected child abuse, it is important that those pediatricians do not abandon these families. Pediatricians can be of great assistance to children, nonoffending parents, and family members during such times of crisis. They can help interpret children’s injuries for Child Protective Service agencies and law enforcement investigators. Pediatricians might also be required to testify in trial proceedings.12
In addition to detecting child abuse affecting individual patients, pediatricians can help to prevent abuse by advocating for funding and the implementation of evidence-based prevention programs in their communities, states, and at the national level.7
NEXT: Questions and clues checklist
References
1. Stephenson T. Bruising in children. Curr Paediatr. 1995;5:225-229.
2. Kos L, Shwayder T. Cutaneous manifestations of child abuse. Pediatr Dermatol. 2006;23(4):311-320.
3. Sheets LK, Leach ME, Koszewski IJ, et al. Sentinel injuries in infants evaluated for child physical abuse. Pediatrics. 2013;131(4):701-707.
4. McDonald KC. Child abuse: approach and management. Am Fam Physician. 2007;75(2):221-228.
5. Children’s Bureau. Administration for Children and Families. Child Maltreatment 2013. January 15, 2015. http://www.acf.hhs.gov/programs/cb/resource/child-maltreatment-2013. Accessed August 5, 2015,
6. Committee on Child Abuse and Neglect, American Academy of Pediatrics. When inflicted skin injuries constitute child abuse. Pediatrics. 2002;110(3):644-645.
7. Christian CW; Committee on Child Abuse and Neglect, American Academy of Pediatrics. The evaluation of suspected child physical abuse. Pediatrics. 2015;135(5):e1337-e1354.
8. Rosenberg LA. Effects of maltreatment on the child. In: Wissow LS, ed. Child Advocacy for the Clinician: An Approach to Child Abuse and Neglect. Baltimore, MD: Williams & Wilkins, 1990:12.
9. Anderst JD, Carpenter SL, Abshire TC; Section on Hematology/Oncology and Committee on Child Abuse and Neglect of the American Academy of Pediatrics. Evaluation for bleeding disorders in suspected child abuse. Pediatrics. 2013;131(4):e1314-e1322.
10. Oranje A, Bilo RA. Skin signs in child abuse and differential diagnosis. Minerva Pediatr. 2011;63(4):319-325.
11. Pierce MC, Kaczor K, Aldridge S, et al. Bruising characteristics discriminating physical child abuse from accidental trauma. Pediatrics. 2010;125(1):67-74.
12. Committee on Medical Liability and Risk Management. Policy statement-Expert witness participation in civil and criminal proceedings. Pediatrics. 2009;124(1):428-438.
Ms. Hilton is a medical writer who has covered health and medicine for 25 years. She resides in Boca Raton, Florida. She has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.