Cystic Fibrosis: Classic Radiographic Findings
1. The chest radiographs (Figure 1) of a 9-year-old child reflect the classic findings of a particular disease. Among other findings, the size of the patient's heart is_____? A. Enlarged. B. Small to normal. C. Consistent with early failure. 2. If you were to see calcifications in the abdomen (none are present in this case), they would probably be caused by which of the following? A. Previous adrenal hemorrhage. B. Gallstones. C. Splenic granulomas. 3. Is there evidence of hyperinflation? A. Yes . B. No. 4. Do you see acute findings? A. Yes. B. No. C. Cannot be determined. 5. Which of the following organisms are common culprits in this condition? A. Pseudomonas aeruginosa. B. Burkholderia cepacia. C. Staphylococcus aureus. D. All of the above, and then some.
1. The chest radiographs (Figure 1) of a 9-year-old child reflect the classic findings of a particular disease. Among other findings, the size of the patient's heart is_____?
A. Enlarged.
B. Small to normal.
C. Consistent with early failure.
2. If you were to see calcifications in the abdomen (none are present in this case), they would probably be caused by which of the following?
A. Previous adrenal hemorrhage.
B. Gallstones.
C. Splenic granulomas.
3. Is there evidence of hyperinflation?
A. Yes .
B. No.
4. Do you see acute findings?
A. Yes.
B. No.
C. Cannot be determined.
5. Which of the following organisms are common culprits in this condition?
A. Pseudomonas aeruginosa.
B. Burkholderia cepacia.
C. Staphylococcus aureus.
D. All of the above, and then some.
Answer & Discussion: The radiographs show classic findings of cystic fibrosis (CF).
1. The chest radiographs (see Figure 1) of a 9-year-old child reflect the classic radiographic appearance of CF. Among other findings, the size of the patient's heart is small to normal. (B is the correct choice.
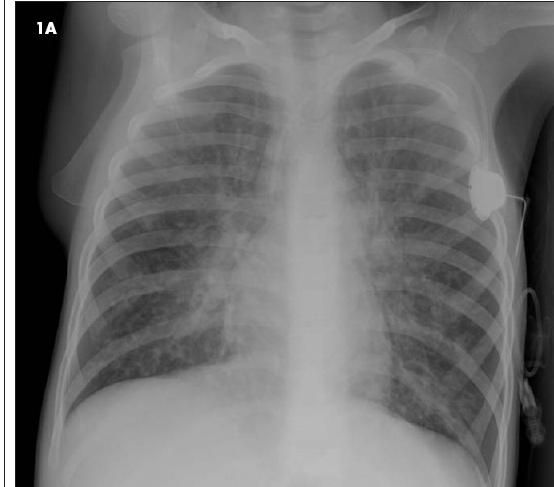
Figure 1
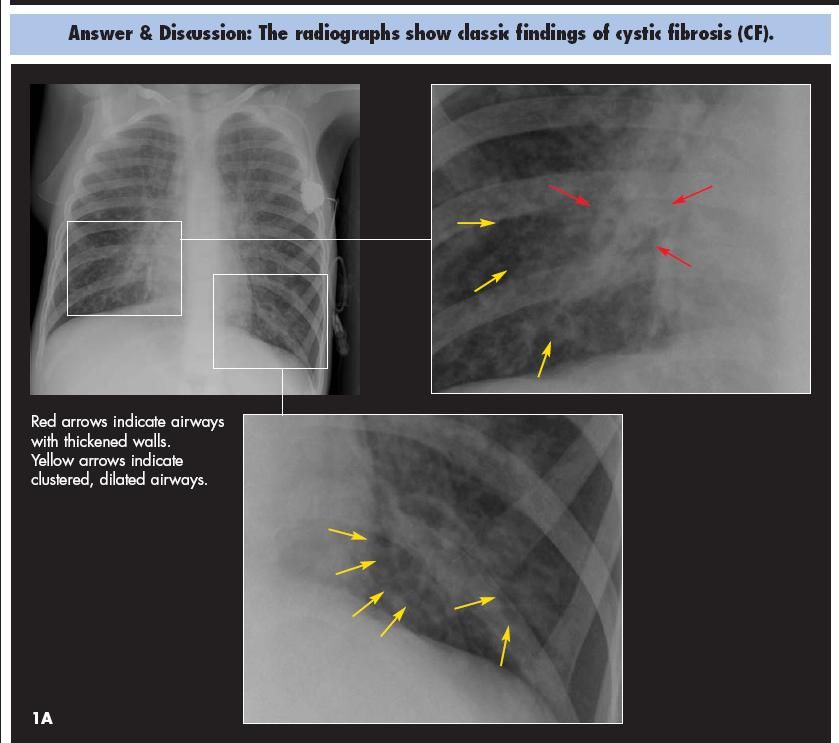
Figure
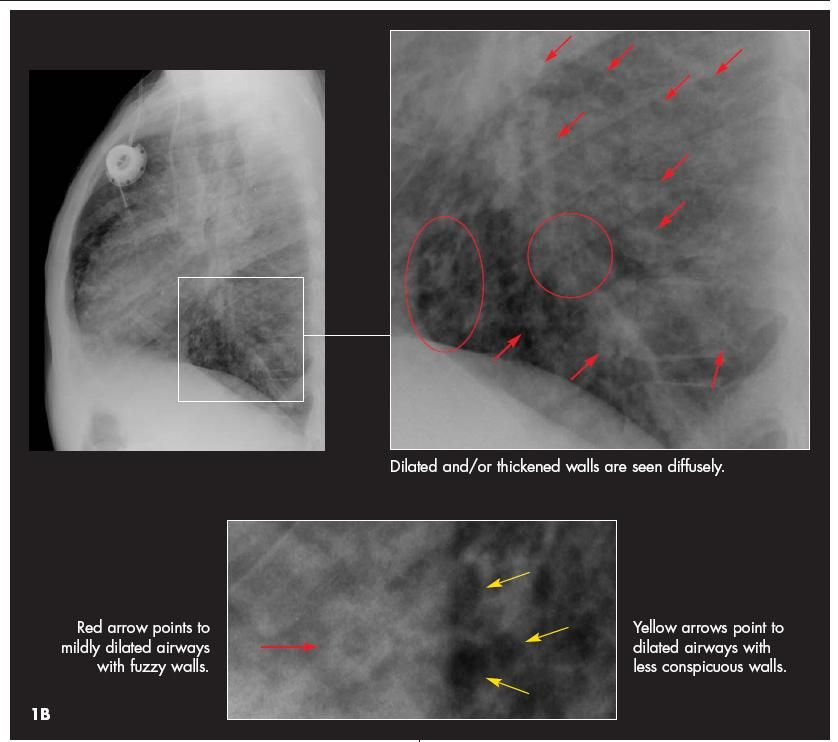
Figure
Figure
The patient's heart is probably of normal size, but the hyperexpansion commonly seen in patients with CF may make it seem relatively small. This phenomenon is frequently observed in older patients with emphysematous lungs. A small cardiac silhouette may also be seen in patients with asthma. The finding of microcardia could also suggest a hypovolemic state in other patients.
Other common radiographic and cross-sectional imaging (CT) findings of CF include focal atelectasis with or without hyperaeration, bronchiectasis seen as dilated tubular tracts or end-on with a cystic appearance, parahilar streaky opacities, peribronchial thickening, and mucous plugging.
Remember that patients with advanced CF may have enlarged pulmonary arteries from pulmonary arterial hypertension. Furthermore, copious hemoptysis is an uncommon but life-threatening development when pulmonary pathology encroaches on neighboring bronchial arteries, which themselves often demonstrate compensatory enlargement and tortuosity.
Other findings of end-stage CF include emphysema, pneumothorax, and cor pulmonale. Hypertrophic pulmonary osteoarthropathy is another rare entity that may be seen but is beyond the scope of this discussion.
2. If you were to see calcifications in the abdomen (none are present in this case), they would probably be caused by gallstones. (B is correct.)
Patients with CF not infrequently experience gallbladder complications, such as stones, which may be apparent on plain radiographs. The gallbladder of a patient with CF may also be small, contain sludge, demonstrate poor contractility, or manifest chronic inflammation.
Other GI problems related to CF include endocrine and exocrine pancreatic insufficiency (many patients are insulin-dependent), fatty infiltration of the liver, frank cirrhosis, and uncomplicated or complicated meconium ileus. The list of GI complications also includes meconium ileus equivalent (now called distal intestinal syndrome), gastroesophageal reflux disease, mucous distention of the appendix, intussusception, rectal prolapse, and colonic strictures. The development of colonic strictures in patients with CF has a strong association with use of high-strength pancreatic supplements. Many of the other manifestations of CF in the GI tract ultimately can be traced back to a common origin of inspissated mucus and its tendency to obstruct smaller channels.
3. Is there evidence of hyperinflation? The answer is yes. (A is correct.)
If the frontal view isn't enough to persuade you (count the 10 to 11 posterior ribs on the frontal view), take a look at the lateral view. The diaphragms are nearly completely flattened and there is a barrel shape appearance to the chest that results from anterior expansion (the anterior clear space) and bowing.
4. Do you see acute findings?
It can be difficult to tell whether there are acute findings on a particular single radiograph when seen in isolation. Careful comparison with earlier chest radiographs is essential to determine which area of parenchymal opacification is new amid the scarring, atelectasis, and architectural distortion. Sometimes acute findings (such as an acute lobar pneumonia) are obvious; often enough, they are not. This is why radiologists refer to the comparison radiograph as their "best friend." ("Old is gold.")
The radiograph shown here (see Figure 1) was interpreted without the benefit of earlier films at our institution. Thus, the presence of acute findings cannot be determined. (C is the correct choice.) Although no acute findings are suspected, a more confident interpretation would be possible if earlier films had been submitted for comparison.
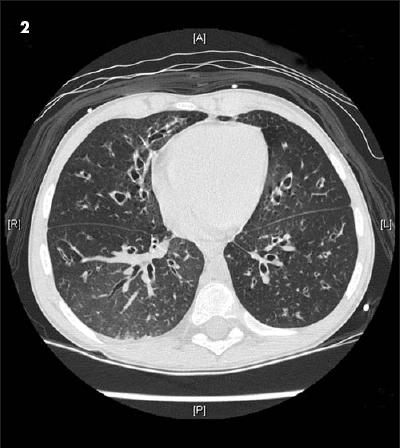
A chest CT scan obtained several weeks later (Figure 2) demonstrates in more detail the bronchiectasis and hyperinflation seen on the radiographs. Note the thickened walls of the airways, which can also be appreciated on the lateral view of the initial radiographs. Look for the fuzzy "cheerios," which represent the airways seen end-on, with thickened/inflamed walls.
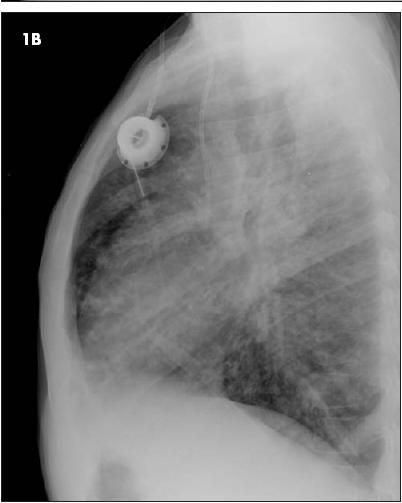
Figure 2
5. Which of the following organisms are common culprits in CF? Pseudomonas aeruginosa, Burkholderia cepacia, and Staphylococcus aureus are among the pathogens commonly associated with CF. (D is the correct answer.)
We all learned early on that CF is associated with P aeruginosa infection. The pathogen involved is not garden-variety Pseudomonas, however: it is a sticky mucoid variant that most patients with CF harbor indefinitely. Occasionally, infectious exacerbations are beaten back into submission with antibiotic therapy.
The frequency and duration of pulmonary infections affects decisions about vascular access. In the patient featured in this case, a chest port was placed in anticipation of long-term access needs.
Other infections that commonly afflict patients with CF are B cepacia, S aureus, Haemophilus influenzae, Stenostrophomonas maltophilia, and Aspergillus in its allergic form, which results in extensive mucous plugging of the airways. Non-tuberculous mycobacteria has also emerged as a problem for those with CF.
SUMMARY
The life expectancy of patients with CF continues to improve; in the earlier part of the 20th century many CF patients did not live to see their 10th birthday. Today, many patients survive into their 40s. Early diagnosis and attentive clinical management make a big difference in the lives of these patients.
BONUS QUESTION
From a genetic standpoint, CF is __________________?
A. Autosomal recessive.
B. Autosomal dominant.
C. Sporadic.
While most clinicians know that CF is an autosomal recessive disorder (A is correct) that affects the cells' chloride channel (the most common mutation to the cystic fibrosis transmembrane regulator [CFTR] is known as delta F508), it is also useful to remember that there are numerous variations of the specific genetic defect and plenty of variability in the phenotypic expression as well. Some patients have primarily GI complications, and the severity of pulmonary disease is also highly variable. A small percentage of patients retain a certain degree of pancreatic function.