Cystic fibrosis: An essential update
The prognosis for patients with cystic fibrosis (CF) continues to improve because of a combination of advances in the understanding of disease pathophysiology, implementation of early screening and diagnosis, and greater emphasis on proactive management to prevent deterioration and disease progression.
Medical writing support provided by Crystal Murcia, PhD
The prognosis for patients with cystic fibrosis (CF) continues to improve because of a combination of advances in the understanding of disease pathophysiology, implementation of early screening and diagnosis, and greater emphasis on proactive management to prevent deterioration and disease progression.
Cystic fibrosis is the most common life-shortening genetic disease among Caucasians, who represent 94% of the CF population in the United States.1 The probability of a Caucasian child being born with CF is approximately 1 in 2500.2 By comparison, the likelihood of CF in the Hispanic American and African American populations are 1 in 13,500 and 1 in 15,100 live births, respectively. It is estimated that there are currently 70,000 individuals living with CF worldwide, 30,000 of whom reside in the United States.1 Children account for more than half of the CF population. The number of affected Americans continues to increase as new cases are diagnosed (approximately 1000 per year) and improvements in treatment and diagnosis enhance longevity. Indeed, within the past 20 years, the predicted median survival age for patients with CF has increased by more than 10 years (Table 1).1

Cystic fibrosis is an autosomal recessive disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. The CFTR protein was first classified as a chloride channel, but has subsequently been shown to facilitate or regulate the transport of other ions, such as sodium (through the epithelial sodium channel), thiocyanate, and bicarbonate.3,4 The CFTR protein is present in the epithelia of various tissues, including that of the lungs, sweat glands, gastrointestinal tract, vas deferens, and pancreas, where it helps regulate salt and water absorption and excretion.5
Disease-causing mutations in the CFTR gene impede protein production, stability, or activity, resulting in less available functional protein.4 In the lung, the ensuing perturbations in ion transport cause airway surface liquid depletion resulting in defective mucociliary clearance. Added to this is an abnormal inflammatory response, whose relation to the ion transport abnormality is unclear. Together, these physiologic changes lead to an iterative cascade of obstruction, inflammation, infection, and, ultimately, progressive, irreversible lung damage.3
Other manifestations of dysfunctional CFTR include pancreatic insufficiency resulting from ductal obstruction, meconium ileus because of increased viscosity of intestinal mucus, and congenital bilateral absence of the vas deferens (CBAVD) caused by obstruction of the Wolffian ducts during fetal development.5,6 The influence of CFTR mutations on nonrespiratory organ systems affects growth, nutritional status, and fertility, but it is the lung disease that is predominantly responsible for CF-related morbidity and mortality.7
Newborn screening
One of the keys to improvements in CF outcomes has been the increasing adoption of a proactive approach to care, which includes the broad implementation of newborn screening (NBS). According to data from the Cystic Fibrosis Foundation Patient Registry, more than 61% of CF diagnoses in the United States in 2012 were made through NBS.1 The rationale for instituting NBS programs is to mitigate the negative impact of untreated CF on lung structure and function and to prevent nutritional deterioration by providing appropriate monitoring and treatment.

It has long been known that infants with pancreatic insufficiency due to CF demonstrate poor growth and inadequate weight gain. Researchers are now beginning to appreciate that structural changes of the lungs have already begun to manifest within the first year of life in affected individuals.8,9 Lung disease is generally not clinically apparent at these early stages because these nascent structural and physiologic abnormalities (eg, bronchial dilatation, bronchial wall thickening, gas trapping) and bacterial infections are usually asymptomatic during infancy.8
Identification of patients through NBS has been associated with improved nutritional status, better cognitive function, improved pulmonary status/lung function, and fewer hospitalizations.10-14 Newborn screening also has the potential to decrease the risk of life-threatening complications and death in infancy, and to reduce treatment costs.7,15 Indeed, comparisons with historical data indicate an increased probability of survival into early adulthood for those diagnosed as the result of NBS.12 For parents, the expedited time to diagnosis reduces distress and provides opportunities for genetic counseling, which could influence future childbearing decisions.7
Screening for CF is currently offered as a component of NBS programs in all 50 states. The CF screening programs are a multistep process that begins with the measurement of immunoreactive trypsinogen (IRT) levels in blood taken from the newborn heel prick. This pancreas-derived enzyme is typically elevated in all patients with CF, even those who are pancreatic sufficient. However, levels in the normal range may be present in infants with CF who present with meconium ileus.10
Meconium ileus is the first symptom of CF in approximately 15% to 20% of affected newborns.7 Given the association with CF, it is recommended that all newborns who have meconium ileus (or any small bowel obstruction, even if it is not clearly recognized as meconium ileus) are administered a sweat test regardless of findings on the IRT screen.10 Elevations in IRT that are not associated with CF may be detected in infants who experience perinatal stress or who have a low birth weight. African American infants may also demonstrate elevated IRT levels compared with Caucasian infants, which could result in a false-positive NBS.
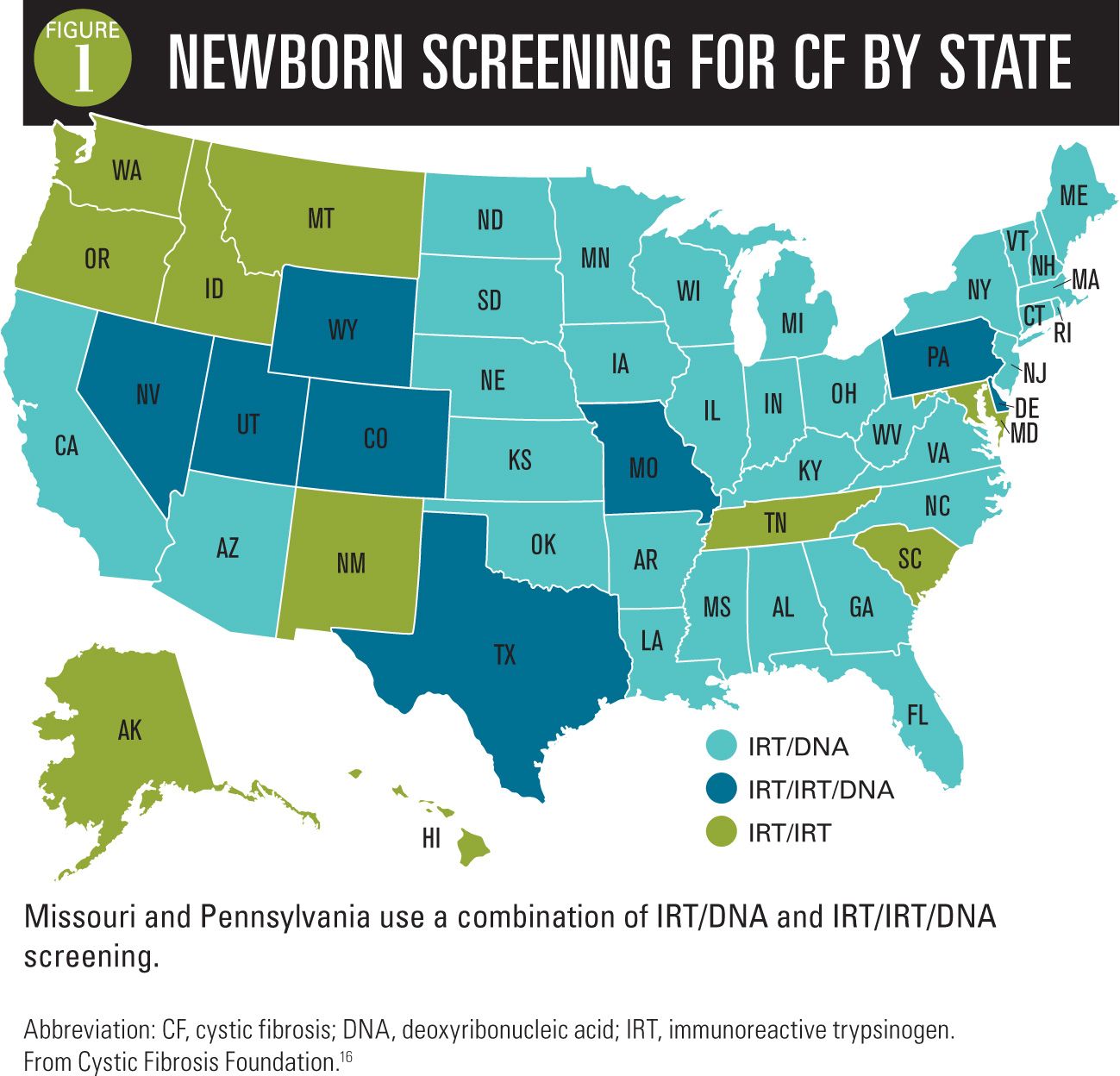
The method for further assessment after finding an elevated IRT varies by state (Figure 1).16 There are 4 NBS methods used in the United States. The most widely used approach, IRT/DNA, begins with IRT measurement when the infant is 1 or 2 days old. If the IRT level on the initial blood spot is elevated (eg, in the 96th percentile), that same blood spot is tested for CFTR mutations from a predefined panel of the most common mutations. If even 1 mutation is found, the infant is referred for sweat testing, because no panel includes all mutations.
The second most common approach is IRT/IRT, for which the IRT assay is performed on blood specimens collected at age 1 to 2 days, then repeated again at approximately 2 weeks of age. Two elevated IRTs constitute a positive NBS for CF and indicate that a sweat test needs to be performed. A third approach, IRT/IRT/DNA, uses slightly lower thresholds for the IRT cutoff compared with the IRT/IRT method, but then checks the blood of children with 2 elevated IRT measurements for common CFTR mutations. Finally, the state of California uses a variation on the IRT/DNA approach in which gene sequencing rather than a screening panel is used when an elevated IRT is found, eliminating the role of sweat testing as a confirmatory test.
In all states other than California, the definitive diagnosis is made through sweat testing. Sweat collection is performed using pilocarpine iontophoresis and followed by measurement of chloride levels. This noninvasive procedure can be reliably performed once the infant reaches 72 hours of age. It should be noted that infants who are premature, weigh less than 2 kg, or who are African American have a higher likelihood of producing insufficient quantities of sweat for testing.10
A sweat chloride value of 60 mEq/L or greater is considered diagnostic for CF.10,17 A result of 30 to 59 mEq/L is indeterminate but is often due to the presence of a CFTR mutation that has residual chloride channel function.17 Beyond the age of 6 months, the indeterminate range for sweat chloride is 40 to 59 mEq/L. Patients with an indeterminate test result should undergo periodic retesting until test results are unequivocal or the presence of symptoms solidifies the diagnosis.17 Sweat testing should be performed at an accredited CF care center in order to be considered reliable. Cystic fibrosis care centers are supported by the Cystic Fibrosis Foundation and offer specialized care for children and/or adults with CF. A complete listing of CF care centers is available through the foundation’s website.
Implementation of NBS has not been without its challenges. These issues generally fall into 3 categories: 1) lack of primary care physician (PCP) familiarity with the process; 2) breakdown of communication between healthcare providers and affected families; and 3) difficulties in administering or interpreting test results. Many of the issues related to the latter point can be resolved by ensuring that sweat testing is performed at a Cystic Fibrosis Foundation-accredited laboratory facility.
Aside from problems in the execution of the program, there have been several unintended consequences of CF NBS, including inconveniencing large numbers of families of children who initially screen positive but who are eventually found to be healthy by requiring them to travel long distances for sweat testing; identification of CFTR mutation carriers, which may lead to confusion and misconceptions in the absence of adequate genetic counseling; and the detection of patients with CFTR mutations of unclear significance, which can lead to unnecessary worry and other psychological consequences. Communication and education prior to and following sweat testing may provide some relief from the emotional toll and distress that accompany a positive NBS result.
Variation in presentation and severity
More than 1900 mutations in CFTR have been identified and different mutation classes are associated with variable compromise in CFTR function. As a result, there is great variation in presentation and disease severity. Lung disease, in particular, is influenced by a complex interaction with a variety of modifier genes and environmental exposures.
A major distinguishing feature among patients with CF is the categorization of exocrine pancreatic function. Patients who are pancreatic insufficient require supplementation with pancreatic enzymes to aid digestion and promote normal growth and development. These patients experience gastrointestinal symptoms such as gas, loose stools, and abdominal pain as a result of fat malabsorption. Pancreatic insufficiency is present in more than 80% of CF patients. It may not always be found at the time of CF diagnosis, but susceptible patients will develop it over the first year of life.7 The minority of patients who are pancreatic sufficient tend to have a CF phenotype with less pulmonary involvement because their mutations retain some residual CFTR function, but this tendency is not invariable. Pancreatic sufficient patients are prone to the development of pancreatitis, and those with recurrent pancreatitis may sometimes acquire late pancreatic insufficiency.
One of the complicating consequences of NBS programs is the identification of patients with CFTR mutations who do not fulfill the diagnostic criteria for CF. An infant who displays elevated IRT levels in the presence of A) fewer than 2 CFTR mutations and intermediate sweat chloride measurements, or B) normal sweat chloride measurements and 2 CFTR mutations of which no more than 1 is known to cause CF, is considered to have CFTR-related metabolic syndrome (CRMS; Table 2).18

Infants with CRMS show no clinical manifestations of CF other than an elevated IRT.19 However, they may develop symptoms later in childhood or adulthood and the effects may be limited to a single organ system.20 There are patients with CRMS in whom signs or symptoms associated with CF will never develop. However, given the potential for CF or CFTR-related disorders, ongoing monitoring is recommended.18
Lack of weight gain; loose stools, gas, or constipation of greater than 2 weeks in duration; stomach pain; or coughing or wheezing that lasts for more than 2 weeks in children with CRMS should trigger consultation with a CF specialist. Although treatments typically prescribed for patients with CF are of uncertain benefit for children with CRMS, guidelines do suggest monitoring for and treatment of Pseudomonas aeruginosa if it is detected in airway cultures.
Physicians should distinguish CRMS from another condition typically diagnosed later in life, CFTR-related disorder, which is characterized by mild clinical manifestations of CF in association with mutations in the CFTR gene (Table 3). Patients with this diagnosis typically present with male infertility (because of CBAVD), chronic or recurrent sinusitis, recurrent pancreatitis, and/or late development of bronchiectasis. A CFTR-related disorder is diagnosed by the presence of 1 or more of these traits (or by the presence of a sibling with CF), along with a sweat chloride test result in the intermediate range and detection of fewer than 2 CFTR mutations that are known to be disease causing.

Treatment
Innovations in therapies for CF have contributed to the improvements in life expectancy that have been observed over the past 30 years (Figure 2). However, arguably the most important advance in CF treatment has been the shift in focus from reactive to proactive treatment of the nutritional and pulmonary manifestations of disease.

Depending on the clinical and patient characteristics, maintenance therapy may entail a combination of careful attention to nutrition; use of pancreatic enzymes and multivitamin supplementation; physical and pharmacologic techniques for augmenting airway clearance; inhaled antibiotics; and anti-inflammatory medications (Table 4). Aerobic exercise is recommended as a complement to airway clearance techniques and has the additional benefits of improving physical, heart, and muscle strength.21

Systemic antibiotics are added when respiratory symptoms suggesting a pulmonary exacerbation develop, with close follow-up to ensure resolution. The exception is azithromycin, which has been shown to improve lung function and reduce the occurrence of exacerbations. This is thought to be due to anti-inflammatory rather than antimicrobial effects. Azithromycin is recommended for chronic use primarily in patients with persistent P aeruginosa airway infection who are not infected with nontuberculous mycobacteria.22 Aerosolized antibiotics are used in the eradication of newly acquired P aeruginosa infections and as chronic therapy of persistent infection. Their use minimizes systemic exposure and toxicity, but they are less effective in acute infection because of poor penetration into obstructed airways.
The newest addition to the maintenance therapy armamentarium, ivacaftor (Kalydeco; Vertex Pharmaceuticals; Boston, Massachusetts), is unique in several respects. Ivacaftor is the first pharmaceutical agent to specifically target defective CFTR.23 Ivacaftor potentiates CFTR chloride channel function by increasing the amount of time that the CFTR channel is open and transporting chloride ions. It is specifically effective for the 5% of CF patients with CFTR mutation classes in which the molecule locates to the apical cell membrane, and is not yet approved by the US Food and Drug Administration for children aged younger than 6 years.23
The potential to expand ivacaftor indications to non-G551D mutations is currently being explored, as is the use of other CFTR-targeted investigational agents, such as lumacaftor and ataluren. Regulatory approval is being sought for lumacaftor based largely on positive results from 2 phase III studies in which lumacaftor was combined with ivacaftor in patients homozygous for the F508del mutation.24
Role of the pediatrician
Pediatricians are important members of the CF care team, from the initial screening through monitoring of patients during childhood and adolescence. Pediatricians/PCPs are the first source of support and education for the parents of infants with positive NBS results. As such, they must be able to explain the results and implications of a positive NBS result; provide general disease state information about CF; describe the next steps in terms of diagnostic evaluations; discuss the possible outcomes of sweat testing and their likelihood; and develop a plan with the family for follow-up after the sweat test.10 The pediatrician/PCP is also vital to early referral to a CF care center for infants with positive NBS results or children who develop signs and symptoms characteristic of CF.
Patients with diagnosed CF will have routine visits at a CF care center. However, particularly during the first years of life, a child will have frequent interactions with his or her pediatrician as well. These touch points are opportunities to evaluate the child for disease-related symptoms and reinforce adherence to therapy, which is an ongoing challenge for patients with CF. The presence of respiratory symptoms are of potential concern as they may signal a pulmonary exacerbation (Table 5). The common cold, which is endemic in childhood, has a greater propensity to develop into a lower respiratory tract infection in children with CF compared with unaffected children.7 Moreover, viral infections often will be associated with bacterial complications that benefit from antibiotic therapy. The frequency of respiratory symptoms and infections increases with age. Consultation with a CF specialist is advised for children with CF who show respiratory signs or symptoms.

Patients who are diagnosed with CRMS require routine evaluation for indicators of disease progression. Although many of these children will remain healthy, an unknown number will develop a CFTR-related disorder or overt CF.18 These patients will be followed periodically by the CF care center (once or twice a year), but their physicians will need to be aware of possible disease manifestations (Tables 1 and 2). If signs or symptoms develop, the patient should be referred back to the CF care center. Clinicians also are challenged with regard to explaining CRMS to parents of an apparently healthy child. The Cystic Fibrosis Foundation offers guidance for discussing CRMS with the family of affected patients.
Vigilant monitoring is also encouraged for newborns that demonstrate an intermediate sweat test result.10 These patients should undergo a second test 1 to 2 months after the first assessment. In the interim, the pediatrician/PCP should closely observe the infant’s nutritional status and growth for evidence of pancreatic insufficiency. Respiratory symptoms in these patients should prompt immediate action.
Despite the generally high sensitivity and specificity of NBS programs for detecting individuals with clinically relevant CFTR mutations, false-negative results do occur.25 These patients risk delayed diagnosis if CF is not considered because of a negative NBS finding.10 In infants, symptoms suggestive of CF may include failure to thrive, excessive appetite, and abnormal stools, along with the classic respiratory symptoms such as persistent cough, frequent lung infections, wheezing, and dyspnea. Patients who present with symptoms suggestive of CF should be referred for sweat testing even if their NBS is known to have been negative. Early diagnosis of CF is crucial to preserving lung health and preventing adverse outcomes.
Summary
Improvements in CF care over the last several decades have led to a greatly improved prognosis. Advances in patient management have resulted from both the availability of new medications and the institution of proactive care before overt disease is manifest. Newborn screening programs present a logical extension of this philosophy. Pediatricians have the ability to maximize the benefits of diagnostic and treatment advances by providing family education and counseling, identifying patients with CFTR dysfunction early in the course of the disease, monitoring affected and at-risk children, and working in collaboration with CF care centers.
REFERENCES
1. Cystic Fibrosis Foundation. Cystic Fibrosis Foundation Patient Registry 2012 Annual Data Report. Bethesda, Maryland; 2013.
2. American Lung Association. State of Lung Disease in Diverse Communities 2010. Washington, DC: American Lung Association; 2010.
3. Cohen-Cymberknoh M, Shoseyov D, Kerem E. Managing cystic fibrosis: strategies that increase life expectancy and improve quality of life. Am J Respir Crit Care Med. 2011;183(11):1463-1471.
4. Clancy JP, Jain M. Personalized medicine in cystic fibrosis: dawning of a new era. Am J Respir Crit Care Med. 2012;186(7):593-597.
5. Barrett PM, Alagely A, Topol EJ. Cystic fibrosis in an era of genomically guided therapy. Hum Mol Genet. 2012;21(R1):R66-R71. Erratum in: Hum Mol Genet. 2013;22(9):1911.
6. van der Doef HP, Kokke FT, van der Ent CK, Houwen RH. Intestinal obstruction syndromes in cystic fibrosis: meconium ileus, distal intestinal obstruction syndrome, and constipation. Curr Gastroenterol Rep. 2011;13(3):265-270.
7. Grosse SD, Boyle CA, Botkin JR, et al. Newborn screening for cystic fibrosis: evaluation of benefits and risks and recommendations for state newborn screening programs. MMWR Recomm Rep. 2004;53(RR-13):1-36.
8. Sly PD, Brennan S, Gangell C, et al; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF). Lung disease at diagnosis in infants with cystic fibrosis detected by newborn screening. Am J Respir Crit Care Med. 2009;180(2):146-152.
9. Stick SM, Brennan S, Murray C, et al; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF). Bronchiectasis in infants and preschool children diagnosed with cystic fibrosis after newborn screening. J Pediatr. 2009;155(5):623.e1-628.e1.
10. Comeau AM, Accurso FJ, White TB, et al; Cystic Fibrosis Foundation. Guidelines for implementation of cystic fibrosis newborn screening programs: Cystic Fibrosis Foundation workshop report. Pediatrics. 2007;119(2):e495-e518.
11. Rosenfeld M, Emerson J, McNamara S, et al; EPIC Study Group Participating Clinical Sites. Baseline characteristics and factors associated with nutritional and pulmonary status at enrollment in the cystic fibrosis EPIC observational cohort. Pediatr Pulmonol. 2010;45(9):934-944.
12. Dijk FN, McKay K, Barzi F, Gaskin KJ, Fitzgerald DA. Improved survival in cystic fibrosis patients diagnosed by newborn screening compared to a historical cohort from the same centre. Arch Dis Child. 2011;96(12):1118-1123.
13. Venkata JA, Jones KL. Benefits of newborn screening for cystic fibrosis in Shreveport, Louisiana, Cystic Fibrosis Center. J La State Med Soc. 2011;163(6):316-319.
14. Martin B, Schechter MS, Jaffe A, Cooper P, Bell SC, Ranganathan S. Comparison of the US and Australian cystic fibrosis registries: the impact of newborn screening. Pediatrics. 2012;129(2):e348-e355.
15. Doull IJ, Ryley HC, Weller P, Goodchild MC. Cystic fibrosis-related deaths in infancy and the effect of newborn screening. Pediatr Pulmonol. 2001;31(5):363-366.
16. Cystic Fibrosis Foundation. Newborn screening for cystic fibrosis. http://www.cff.org/GetInvolved/Advocate/NewbornScreening/. Accessed September 24, 2014.
17. Farrell PM, Rosenstein BJ, White TB, et al; Cystic Fibrosis Foundation. Guidelines for diagnosis of cystic fibrosis in newborns through older adults: Cystic Fibrosis Foundation consensus report. J Pediatr. 2008;153(2):S4-S14.
18. Cystic Fibrosis Foundation, Borowitz D, Parad RB, et al. Cystic Fibrosis Foundation practice guidelines for the management of infants with cystic fibrosis transmembrane conductance regulator-related metabolic syndrome during the first two years of life and beyond. J Pediatr. 2009;155(6 suppl):S106-S116.
19. Ren CL, Desai H, Platt M, Dixon M. Clinical outcomes in infants with cystic fibrosis transmembrane conductance regulator (CFTR) related metabolic syndrome. Pediatr Pulmonol. 2011;46(11):1079-1084.
20. Schram CA. Atypical cystic fibrosis: identification in the primary care setting. Can Fam Physician. 2012;58(12):1341-1345, e1699-e1704.
21. Flume PA, Robinson KA, O'Sullivan BP, et al; Clinical Practice Guidelines for Pulmonary Therapies Committee. Cystic fibrosis pulmonary guidelines: airway clearance therapies. Respir Care. 2009;54(4):522-537.
22. Mogayzel PJ Jr, Naureckas ET, Robinson KA, et al; Pulmonary Clinical Practice Guidelines Committee. Cystic fibrosis pulmonary guidelines. Chronic medications for maintenance of lung health. Am J Respir Crit Care Med. 2013;187(7):680-689.
23. Flume PA, Van Devanter DR. State of progress in treating cystic fibrosis respiratory disease. BMC Med. 2012;10:88.
24. Two 24-week phase 3 studies of lumacaftor in combination with ivacaftor met primary endpoint with statistically significant improvements in lung function (FEV1) in people with cystic fibrosis who have two copies of the F508del mutation [press release]. Available at: http://investors.vrtx.com/releasedetail.cfm?ReleaseID=856185. Published June 24, 2014. Accessed September 24, 2014.
25. Dunn CT, Skrypek MM, Powers AL, Laguna TA. The need for vigilance: the case of a false-negative newborn screen for cystic fibrosis. Pediatrics. 2011;128(2):e446-e449.
Dr Schechter is professor of pediatrics, Virginia Commonwealth University (VCU), and chief, Division of Pulmonary Medicine, Children’s Hospital of Richmond at VCU, Richmond, Virginia. He discloses research support from Vertex Pharmaceuticals and Novartis, and consulting for Vertex, Gilead Sciences, Novartis, Genentech, and Celtaxsys. In addition, he has served on data safety monitoring committees for AstraZeneca and Bayer.