Determining whether a skin injury could be physical abuse
How can you distinguish intentionally inflicted injuries from findings not caused by abuse?
Determining whether a skin injury could be physical abuse
By Jean Labbé, MD
Skin injuries, the most frequent manifestation of physical abuse of a child, may be found fortuitously during any medical visit. How can you distinguish intentionally inflicted injuries from findings not caused by abuse?
Most physicians include the possibility of physical abuse in their differential diagnosis when they are seeing a child for trauma. They should do the same when the physical exam of a child presenting for a reason other than trauma leads to discovery of suspicious skin injuries. Skin injuries are the most frequent sign of physical abuse: More than 90% of victims present with this type of injury.1 Minor skin injuries are more frequent than major lesions in victims of abuse.2
Very young children deserve particular attention. They are defenseless, more vulnerable to blows, completely dependent, demanding, and lack the language skills to verbalize their condition. Some spend their time mainly at home and so are rarely in contact with adults other than their parents.*
* In this article, the term "parents" refers not only to birth or adoptive parents but also to any person responsible for the care of a child.
How can abusive skin injuries be distinguished from other manifestations in a child who is not being seen specifically for those injuries (trauma)? What attitude should you take toward parents during the visit? What must you do when physical abuse is suspected? These questions and their answers are the subject of this article.
Clinical approach
The diagnosis of physical abuse is not easy to establish. Pathognomonic signs are rare. There is an important overlap between the appearance of most injuries caused by abuse and the appearance of injuries from other causes. The child may be too young to talk or may keep his secret out of fear of the consequences of disclosure. Most abusive parents lie when questioned about the origin of their child's injuries.
Abuse is a sensitive issue that can make physicians uneasy because such cases easily raise emotions that can interfere with clinical judgment. The risk of the situation getting out of hand is real. Alleging abuse when, it turns out, none exists can lead to an unpleasant sociojudiciary investigation of innocent parents. At worst, their child could be taken away from them.
On the other hand, missing a case of abuse can lead to recidivism that may be more serious than the previous abuse and could even cause the death of a child. Because the consequences of a false negative (not suspecting abuse when abuse actually exists) are potentially more serious than those of a false positive (suspecting abuse when there actually is none), the protection of the child must be considered paramount.
It is not the pediatrician's responsibility to establish proof that a child is being maltreated; that is the role of child protective services (CPS). The pediatrician has only to establish a presumptive diagnosis, based on indicators. Once there is "reasonable suspicion" of physical abuse, the physician is legally obligated to make a report to CPS.3
To establish a presumptive diagnosis, the physician gathers data using familiar methods: history, observation, examination, and complementary tests, as needed. When dealing with a sensitive issue such as suspected maltreatment, the physician must be careful not to be swayed by subjective impressions and to instead seek the most objective data possible.
History. The history is obviously oriented to the reason for consultation. Once suspicious skin injuries are detected, however, the history must be completed by asking for an explanation of those injuries. If the child is able to talk, ask him questions directly in an open style: "I see that you have an injury here. How did it happen?" For children without verbal skills, direct questions to the parent. When your suspicion is high, it is preferable to question the people present at the consultation separately.
Candor is called for in all cases. When you face a parent who is wondering why you are paying so much attention to a skin injury, explain that, when such an injury looks like trauma, it is always important to determine its origin. Keep the tone of your questioning neutral and professional. Remember: You are not a police officer; you do not have to prove that a crime was committed or identify an aggressor. Your questioning is only a means of finding an explanation for an injury. Even in cases that are clearly, or very suspect of, maltreatment, you must take a supportive, nonaccusing approach to parents, without revealing your emotions.
Some skin injuries that appear suspicious are found, upon investigation, to be the result of other causes, such as a medical condition. Personal and family antecedents are important for determining whether the child has a hereditary coagulation disorder. During the review of systems, verify whether the child bruises easily, suffers nosebleeds, or bleeds profusely when accidentally cut. It is also imperative to ask whether the child is taking medication, because certain drugs (detailed later) can cause the patient to bruise easily.
In some cases of abuse, the people accompanying the child may not be aware that abuse has taken place. In other situations, when the parent present is the aggressor, he often has a difficult personal history himself that explains his actions, while not excusing them. Taking a social history of the family allows you to identify risk factors such as stress at home (social isolation, poverty, substance abuse, acute crisis). The American Academy of Pediatrics' Committee on Child Abuse and Neglect recommends routine screening of all women for abuse at the time of the well-child visit.4 This screening is even more relevant when there is a strong suspicion of abuse of a child, because child abuse and conjugal violence are often present together.5 When the mother accompanies the child, you may introduce the topic in the following manner (with the child out of the room): "In my practice, I now ask all parents, in a systematic manner, questions about family violence, because it affects their health and safety and that of their children. Have you ever been threatened or injured by your partner?"
Observation. During the visit, observe the attitude of the parents and the child as well as their interactions. If the child is crying or in discomfort, does the parent attempt to console him? How does the parent react when the clinician discovers the injuries and questions him about the subject? Does the child look for the parent's approval before answering questions? Question the personnel of your office or clinic. They may have noteworthy observations about the parent-child interaction in the waiting room before the consultation.
Examination. The child's general appearance and cleanliness help reveal the quality of care at home. During routine medical checkups, systematically examine the entire body surface. During visits for other reasons, examine the entire body surface if you find any suspicious skin injury, in addition to performing an examination specific to the reason for the visit. The child does not have to be completely undressed at once but can be undressed a little at a time to preserve his comfort and sense of modesty. When suspicion of physical abuse of a baby is strong, the mouth and the fundi must be examined.
Complementary tests. In the case of multiple or severe bruises, a hematologic assessment is necessary. Initial laboratory tests should include a complete blood count (CBC), prothrombin time (PT), and activated partial thromboplastin time (aPTT). When physical abuse of a child less than 2 years of age is strongly suspected, a complete skeletal survey is indicated.
Establishing a presumptive diagnosis of physical abuse
Schmitt and Kempe devised a succinct explanation of child abuse: "The right parent, the right child, the right day."6 This expression reflects the risk factors elucidated by various epidemiologic studies. It is important, however, to properly interpret the significance of these risk factors for each parent, child, and trigger situation (Tables 1 and 2). These factors increase the probability of physical abuse, and the risk of abuse increases with the number of risk factors identified. Risk factors should increase the physician's vigilance but must not be used as indicators of physical abuse. Many parents at risk never mistreat their children, because of the presence of protective factors that cancel the noxious influence of the risk factors. The opposite is also truecases of physical abuse can be found in situations in which there is no apparent risk. Consequently, it is important to avoid affirming or invalidating abuse based on whether or not the patient or parent fits the "profile" of an abused child or abusive parent.
TABLE 1
Risk factors for child abuse
In the parents
Previous abuse of another child
Lack of knowledge of normal child development and behavior
Antecedents of maltreatment in childhood
Poor impulse control
Aggressiveness
Young age
Single parent without support
Social isolation
Criminal record
Poverty
Mental illness
Mental retardation
Conjugal violence
History of substance abuse
In the child
Result of an unwanted pregnancy
Different from parental expectations
Born prematurely
Handicapped
Difficult or perceived as being so
Hyperactivity
Developmental delay
TABLE 2
Triggers for abuse
Acute illness of the child
Excessive crying
Nighttime awakenings
Feeding problems
Regurgitations
Oppositional behavior
Soiling in the period of potty training
Poor academic results
Conjugal conflict
Any acute crisis
The diagnostic process can be compared to a puzzle that is put together piece by piece, without knowing the final picture ahead of time. It is unnecessary to put all the pieces in place to guess the outcome, but the more pieces one has, the clearer the picture will be. Some pieces are more important than others to identify the picture. In the presumptive diagnosis of physical abuse, each indicator (Table 3) represents a piece of the puzzle. I am limiting the discussion here to indicators that apply to a child who is not presenting for trauma. A differential diagnosis is also essential to eliminate causes other than abuse that could explain the injuries.
TABLE 3
Indicators of physical abuse
Fortuitous discovery of a significant skin injury
Injuries suspicious of physical abuse
Multiple injuries of various ages
No history offered, or a changing or contradictory history, for the injuries
Injuries inconsistent with the history
Injuries inconsistent with the child's stage of development
Suspicious attitude in the parents
Suspicious attitude in the child
Injuries in different systems
History of unexplained trauma
Indicators of physical abuse
The physical findings, the history, and the behavior of the parents may provide tip-offs to the presence of abuse.
Fortuitous discovery of a "significant" skin injury.By "significant," I mean an injury requiring care for which most parents would consult a doctor (a laceration, wound infection, or deep or widespread burn, for example). It is suspicious to find such an injury for which there was no previous medical visit, especially if the care given appears inadequate. In cases of abuse, the parent may not have brought the child to the office in order to avoid having the true origin of the injury discovered.
Injuries suspicious of physical abuse. Barely 8% of skin injuries in victims are pathognomonic.1 These are recognizable marks such as imprints of objects used to hurt the child: fingers, hand, teeth, belt, cord, hot object, and so on (Figure 1). Finger imprints differ according to the type and duration of force. When fingertips are pressed forcefully into the skin, the force is applied steadily for a relatively long time and capillaries are ruptured at the site of pressure. This leaves round bruises that are recognizable by their linear distribution (Figure 2). With a hard slap, the force is applied for a very short period; blood is driven away from the site of impact and pressure in the capillaries increases abruptly in the spared areas between the fingers. Fine parallel lines of bruises result from the ruptured capillaries, showing the outlines of the fingers (Figure 3).



Circumferential marks around the wrists and the ankles suggest the use of bonds. Adult bites can be identified by their double-arc shape and the distance between the canines (more than 3 cm). "Punched out" circular burns are typical of intentional contact with a cigarette (Figure 4).

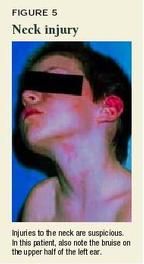
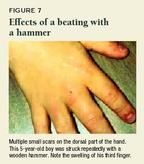
In the absence of obvious signs of abuse, certain skin injuries are suspicious because they have been described predominantly in victims of abuse. Pay attention to injuries to the face and head, outer ears, neck (Figure 5), thorax, abdomen, lumbar region, buttocks, genital organs, and inner part of the thighs.2,7,8 Lesions on the forearms may testify to an attempt by the child to protect himself from blows. Bruises of unusual size may suggest abuse (Figure 6).9 Bilateral injuries as well as multiple scars are also suspicious (Figure 7). 10,11

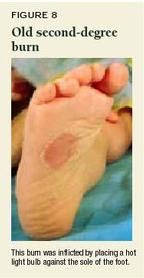
Also pay attention to burns in children younger than 3 years old. Certain locations are suspicious: places normally protected by clothing, the backs and palms of the hands, the soles of the feet (Figure 8), the perineum, genital organs, and buttocks. Also suspicious are burns that are multiple, bilateral, symmetrical, deep, or uniform, or that have a clearly defined edge. Stocking and glove scalding burns without splash marks are characteristic of nonaccidental injury.
Multiple injuries of various ages, such as healed wounds along with newer ones, are a classic indicator of abuse. In the case of bruises, however, it is difficult to assess their age. Experience has shown us that characteristics of recent bruises (well-defined, uniform reddish-blue color, painful, swollen) are different from those of old bruises (multicolored, indistinctive edge, absence of swelling and pain). But dating bruises precisely is a hazardous task. Charts indicating the date of bruises according to their color are unreliable. Numerous factors, apart from the age of bruises, affect their appearance: the quantity of blood, the depth under the skin surface, the vascularity of the underlying tissue, and the color of the skin.12 It takes at least 18 hours before a bruise takes on a yellow hue.13 However, it is often difficult to precisely determine the predominant color of a bruise.14 In a recent study, pediatricians' estimation of the age of bruises using three categories (less than 48 hours, 48 hours to seven days, and more than seven days) was accurate in only 76% of cases. Their estimates of bruise age within 24 hours were accurate in only 48% of cases.15
No history offered; changing or contradictory history. This indicator is not necessarily useful with minor skin injuries that have gone unnoticed by the parents. It is, however, important to consider in the presence of significant injuries in any child or bruises in a young baby.
Injuries inconsistent with the history.Explanations may not correspond with the observed injuries because they are not in accord with the laws of physics and biomechanics or because they contradict observations made in studies on documented unintentional injuries. When a child falls, we expect injuries to appear at the site of impact and to be proportional to the energy absorbed by the tissues at the moment of impact. This energy depends on numerous factors, such as the speed of the impact, the surface upon which impact is made, the angle of the fall, and so on. A fall from a height, therefore, would not explain multiple injuries on parts of the body that are not close together. In all but fewer than 3% of cases, even a fall down the stairs would not cause injuries to more than one site (Figure 9).16

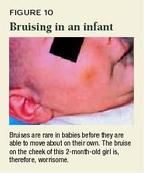
Injuries incompatible with the child's stage of development.With any injury, the stage of development of the child must be considered. Bruises are very rare in babies before they are able to move about on their own (Figure 10).17 The same can be said for all other injuries, with the exception of scratches on the face. A 1-year-old cannot turn on the hot water faucet in the bathtub. A child accused of having injured another child must have the muscular strength to inflict such an injury.
Suspicious attitudes in the parents or child.The behavior of the parents must draw the examiner's attention when it appears unusual to the circumstances. It is important, however, to distinguish between inappropriate attitudes and those that are a reaction to a difficult situation (extreme fatigue, acute stress). Some of the behaviors of the child, too, can be warning signs (Table 4).
TABLE 4
Attitudes that should raise suspicion of child abuse
In the parents
Aggressiveness, provocation
Excessive criticism of the child
Lack of empathy (e.g., does not attempt to comfort their crying child)
Unrealistic expectations for the child
Preoccupation with their needs rather than those of the child
Excessive control of the child (e.g., prevents the child from answering questions)
Accusing another child of causing the injuries
Visibly under the influence of alcohol or drugs
In the child
Hypervigilance
Fear
Passivity
Aggressiveness
Mistrust
Depressed look
Injuries in different systems.The discovery of a skin injury in a baby should lead to a search for injuries elsewhere (in the mouth, of the bones, etc.). Injuries discovered fortuitously in different systems (for example, suspicious bruises and fractures found in the same patient) is a very specific indicator supporting physical abuse.
A history of unexplained trauma.More than three consultations a year for injuries that require medical attention is considered suspicious.18 It is not easy to bring this indicator to light, however, because abusive parents tend to seek consultations in different places to avoid attention.
Differential diagnosis
A number of conditions and causes should be considered when evaluating suspicious skin injuries.
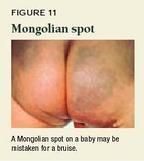
Skin marks resembling trauma.Certain medical conditions can resemble bruises (Mongolian spots, erythema multiforme, and vasculitis, for example), injuries (dermatographism, stretch marks), burns (bullous impetigo, toxic photodermatitis, diaper rash), or pulled hair (alopecia areata, tinea capitis) (Figures 11 and 12).19,20

Rare petechiae (one or two spots only) can be found in normal babies, particularly on the thorax, abdomen, and lower limbs.21 They can also be found in abundance on the face after crying, efforts to vomit, or coughing.
Disorders or medication that contribute to traumatic injuries. It is well known that certain medical conditions (hereditary coagulation disorders, idiopathic thrombocytopenic purpura, leukemia) can cause children to bleed easily (Figure 13). These children display larger and more numerous bruises. Some patients bruise easily without having an evident disorder (purpura simplex); this condition is reported mostly in adults, particularly in women 20 to 30 years of age.22

Some commonly used drugs can cause easy bruising by any of several mechanisms: thrombocytopenia, impairment of platelet function, or hypersensitivity vasculitis (Table 5).23,24
TABLE 5
Some commonly used drugs and classes of drugs that can cause purpura
Acetaminophen
Ampicillin
Aspirin
Barbiturates
Carbamazepine
Cephalosporins
Chemotherapy agents
Chloral hydrate
Chlorpromazine
Cimetidine
Clindamycin
Ethambutol
Furosemide
Ganciclovir
Gentamicin
Glyceryl guaiacolate
Ibuprofen
Imipramine
Indomethacin
Insulin
Nafcillin
Naproxen
Penicillin
Phenytoin
Propranolol
Pseudoephedrine
Ranitidine
Sulfonamides
Trimethoprim- sulfamethoxazole
Valproic acid
Unintentional injuries. Children hurt themselves almost daily by falling down and hitting themselves on objects. Their injuries are usually minor and do not require medical treatment. What do these unintentional injuries look like? To answer this question, I systematically examined the skin of children during 2,040 consecutive medical visits. 25 The number and type of injuries varied according to the age of the child and the time of year (in a temperate climate). I did not find any significant difference between boys and girls. Babies 8 months old or younger rarely had bruises, as could be expected because of their reduced mobility. The most frequent injuries in this age group were scratches on the face. None of the young babies had more than three cutaneous injuries at a time, regardless of the time of year. After the age of 9 months, three quarters of the children had at least one recent injury, 22% had at least five, 5% had at least 10, and less than 1% had 15 or more. The 5- to 9-year-olds had the most skin injuries. Bruises were predominant, followed by abrasions and scratches. Fewer than 2% of children presented with other types of recent injuries (lacerations, burns, bites).
In the warm seasons, children play outside more often and wear less protective clothing. They have twice as many skin injuries than in the winter and, although bruises remain predominant, they present with more abrasions and scratches.
Although any body site can be affected in unintentional trauma, injuries are found mainly on the lower limbs (shins, knees, thighs) (Figure 14), and the upper limbs (forearms, elbows). Certain sites are rarely affected. In our study, less than 2% of children had injuries to the thorax, abdomen, pelvis, or buttocks and less than 1% to the chin, ears, or neck.

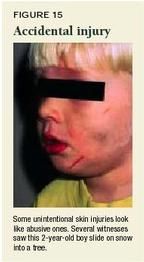
The history remains crucial for identifying unintentional injuries, because their appearance or location may be misleading (Figure 15). In the case of an accident, the history is usually clear, plausible, and does not vary over time or from one witness to another.
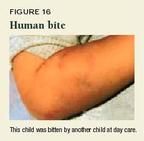
Inflicted nonabusive trauma. Children sometimes inflict injury on each other. These injuries are usually the result of fighting between children of the same age and at a similar stage of development (Figure 16). Children can also have trauma injuries that are self-inflicted. For example, children with trichotillomania pull out their hair. Self mutilation may be seen in children with certain genetic disorders (Cornelia de Lange syndrome, Lesch-Nyhan syndrome, familial dysautonomia), mental disorders (autism), developmental delay, and behavioral problems or personality disorders, as well as in children who are victims of abuse.
Cultural practices can also lead to skin injury suspicious of abuse.19,20 Cao gio (or coining) is a practice used in Southeast Asia to treat fever, chills, and headache. The skin on the back is massaged with mentholated oil and then rubbed vigorously with a coin or spoon, which results in linear bruises. Cupping is a very old therapeutic practice still used in Eastern Europe, Africa, and Mexico to treat various ailments. Usually, a heated cup is applied to the skin, creating suction, which can cause circular bruises or burns. Moxibustion is a traditional Chinese practice in which small amounts of the moxa herb, believed to draw out illness, are burned on the skin at the site of the symptoms. This practice causes patterned burns.
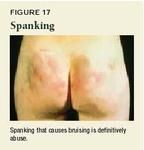
Three quarters of American children say they have been physically punished by their parents.26 The line of demarcation between acceptable physical punishment and an unacceptable act has changed with the times, and still varies according to culture. Today in North America, any physical punishment is considered abusive if it is more serious than redness caused by a slap and results in a mark that lasts more than 24 hours (Figure 17).27 In the view of child protective services, it is not the intention behind the aggression that counts but the consequences to the child.
Injuries can also be caused by domestic animals (scratches, bites), but they are usually not difficult to interpret.
Negligence. Some injuries result from accidents caused by blatant negligence (lack of supervision, exposure to a dangerous environment). In these cases, parents may lie about the circumstances of the accident to avoid being blamed. Evidence of negligence does not exclude the possibility of abuse. The occurrence of several types of maltreatment in a single child is common.
The clinician's conduct after the evaluation
Without a confession from the aggressor, the presence of an impartial witness at the time of the event, or a credible statement from the victim, the diagnosis of abuse remains an opinion. This opinion is more likely to be correct if it is based on specific and multiple indicators, which is why the situation must always be considered in its entirety. When enough pieces of the puzzle point to physical abuse, the physician must intervene. Waiting to be absolutely certain may put the safety of several children in danger. A report is not an accusation against the parents. You are simply asking for a consultation with CPS to confirm or negate your clinical impression.
Most hospitals in large cities have access to child abuse experts (mainly pediatricians) who can be consulted when your findings are difficult to interpret. It is of utmost importance that first-line pediatricians document appropriately the pertinent facts in the child's medical record.3 Describe each injury in specific termslength, width, shape, color, depth, and associated swelling.28,29 Draw and, ideally, photograph significant injuries. Include in the record the explanations for the injuries, specifying how they were obtained. If the child makes a verbal statement, document it verbatim in quote marks. If the attitude of the parents or the child is unusual, make note of it. It is advisable to write down observed facts (such as alcoholic breath, unsteady gait) rather than interpretations (parent under the influence of alcohol).
Remain vigilant, take appropriate action
Practitioners should make a habit of systematically examining a child's skin during routine medical checkups. In this manner, you may occasionally detect injuries suspicious of physical abuse. Patterned marks on the skin speak for themselves. In the absence of these pathognomonic signs, be alert to skin injuries presenting certain characteristics:
unusual location
>15 injuries
bruises in a baby younger than 9 months old
multiple injuries in sites other than the legs
multiple injuries in cold seasons (in a temperate region)
injuries other than bruises, abrasions, and scratches.
Obviously, each case is unique and the situation must be considered in its entirety. Are there other indicators supporting the diagnosis? Could these injuries have other causes? If there is a serious doubt, you must make a report to CPS.
REFERENCES
1. McMahon P, Grossman W, Gaffney M, et al: Soft-tissue injury as an indicator of child abuse. J Bone Joint Surg 1995;77:1179
2. Pascoe JM, Hildebrandt HM, Tarrier A, et al: Patterns of skin injury in nonaccidental and accidental injury. Pediatrics 1979;64:245
3. Krugman RD, Bross DC: Medicolegal aspects of child abuse and neglect. Neurosurg Clin NA 2002; 13:243
4. American Academy of Pediatrics: The role of the pediatrician in recognizing and intervening on behalf of abused women. Pediatrics 1998;101:1091
5. Edelson JL: The overlap between child maltreatment and woman battering. Violence Against Women 1999;5:34
6. Schmitt BD, Kempe CH: The pediatrician's role in child abuse and neglect. Curr Probl Pediatr 1975;5:3
7. Roberton DM, Barbor P, Hull D: Unusual injury? Recent injury in normal children and children with suspected non-accidental injury. Br Med J 1982;285:1399
8. Johnson CF: Injury variables in child abuse. Child Abuse Negl 1985;9:207
9. Dustan FD, Guildea ZE, Kontos K, et al: A scoring system for bruise patterns: A tool for identifying abuse. Arch Dis Child 2002;86:330
10. Laing SA: Bilateral injuries in childhood: An alerting sign? Br Med J 1977;2:1355
11. Schachner LA, Hankin D: Assessing child abuse in the dermatologist's office. Adv Dermatol 1988;3:61
12. Stephenson T: Ageing of bruising in children. J R Soc Med 1997;90:312
13. Langlois NEI, Gresham GA: The ageing of bruises: A review and study of the colour changes with time. Forensic Sci Intern 1991;50:227
14. Munang LA, Leonard PA, Mok JYQ: Lack of agreement on color description between clinicians examining childhood bruising. J Clin Forens Med 2002;9:171
15. Bariciak ED, Plint AC, Gaboury I, et al: Dating of bruises in children: An assessment of physician accuracy. Pediatrics 2003;112:804
16. Joffe M, Ludwig S: Stairway injuries in children. Pediatrics 1988;82:457
17. Sugar NF, Taylor JA, Feldman KW: Bruises in infants and toddlers. Those who don't cruise rarely bruise. Arch Pediatr Adolesc Med 1999;153:399
18. Reece RM, Grodin MA: Recognition of nonaccidental injury. Pediatr Clin North Am 1985;32:41
19. Scales JW, Fleischer Jr AB, Sinal SH, et al: Skin lesions that mimic abuse. Contemporary Pediatrics 1999;16(1):137
20. Pride HB: Child abuse and mimickers of child abuse. Adv Dermatol 1999;14:417
21. Downes AJ, Crossland DS, Mellon AF: Prevalence and distribution of petechiae in well babies. Arch Dis Child 2002;86:291
22. Sham RL, Francis CW: Evaluation of mild bleeding disorders and easy bruising. Blood Rev 1994;8:98
23. Baselga E, Drolet BA, Esterly NB: Purpura in infants and children. J Am Acad Dermatol 1997; 37(5pt1):673
24. Bick RL: Platelet function defects associated with hemorrhage or thrombosis. Med Clin N Am 1994; 78:577
25. Labbé J, Caouette G: Recent skin injuries in normal children. Pediatrics 2001;108:271
26. Finkelhor D, Dziuba-Leatherman J: Children as victims of violence: A national survey. Pediatrics 1994;94:413
27. American Academy of Pediatrics: When inflicted skin injuries constitute child abuse. Pediatrics 2002;110:644
28. Butts JD: Injuries: Description, documentation, evidence issues. NCMJ 1994;55:423
29. Lambert WF, Grant P: Recognizing cutaneous signs of child abuse. Curr Opin Pediatr 1992;4:638
DR. LABBÉ is a pediatrician with Direction de Santé Publique and a professor in the department of pediatrics at Laval University, Québec, Canada. He has nothing to disclose in regard to affiliation with, or financial interests in, any organization that may have an interest in any part of this article.
KEY POINTS
Skin injuries of abusive origin
- Most skin injuries caused by abuse are minor.
- Recognizable imprints are pathognomonic, but they are rare.
- Skin injuries with the following characteristics are considered "suspicious": unusual location, >15 injuries, bruises in a baby less than 9 months old, multiple injuries in sites other than the legs, multiple injuries in the cold seasons (in a temperate region), injuries other than bruises, abrasions, and scratches.
- The risk factors for abuse are not diagnostic.
- The medical evaluation must not be limited to the injuries; it must also include a search for other indicators of physical abuse as well as a differential diagnosis.
- Waiting to be absolutely certain before making a report to child protective services is not recommended; reasonable suspicion is sufficient to prompt such a report.
Jean Labbe. Determining whether a skin injury could be physical abuse. Contemporary Pediatrics December 2003;20:27.