Dying to be thin: Body image and disordered eating
This article briefly discusses theories on why poor body image develops and the strong link to disordered eating; ways to screen for poor body image and eating disorders in children and adolescents; and some efforts under way to prevent and intervene in children at risk of, or who have developed, poor body image.
During the developmental years of childhood and adolescence, as these young people pass through various stages in establishing self-identity, how they view their own bodies in the context of family, peers, and the larger culture has a profound influence on their physical and emotional well-being.
Recommended: Using family-based therapy to tackle disordered eating
Being overweight, or more importantly perceiving oneself as overweight, is a main driver of poor body image, particularly among adolescent girls. Data show that up to 50% of preadolescent girls report dissatisfaction with their bodies, and that this dissatisfaction may start well before puberty.1 Boys are not immune to this problem. Emerging data show just how rampant poor body image is among boys, regardless of sexual orientation.2,3
The effects of poor body image or body dissatisfaction are well known, particularly in girls. One primary fallout is disordered eating, with reports showing that between 25% and 55% of 12-year-old girls report dieting, 14% report binge eating, and 48% report trying to control weight by fasting and using food substitutes.4
For girls, disordered eating is linked to a concern over appearance and striving toward the Western cultural ideal of thinness.1 For boys, disordered eating is linked to trying to achieve muscularity and leanness as seen as the ideal forms of masculinity.2 As such, disordered eating in boys is less about losing weight and more about gaining muscle and leanness. To this end, steroids, with concomitant adverse effects, are also frequently used by these boys.2
Along with disordered eating, obesity, chronic weight cycling, and depression are linked to poor body image. The need to address obesity is highlighted by statistics that show that about 17% (12.7 million) of children and adolescents aged 2 to 19 years are obese.5 In addition to the physical comorbidities that these young people face, such as diabetes, the poor body image these children develop because of their obesity or being overweight increases their risk of participating in high-risk behaviors such as substance abuse and risky sexual behavior.6
Early identification of children and adolescents at risk of developing poor body image is therefore critical to help prevent disordered eating and other associated maladaptive behaviors. Pediatricians, working with others involved with children’s lives including parents and school administrators, can help identify children at risk in the attempt and hope to prevent poor body image or intervene when it has already developed.
This article briefly discusses theories on why poor body image develops and the strong link to disordered eating; ways to screen for poor body image and eating disorders in children and adolescents; and some efforts under way to prevent and intervene in children at risk of, or who have developed, poor body image.
NEXT: The power of perception
Power of perception
Although being overweight and obese is a major driver of poor body image in girls, the perception of being overweight or obese (regardless of the reality) has an even stronger effect on body image.7 A 2009 survey of health behaviors in a national sample of girls in grades 5 to 10 in the United States found worse physical, emotional, school, and social health-related quality of life in girls who perceived themselves as overweight compared with those who actually were overweight.7
More: AAP shifts focus on child obesity
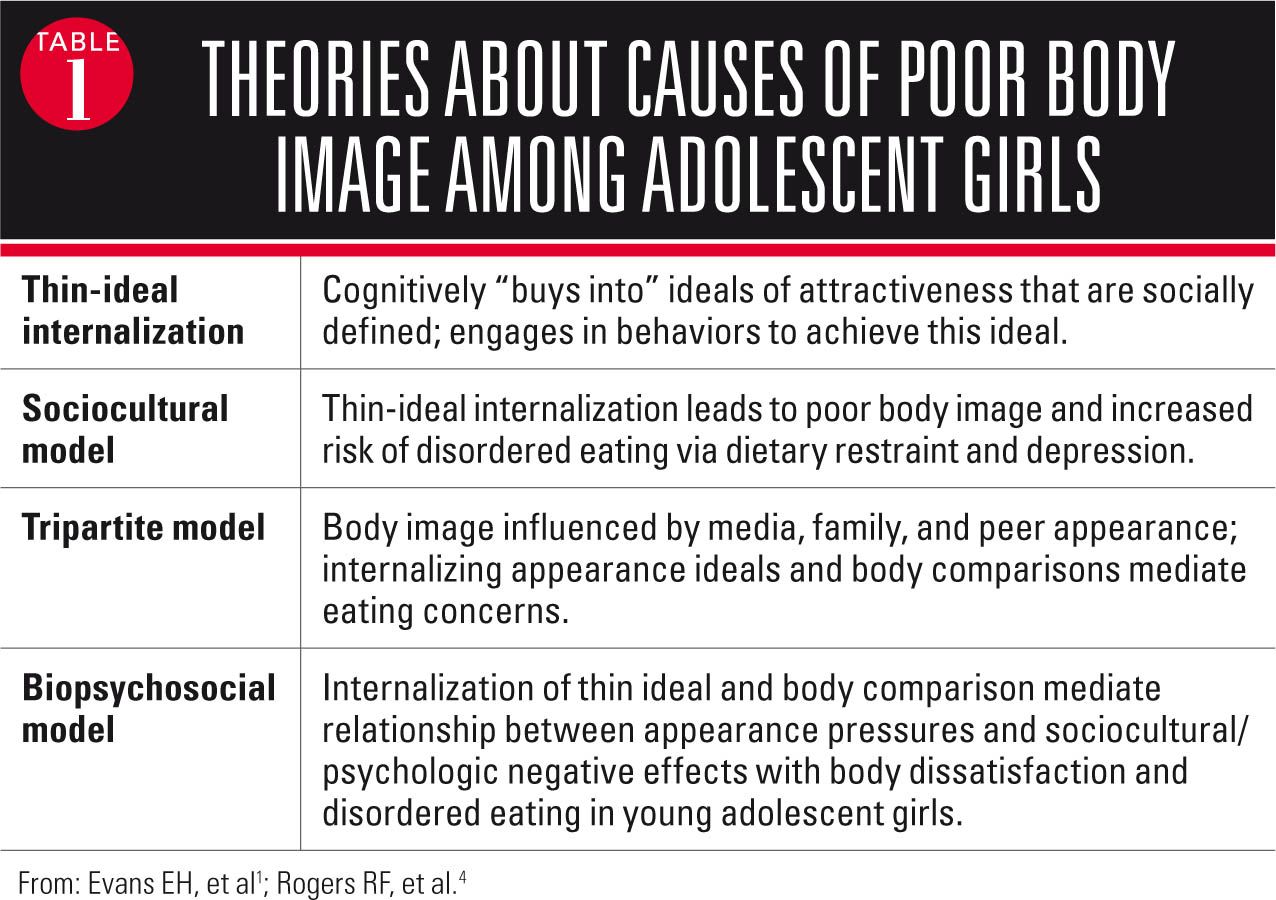
This finding points to the power of perception, supporting various theories of and empirical evidence showing how poor body image develops (Table 1).1,4 A common theme among these theories seems to be, particularly for girls, the effect on body image of internalizing cultural ideals of attractiveness that elevate thinness. For example, a theory aptly called the “thin-ideal internalization theory,” in which girls “buy into” ideals of attractiveness and engage in behaviors to achieve this ideal, has been validated in girls aged as young as 6 years. It also has been shown to partially mediate the relationship between body mass index and body dissatisfaction in girls aged 9 to 12 years.1,4
Other theories that, in various ways, highlight the effect of culturally mediated ideals of thinness on body image all point to the strong connection between disordered eating and poor body image. In this context, the link between poor body image and obesity or being overweight is easy to understand, as is the linkage with girls who perceive themselves as being overweight.
The implication of these findings is the need to target screening and intervention for children and adolescents at risk of developing poor body image, not only in children with the known risk factor of actually being overweight or obese but also in those who perceive themselves as being overweight.7 Another implication is the need to address cultural influences that reinforce thinness as the ideal body type.
NEXT: How to screen for poor body image
Screening for poor body image issues
Assessing risk factors for the development of poor body image is an important aspect of screening. Being overweight or obese is a known risk factor as stated previously. As also stated previously, however, the perception of being overweight and obese is an even greater risk factor for developing poor body image.
Among the risk factors that pediatricians can look for in their conversations with children and adolescents are those related to internalizing cultural ideals of physical attractiveness. Risk factors associated with negative body image include internalization of cultural appearance ideals, appearance-related conversations, appearance-related comparisons, and appearance-related teasing.8 All these risk factors influence how individuals perceive themselves in relation to one ideal or another.
Recommended: Care of the student athlete
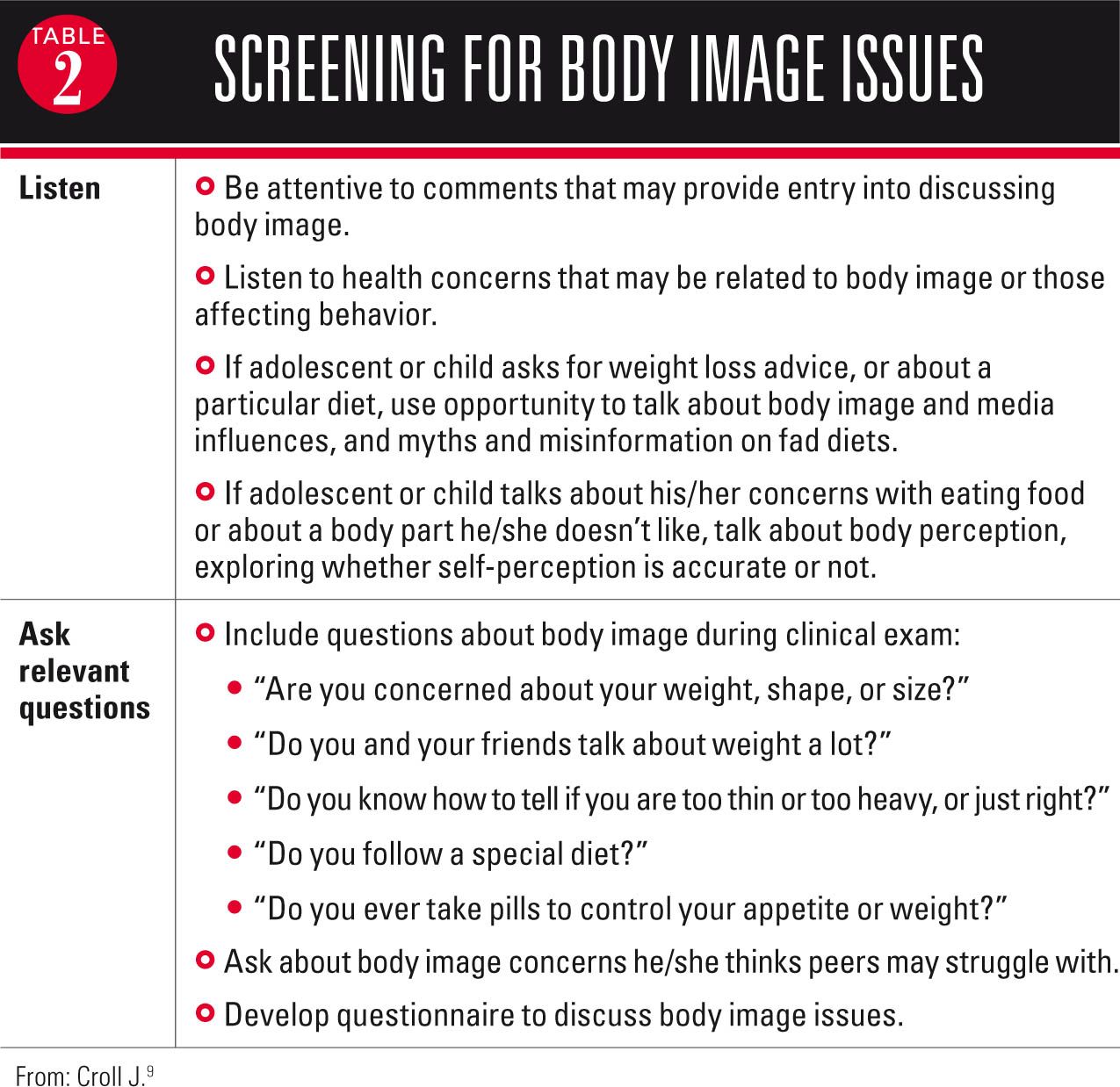
To recognize which children and adolescents may be more susceptible to poor body image based on these internalizing risk factors, pediatricians can listen carefully to how children and adolescents talk about themselves and also ask relevant questions to further uncover information that may reveal a risk for the development of poor body image (Table 2).9 Generating a conversation about body image issues during clinical exams can be done on a regular basis starting before puberty and into adulthood.9
NEXT: Looking at ways to prevent and intervene
Prevention and interventions
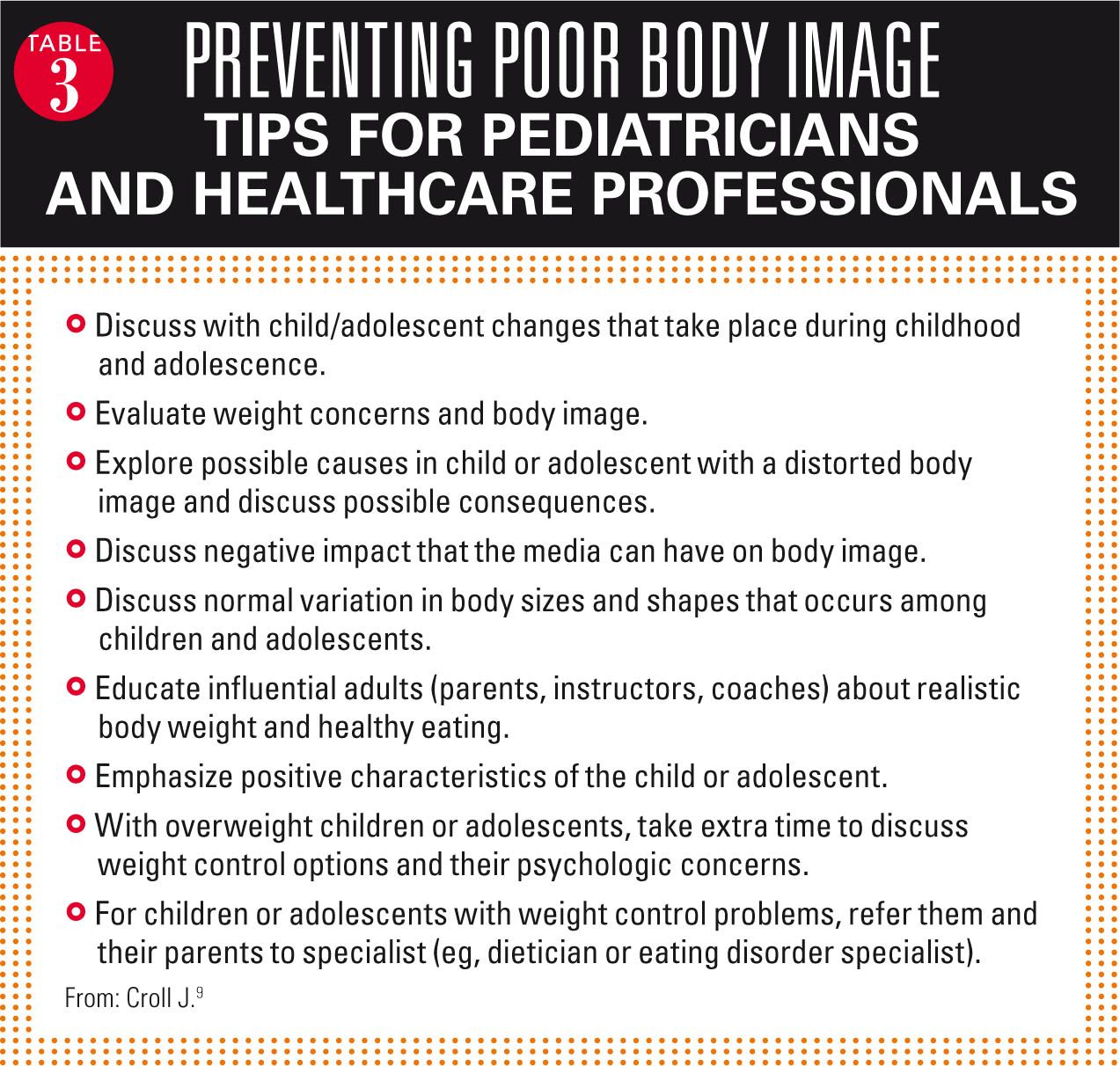
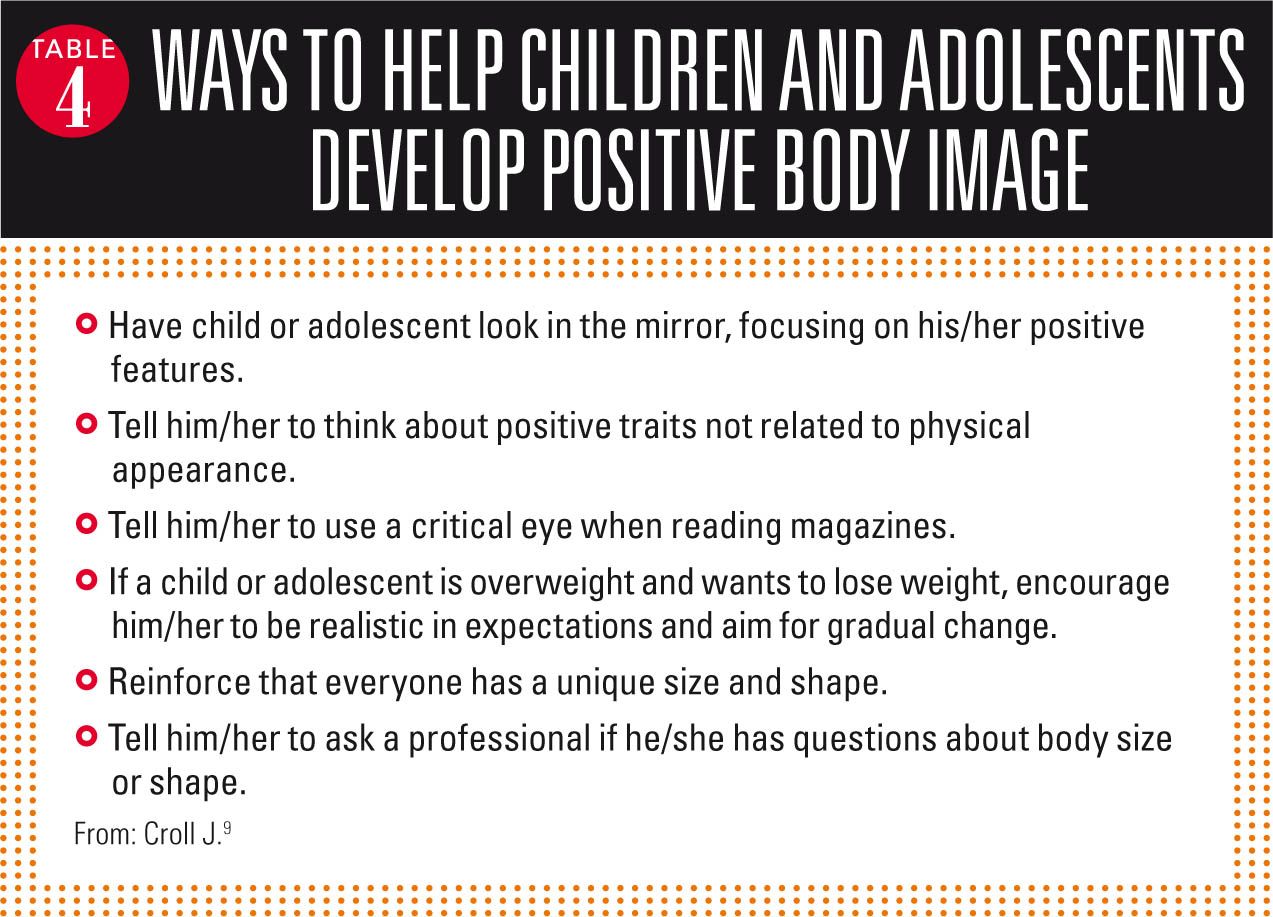
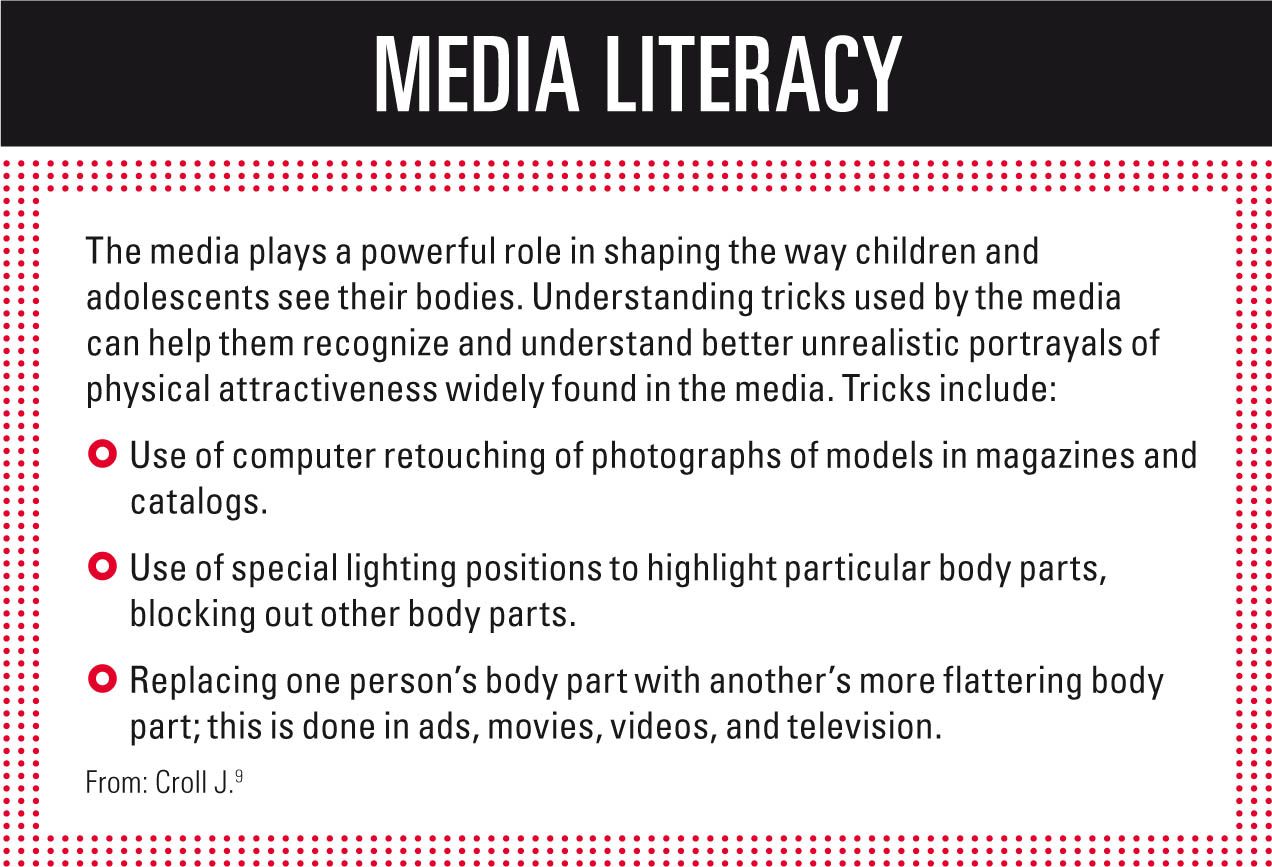
To help children and adolescents foster a positive body image and prevent a poor body image from developing, pediatricians and other healthcare professionals can provide needed information on issues that affect body image (Table 3).9 They also can encourage various activities and resources for children and adolescents to become better aware of their own perceptions of body image and the influences on those perceptions (Table 4).9 (See “Media literacy”9)
More: Using technology to combat kids' obesity
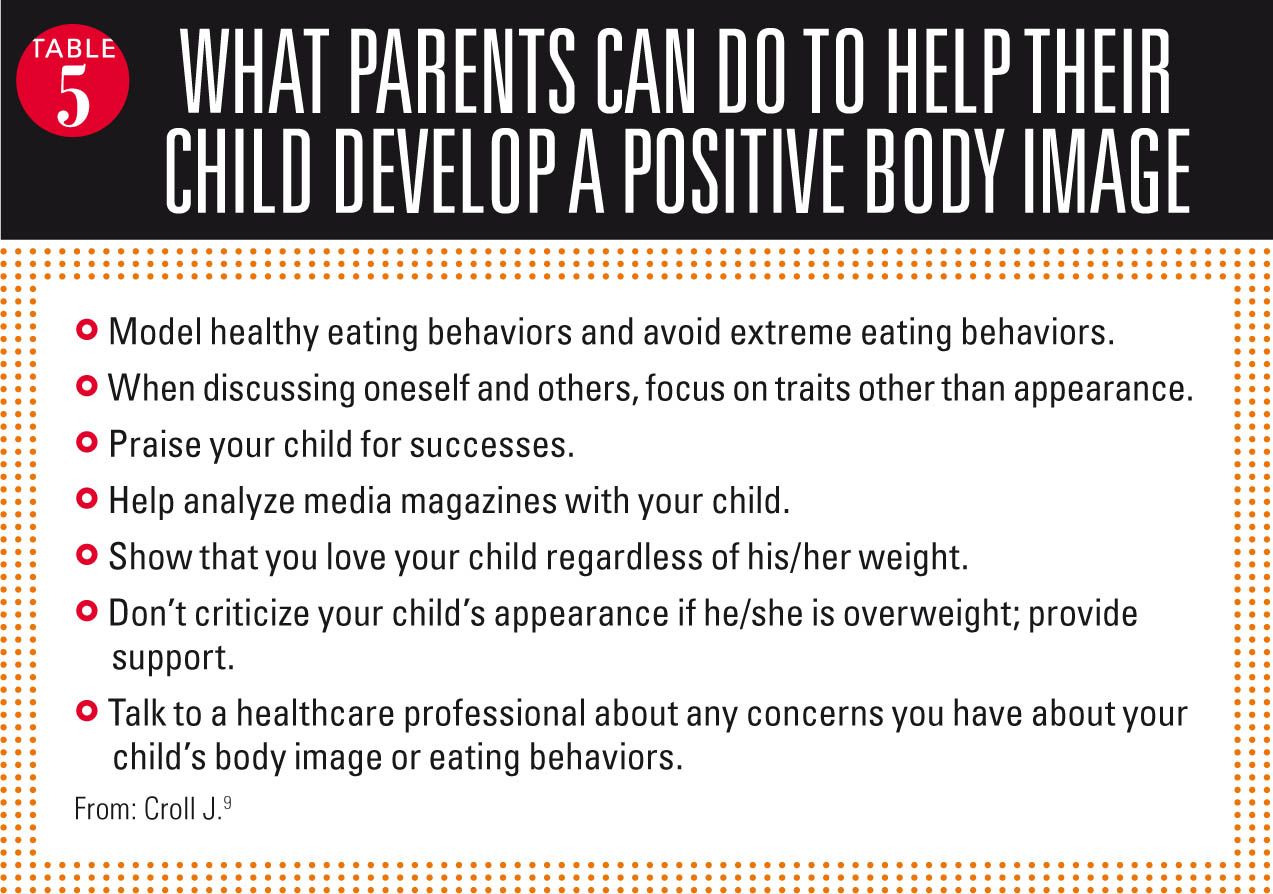
Critical to preventing poor body image is participation by parents. Although perception of one’s body, particularly of being overweight, is a major driver of poor body image, a recent study also showed a declining tendency by parents to perceive their children as overweight when in fact they are.10 Because parents play a critical role in shaping their child’s self-perception, parents need to be educated on the real risk of poor body image development in children who are overweight or obese. Table 5 provides a list that can be given to parents to help them better educate their children on positive body image.9
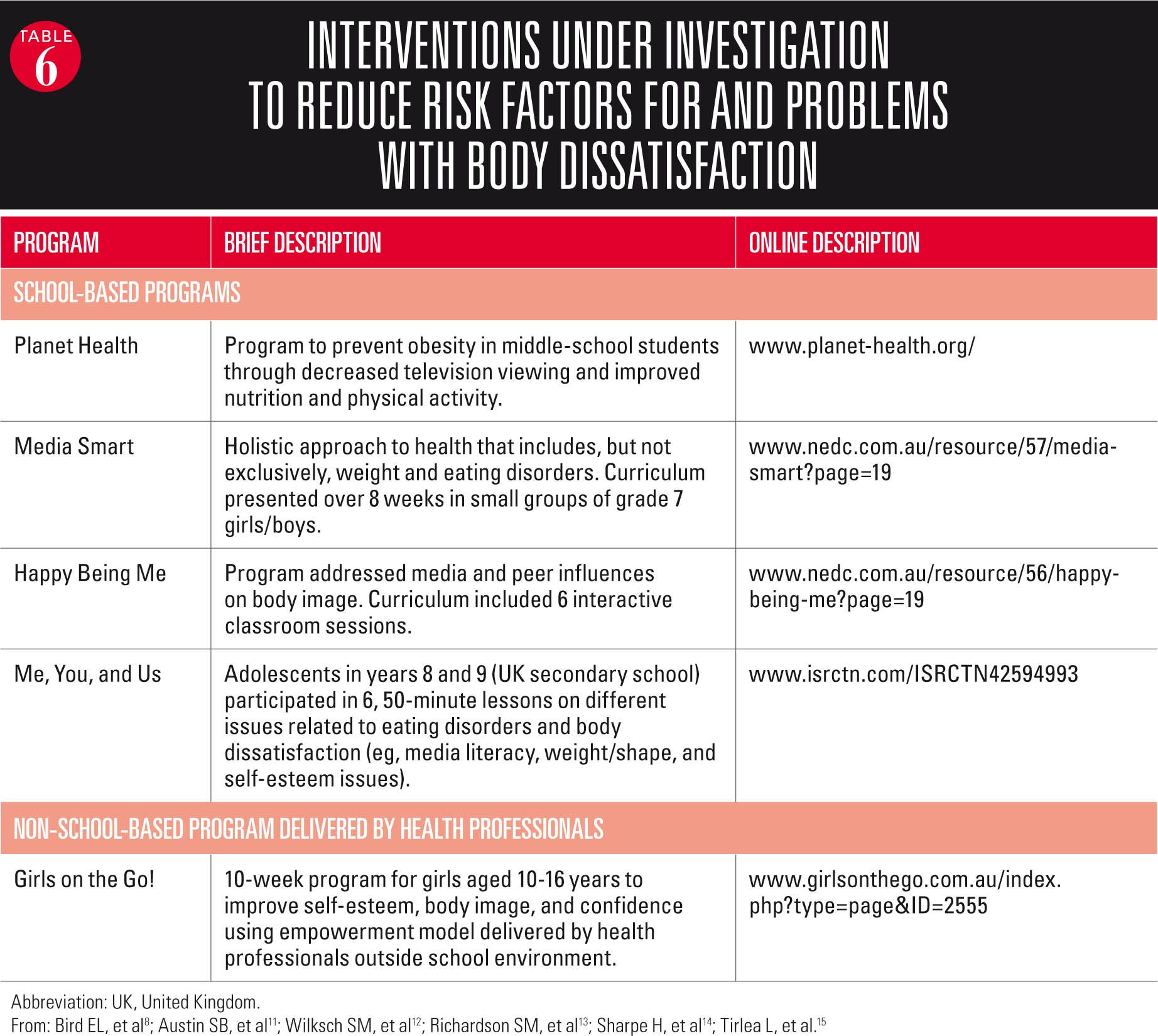
These preventive efforts can be used to intervene when poor body image has developed. Along with these efforts, a number of school-based programs are under investigation to examine their impact on prevention and intervention (Table 6).8,11-14 Also promising is a program designed for delivery by healthcare professionals outside the school setting. Called “Girls on the Go!,” the program is described as a group-based, low-dose intervention targeted at girls aged between 10 and 16 years (Table 6).15 Results of randomized trials that tested this program found it significantly increased self-esteem and self-efficacy for primary and secondary school-aged children and reduced dieting behaviors for secondary school students.15
NEXT: How can parents help their children improve their self image?
Summary
Poor body image in children and adolescents is associated with disordered eating and other maladaptive behaviors that place them at increased risk for a number of physical and psychologic problems. Children and teenagers who are overweight and obese are at risk of developing poor body image, and those who perceive themselves as overweight are even at higher risk.
More: What's new about lead poisoning?
Pediatricians and other healthcare professionals can help prevent poor body image by identifying children and adolescents at risk for poor body image, and providing guidance on, among other issues, realistic perceptions of body weight and healthy eating.
NEXT: What are the interventions currently being investigated?
REFERENCES
1. Evans EH, Tovée MJ, Boothroyd LG, Drewett RF. Body dissatisfaction and disordered eating attitudes in 7- to 11-year-old girls: testing a sociocultural model. Body Image. 2013;10(1):8-15.
2. Calzo JP, Masyn KE, Corliss HL, Scherer EA, Field AE, Austin SB. Patterns of body image concerns and disordered weight- and shape-related behaviors in heterosexual and sexual minority adolescent males. Dev Psychol. June 22, 2015. Epub ahead of print.
3. Field AE, Sonneville KR, Crosby RD, et al. Prospective associations of concerns about physique and the development of obesity, binge drinking, and drug use among adolescent boys and young adult men. JAMA Pediatr. 2014;168(1):34-39.
4. Rodgers RF, Paxton SJ, McLean SA. A biopsychosocial model of body image concerns and disordered eating in early adolescent girls. J Youth Adolesc. 2014;43(5):814-823.
5. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814.
6. Farhat T. Stigma, obesity, and adolescent risk behaviors: current research and future directions. Curr Opin Psychol. 2015;5:56-66.
7. Farhat T, Iannotti RJ, Summersett-Ringgold F. Weight, weight perceptions, and health-related quality of life among a national sample of US girls. J Dev Behav Pediatr. 2015;36(5):313-323.
8. Bird EL, Halliwell E, Diedrichs PC, Harcourt D. Happy Being Me in the UK: a controlled evaluation of a school-based body image intervention with pre-adolescent children. Body Image. 2013;10(3):326-334.
9. Croll J. Body image and adolescents. In: Stang J, Story M, eds. Guidelines for Adolescent Nutrition Services. Minneapolis, MN: University of Minnesota, 2005.
10. Duncan DT, Hansen AR, Wang W, Yan F, Zhang J. Change in misperception of child’s body weight among parents of American preschool children. Child Obes. 2015;11(4):384-393.
11. Austin SB, Spadano-Gasbarro JL, Greaney ML, et al. Effect of the planet health intervention on eating disorder symptoms in Massachusetts middle schools, 2005-2008. Prev Chronic Dis. 2012;9:E171.
12. Wilksch SM, Paxton SJ, Byrne SM, et al. Prevention across the spectrum: a randomized controlled trial of three programs to reduce risk factors for both eating disorders and obesity. Psychol Med. 2015;45(9):1811-1823.
13. Richardson SM, Paxton SJ. An evaluation of a body image intervention based on risk factors for body dissatisfaction: a controlled study with adolescent girls. Int J Eat Disord. 2010;43(2):112-122.
14. Sharpe H, Schober I, Treasure J, Schmidt U. Feasibility, acceptability and efficacy of a school-based prevention programme for eating disorders: cluster randomised controlled trial. Br J Psychiatry. 2013;203(6):428-435.
15. Tirlea L, Truby H, Haines TP. Pragmatic, randomized controlled trials of the Girls on the Go! program to improve self-esteem in girls. Am J Health Promot. May 14, 2015. Epub ahead of print.
Ms Nierengarten, a medical writer in St. Paul, Minnesota, has over 25 years of medical writing experience, authoring articles for Lancet Oncology, Lancet Neurology, Lancet Infectious Diseases, and Medscape. She has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.