Genetic Disorders: Recognition and (Yes!) Therapy
Genetic diseases are individually rare but common in the aggregate. They account for over 60% of early miscarriages and underlie most cases of developmental delays. Genetic changes predispose to common multifactorial disorders, such as diabetes mellitus or schizophrenia, and are present in every cancer.
I am happy to introduce this special supplement to Consultant for Pediatricians that highlights a new era of therapy for genetic disease. The cases here set the stage for a brief discussion of triage and testing, and for an update on management of genetic disorders-from prevention of complications to real therapy through tissue/enzyme replacement.
Your role as pediatrician is pivotal for early recognition and referral of patients with genetic disease and it is key to optimizing child development and later reproduction.1-3
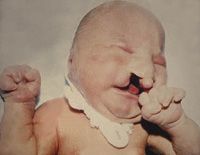

Case A is a term newborn with hypertonia and several anomalies, including cleft lip/palate, bilateral postaxial polydactyly, and penile chordee. His family and gestational histories are unremarkable.
Case B is a 6-year-old boy with absent speech, connective tissue laxity, and autistic behavior. His mother has learning disabilities and a maternal uncle is said to have mental retardation.

Case C shows the pedigree of a newborn who appeared normal at birth. She deteriorated on day 2 of life (laboratory test values are shown). A sibling also died in the newborn period.
Do you recognize these disorders? (Diagnoses appear on the next page.)
Answers:
Recognition, Not Recall: Triage of Genetic Disorders
Genetic diseases are individually rare but common in the aggregate. They account for over 60% of early miscarriages and underlie most cases of developmental delays. Genetic changes predispose to common multifactorial disorders, such as diabetes mellitus or schizophrenia, and are present in every cancer.
Genetic diseases can be categorized as chromosomal, Mendelian (involving single genes), or multifactorial (multiple genes plus environmental factors). Relatively common multifactorial disorders such as diabetes mellitus, schizophrenia, or isolated birth defects rarely cluster in families and have low recurrence risks (2% to 5% for primary relatives). Chromosomal disorders are usually sporadic, except for rare families with translocations. Mendelian diseases have significant recurrence risks (up to 50% for autosomal dominant conditions, 25% for autosomal or X-linked recessive conditions). Screening forms are adequate to define most family histories, occasionally prompting informative pedigree sketches like that for case C (autosomal recessive).4
Pediatricians most often encounter children with multifactorial or common Mendelian disorders and manage them in league with the appropriate subspecialist. The more common genetic disorders are well covered in pediatric training programs, ensuring familiarity with conditions like diabetes, cystic fibrosis, and sickle cell anemia. It is the child with several birth defects or possible metabolic disease who prompts referral to a geneticist.
The Figure illustrates a simple approach to clinical triage that begins with the question: does the child have physical anomalies? Newborns with obvious anomalies occupy one extreme of the dysmorphology spectrum (see case A). Those with a normal appearance and chemical changes fall on the opposite side (see case C). If there is a physical anomaly, is the birth defect isolated or part of a pattern? I use a checklist to facilitate systematic identification of minor anomalies that can indicate a pattern of abnormal development.5 Sometimes children with delays and subtle anomalies have a form of "pure" mental disability (eg, fragile X syndrome in case B). The physical examination reveals the possibility of a syndrome, which is confirmed by referral with references for details.4-9

Children who appear normal may deteriorate after birth with acute, intermittent, or insidious symptoms. Keep acute metabolic disease in mind when a newborn deteriorates after feeding.7,8 Acute disorders typically involve small molecules, such as ammonia or propionic acid, and cause changes in routine chemistries illustrated by the acidosis with anion gap (as in case C). Milder metabolic derangements may manifest with intermittent illness. Stay attuned to unusual severity of routine illness. Opportune follow-up of routine chemistries with blood acylcarnitine profile/amino acids and urine organic acids may reveal an intermittent disorder of metabolism, such as the potentially lethal disorders of fatty acid oxidation.7,8
The third metabolic category involves children who appear normal at birth but whose development plateaus or deteriorates thereafter. Some have childhood disintegrative disorder of the autism spectrum; others regress because of insidious metabolic or storage disease. Storage diseases involve accumulation of large molecules that often affect the brain. The accompanying case provides a striking example of insidious metabolic disease caused by accumulation of mucopolysaccharides. Testing for storage diseases may first identify large molecules in tissues or fluids; enzyme or DNA tests then define the recessive-acting genetic mutation.4
Again, it is early recognition and referral by pediatricians that brings in the geneticist to guide testing and dietary/enzyme therapy for patients with metabolic disease.7-9 Although specifics of genetic testing can be left to the subspecialist, clinical distinction of the dysmorphology/metabolic categories can guide your initial approach and allow preliminary testing that supports your choice of referrals.
Online Help Is at Hand
Therapy for Genetic Disease-Preventive Health Care
Despite the complexity of genetic testing, pediatricians are uniquely equipped to provide a medical home for patients with chronic genetic diseases. The patient with an acute metabolic disorder that is responsive to nutritional therapy will need experienced assessment of neurosensory function, growth, and development in conjunction with subspecialty management. For patients with intermittent metabolic disorders, knowledge of feeding strategies to maintain carbohydrate calories (without the need to switch to fatty acid oxidation) can be lifesaving. Isolated birth defects can be associated with risks for feeding (eg, cleft palate) or hearing difficulties, or for spinal damage from intubation (eg, Klippel-Feil anomaly).9 Children with syndromes have multiple risks that require anticipatory guidance and case management.
Checklist reminders are available to guide busy practitioners in coordinating special needs care.9 Often resolution of simple issues (sleep, feeding, behavior) is pivotal.
Therapy for Genetic Disease-Medical Treatment
Although gene replacement is the logical choice for genetic disease, difficulties with accurate tissue/chromosome targeting and harm from viral gene carriers have limited its application. Enzyme replacement, which uses tissue transplant or infusion of purified molecules, has proved more effective. Persisting challenges include finding compatible donors or getting curative cells/enzymes across the blood-brain barrier to treat the CNS. High mortalities (10% to 15%) with bone marrow transplant are declining as methods for enriching the colonizing stem cells lower rates of graft-versus-host reactions. Umbilical blood banking provides stem cells to replenish bone marrow after cancer chemotherapy, but the individual’s unadulterated cells will not correct any inherited condition. However, introduction of genes into cell cultures is feasible and may predict future therapies with manipulated stem cells.

Standard therapies for acute metabolic disease are now paralleled by enzyme replacement therapies for insidious disorders. Dietary therapies include the restriction of essential substrates (like phenylalanine in phenylketonuria), elimination of inessential substrates (like lactose in galactosemia), salvage of ammonia through diverting agents (like phenylbutrate for urea cycle disorders), and avoidance of damaging pathways (like frequent feeding for disorders of fat oxidation). Now enzyme replacement can ameliorate or cure insidious metabolic disorders (Table). Through early recognition and referral, the pediatrician can be a "lifesaver" for several genetic disorders and a “brain-saver” for many others.
Basic research and industry have collaborated to provide a growing number of treatments for genetic disease, foreshadowing an era of true molecular medicine.10 Never forget your role as a pediatrician in recognizing affected children and grounding new therapy in the venerable foundation of a medical home.
References:
REFERENCES:
1. Cooley WC. Redefining primary pediatric care for children with special health care needs: the primary care medical home. Curr Opin Pediatr. 2004;16:689-692.
2. McMillan JA. Distribution of specialized care to children: role of the pediatric generalist and subspecialist. J Pediatr. 2002;140:491-492.
3. Jaffee A. Women’s health begins in pediatrics. Arch Pediatr Adolesc Med. 1994;148:783.
4. Online Mendelian Inheritance in Man. www.ncbi.nlm.nih.gov/entrez/. Accessed August 1, 2008.
5. Wilson GN. Neonate with hypotonia and subtle anomalies (Down syndrome). Consultant For Pediatricians. 2007;7:69-77.
6. Jones KL. Smith’s Recognizable Patterns of Human Malformation. 6th ed. Philadelphia: WB Saunders; 2006.
7. Weiner DL. Inborn errors of metabolism. www.emedicine.com/emerg/topic768.htm. Accessed July 28, 2008.
8. Saudubray JM, Carpentier C. Clinical phenotypes; diagnoses, algorithms [for inborn errors]. In: Scriver CR, Beaudet AL, Sly WS, Valle D, eds. The Metabolic and Molecular Bases of Inherited Disease. 8th ed. New York: McGraw-Hill; 2001:1327-1406. (This reference also contains excellent review chapters on genetics, molecular testing, gene and enzyme therapy.)
9. Wilson GN, Cooley WC. Preventive Health Care for Children With Genetic Conditions: Providing a Primary Care Medical Home. 2nd ed. Cambridge, UK: Cambridge University Press; 2006.
10. Pyeritz RE. A small molecule for a large disease. N Engl J Med. 2008;358:2829-2831.