A guide to early detection of scoliosis
Pediatricians& ability to recognize scoliosis and associated findings early can make a tremendous difference in outcome. The authors take you step by step through a spinal examination and review conditions in the differential diagnosis.
A guide to early detection of scoliosis
By Kingsley R. Chin, MD, J. Scott Price, MD, and Seymour Zimbler, MD
Pediatricians' ability to recognize scoliosis and associated findings early can make a tremendous difference in outcome. The authors take you step by step through a spinal examination and review conditions in the differential diagnosis.
Pediatric spinal deformities can be a source of tremendous anxiety for families and their doctors. These deformities are varied and may present at any time from birth through adolescence. Some deformities are benign and self-limiting; others may progress and cause substantial morbidity and death from cor pulmonale; and still others may be associated with multiple anomalies in different organ systems.
Orthopedic surgeons are usually responsible for anticipating deformities that could deteriorate rapidly and for formulating a treatment plan of bracing or surgery. But because most patients with an early deformity are seen by pediatricians and family physicians, your ability to recognize spinal deformity and associated findings and to refer the patient early may be the difference between a good treatment outcome and a bad one.
With that in mind, this article focuses on tips you can use to perform an effective spinal examination. We also highlight important conditions associated with one of the most common spinal deformitiesscoliosis.
Performing a general evaluation
Pediatric spinal deformities are grouped as either scoliosis, kyphosis, or lordosis based on the plane of deformity. Recognizing these deformities is the first step in evaluating a patient. Scoliosis is a coronal plane deformity resulting in lateral curvature of the spine. Kyphosis is an excessive convex curvature of the spine with a posteriorly directed apex, a "humpback" commonly seen in the thoracic spine. Lordosis is an excessive concave curvature of the spine with an anteriorly directed apex, commonly seen in the lumbar and cervical spine regions. Any hint of scoliosis, variation in the normal kyphosis of the thoracic spine, or lordosis of the lumbar or cervical spine should prompt inquiry.
Begin with a complete history. The child or adolescent, parents, and any other active caregiver should be present. Allowing input from each member offers insight into how the problem affects the patient and family. Start with general questions to elicit an overall systems review; leave specific questions about the spinal deformity for the end of the history taking. This approach will decrease the risk of missing an associated disorder.
Ask about weight loss, fever, lethargy, skin abnormalities, and joint pain and swelling. Focus on the presence of back pain, remembering that such pain is usually abnormal in children. Note time of onset of pain, location, frequency, duration, severity, and character. Night pain is worrisome because it is associated with tumors, infections, and inflammatory conditions. Any radicular pain, abnormal sensation, weakness, changes in bowel or bladder habits, or balance or coordination difficulties are a tip-off to a potential underlying neurologic problem.
Assess developmental milestones, especially delays during the first two years of life. Difficulties with learning, hearing, gait, vision, and the genitourinary tract may be seen in patients with spinal deformities as a feature of other syndromes. If the patient is an adolescent girl, question her about onset of menses; approximately two years of growth remain after menarche. Scoliosis in girls progresses and requires treatment more often than in boys. With boys, ask about voice changes, the appearance of axillary and pubic hair, and the initiation of shavingevents that generally coincide with the onset of spinal maturity.
Keep in mind that the range of maturity for adolescents varies, and some adolescents continue to grow into their late teens. Nonetheless, the six months before and after the onset of puberty represent the periods of most rapid growth, when patients are at greatest risk for curve progression. Such progression occurs at an approximate maximal rate of one degree a month in idiopathic scoliosis. Plot the child's height on pediatric growth charts to identify stature below the third percentile, which may indicate a bone dysplasia, a syndrome, or an endocrine abnormality.
Inquire when and how the deformity was first detected. Some patients detect asymmetry in their torso, clothing, or stance, but neglect to mention it to a physician until a friend or other family member brings it to their attention. Determine whether there has been a substantial change in the deformity. A detailed family history of genetic conditions is of paramount importance in identifying scoliosis-associated syndromes.
Physical examination
If performed systematically, the physical assessment takes up little time but can uncover even small curves. Begin as soon as you enter the exam room by observing the patient's posture and her (or his) interactions with the parent or caregiver. Physical features and body proportions may be clues to conditions associated with scoliosis.
Start the exam itself with a general inspection of the patient in the standing position. Her head should be directly aligned over the midline of the sacrum. Any deviation from this midline represents spinal deformity. Look for obvious asymmetries along the contours of the back, especially an elevated scapula, an uneven waistline, and the presence of rib humps (Figure 1).

Evaluate tall, thin patients for a high-arched palate, lens dislocation, and abnormally long metacarpalssuggestive of Marfan syndrome. These patients will have an idiopathic scoliosis pattern of long sweeping right thoracic and left lumbar curves. Joint laxity, dislocating patellae and shoulders, and sternal deformities can be seen in the various types of Ehlers-Danlos syndrome (Figure 2).

Assess patients with short stature for other physical findings such as corneal clouding (seen in mucopolysaccharidoses) and limb deformity (Figure 3). Alignment of the lower extremities (genu valgum or genu varum) and the relationship between trunk length and leg length are extremely important in identifying the many variations of bone dysplasia. Many patients with this condition also present with spinal asymmetry and deformity.

Next, evaluate the skin for cutaneous changes, hair patches, dermal sinuses, or clefts (spinal dysraphism or myelomeningocele). More than five café au lait spots or the presence of axillary freckles suggests neurofibromatosis.
Perform the Adams forward-bending test with the patient either sitting (which eliminates leg-length discrepancy) or standing. The test is usually performed with the patient's feet together and knees straight. Instruct the patient to straighten the elbows and place the palms together while bending forward at the waist. A small child can be examined by flexing the trunk over the legs of an examiner or parent sitting in a chair or on the examination table, while the child's feet remain on the floor or table. Patients with tight hamstring muscles may flex their knees, which increases flexion at the waist and the ability to bend forward.
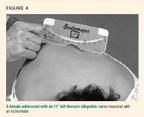
View the patient's back from the head, sides, and rear of the patient. A visible hump (Figure 1) is produced by convexity of the ribs and suggests spinal deformity with vertebral rotation. You can use an inclinometer (Scoliometer, Orthopaedic Systems, Inc.) to measure the rotational deformity (rib hump) of the spine and to approximate the lateral curvature (scoliosis) (Figure 4). Place the inclinometer on the peak of the hump and note the angle of trunk rotation. A rotation of 5° to 7° on an inclinometer corresponds to a 10° to 20° lateral spine curvature and should be evaluated radiographically. A rotation of less than 5° on inclinometer in a skeletally immature child is at risk of progression and should be followed. The smaller the curve, the longer the follow-up interval. Patients who may need bracing if further progression occurs should be followed within four months.
On rare occasions, large scoliotic curves can develop without notable rotational changes in the vertebrae or obvious signs of asymmetry. This may be the case, for example, with obese patients and those with a double curve. While the patient is still standing, palpate the entire spine for irregularities or pain.
To check for leg-length discrepancy, have the patient stand with both feet together and place your index fingers against her waist at the level of both iliac crests. If your fingers are not at the same level, one leg is probably longer than the other. To eliminate the contribution of leg-length discrepancy to pelvic obliquity and scoliosis, place thin wooden blocks (of known height) under the shorter extremity. Also observe the patient from the side to note any abnormality in the normal thoracic kyphosis and lumbar lordosis. (Thoracic kyphosis of 45° and lumbar lordosis of 45° are normal measurements. Measurements beyond this are considered pathologic or excessive kyphosis and lordosis.)
Test for gross motor strength, coordination, and balance by asking the patient to walk on her toes and then on her heels toward you. Then ask her to hop on both feet, to hop on one foot, and to squat. Perform a Romberg test (the patient closes both eyes and straightens both arms at shoulder height) to differentiate between peripheral and cerebellar ataxia. An abnormal Romberg test with ataxia during gait may suggest a diagnosis of Friedreich ataxia.
Next, examine the patient supine on the table. Inspect the chest, rib cage, axillary areas, and pubic areas to supply information for Tanner staging and to assess for chest-wall deformities, such as pectus excavatum or carinatum (pigeon chest).
Perform complete reflex, motor, and sensory tests. Test for abdominal reflexes by lightly stroking the skin on each side of the umbilicus with your index finger; the abdominal muscles should contract and the umbilicus move toward your finger. A unilateral absent reflex suggests hydrosyringomyeliacerebrospinal fluid within the substance of the spinal cord.
Examine the lower extremities for contractures and abnormalities of the feet. Assess for muscular atrophy by measuring and comparing thigh and calf circumferences. Atrophy of the calves or quadriceps is associated with polio, cerebral palsy, and other neurologic abnormalities. Cavus feet (high-arching feet) may also indicate a neuromuscular disorder. In contrast, hyperlaxity and flat feet may suggest collagen vascular disease such as Ehlers-Danlos and Down syndromes.
Assess hamstring flexibility by measuring the child's popliteal angle, which is the angle formed between the back of the thigh and the lower leg when extending the knee and flexing the hip in the supine position. In other words, full-knee extension is normal, and the number of degrees away from full extension is the popliteal angle. Tight hamstrings indicate spondylolisthesis or other low lumbar spine abnormalities. More generalized joint contractures may be consistent with arthrogryposis (Figure 5), myopathies, or other neurologic conditions.

The remainder of the physical examination can focus on specific findings that may suggest one of the many syndromes that has scoliosis as a feature (Table 1).
TABLE 1
The wide differential diagnosis of scoliosis
Radiographic assessment
While the physical examination tips just described improve the sensitivity of detecting body asymmetries, they are not specific for scoliosis or precise for determining curve magnitude. These can be confirmed only by taking entire spine radiographs, both posteroanterior and lateral standing. The Cobb angle technique quantifies the amount of scoliosis, kyphosis, or lordosis1 (Figure 6). When describing scoliosis, note whether the curve is present in the cervical, thoracic, or lumbar spine and whether the apex of the curve is to the left or right. The most common finding in idiopathic scoliosis is a single right thoracic curve. A left thoracic curve is more ominous and suggests an underlying pathologic condition.

Also look at the iliac crests to make rough radiographic inferences about skeletal maturity (Figure 6 [right]). The iliac apophysis gradually fuses from anterolateral to posteromedial and is staged by the Risser system (Table 2). Progression takes about one year, and fusion an additional two years.2 Spinal growth is unlikely but can occur after fusion.3 Idiopathic curves are, therefore, less likely to increase in magnitude as the apophysis progresses. Bracing of idiopathic curves is recommended for curves between 20° and 40° in patients who are Risser 0, 1, or 2. Patients who are Risser 3 and above may not have enough growth remaining to benefit from bracing, but this is an individualized decision made by the orthopedic surgeon.
TABLE 2
Risser staging system to gauge iliac apophysis
Magnetic resonance imaging (MRI) is recommended in patients with atypical curves (left thoracic, right lumbar, or other unusual patterns), and in those who have back or leg pain or neurologic deficits. It is also recommended in male patients and in patients who have unusually rapidly progressing curves, lower extremity deformity, or juvenile idiopathic scoliosis large enough to require treatment.2,4 Males with large structural curves or rapid progression of deformity have a greater chance of occult intraspinal abnormalities.
Differential diagnosis of nonstructural curves
Although scoliosis is usually a benign cosmetic problem, it can signify a serious condition. Scoliosis may, for example, be associated with abnormalities in the brain, spinal cord, vertebral column, gastrointestinal tract, cardiovascular system, and renal system.58 Approach each patient with this thought in mind. We find it useful to try to separate nonstructural from structural curves. A nonstructural curve is often benign and usually corrects with postural changes or treatment of the underlying condition. In contrast, a structural curve requires direct treatment with bracing or surgery and is more likely to be associated with other anomalies.
First separate out nonstructural curves that are associated mostly with poor posture, muscular weakness (abdominal), psychological problems (hysteria), leg-length discrepancy, paravertebral muscular spasm, or visceral pain.5 Postural scoliosis is not usually associated with a prominence on forward bending, and the curve improves when the child lies prone or stands upright. Plain radiographs usually show a long gentle curve extending from the base of the neck to the end of the spine with no rotation.
Patients with leg-length discrepancy often present with an apparent scoliosis or pelvic obliquity that corrects by placing wooden blocks of the proper height under the short limb. These curves also correct when the patient is sitting or lying flat.
Other nonstructural curves may present with back pain. In the case of a painful herniated lumbar disk, patients may lean away from the herniated side to relieve pressure on the nerve root. Keep in mind, however, that back pain in children is often abnormal and requires its own evaluation. An MRI will confirm disk protrusion or identify other painful conditions such as fracture, infection, tumor, or nerve-root tethering. Osteoid osteoma is the most common cause of painful adolescent scoliosis.2 Other benign tumors, such as osteoblastoma, eosinophilic granuloma, and aneurysmal bone cysts, also elicit significant night pain. The postural scoliosis secondary to their presence usually dissipates after tumor excision, if performed within about one year of onset.
Differential diagnosis of structural curves
Structural curves may have a congenital or neuromuscular etiology, or may be idiopathic. Other causes are tumor, osteochondrodystrophies, iatrogenesis, and metabolic and mesenchymal diseases. Several genetic syndromes also display scoliosis among their many features (Table 1).
Idiopathic scoliosis is the most common etiology of scoliosis. It is a diagnosis of exclusion. The condition is categorized as either early onset or late onset. The former occurs from birth to 5 years of age and often presents as a left thoracic curve. Boys are affected more often than girls, but girls may have a worse prognosis.9 Although this is mostly a self-limiting condition, with spontaneous remission occurring in as many as 92% of cases,10 the curves may progress rapidly during adolescence and the child should be referred to an orthopedist early. In addition, patients may present with plagiocephaly, hip dysplasia, "bat" ears, sternomastoid tightness, congenital malformations, and mental retardation.11,12 An MRI is generally obtained to rule out central nervous system pathology such as syringomyelia, Arnold-Chiari malformation (displacement of the brain stem into the foramen magnum), or a tethered cord (present in 17% of patients with early-onset scoliosis).6
Late-onset idiopathic scoliosis appears after age 5 and constitutes the majority of idiopathic scoliosis. Curves less than 10° by radiograph and less than 5° by inclinometer are considered normal variants, but should still be followed through skeletal maturity. Left thoracic curves should be evaluated with MRI, for reasons explained below.
Congenital scoliosis may result from a range of anomalies in the developing vertebrae and most commonly presents as a left thoracic curve. The radiograph below shows a small left thoracolumbar curve due to a hemivertebra in a child with congenital scoliosis. A hemivertebra results from failure to form a complete vertebra, as opposed to a bar, which is failure of segmentation to form disk spaces between vertebrae. Two bars across the same vertebral segment form a block vertebrae with no potential for deformity. The greatest potential for deformity occurs when there is a hemivertebra on one side of the spine across from a bar.

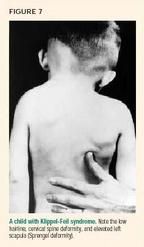
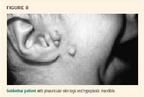
These vertebral defectshemivertebra, bar, and blockusually occur during the first six weeks of gestation; they therefore coincide with organogenesis, which explains their common association with other conditions. Any left thoracic curve should therefore prompt a more thorough evaluation, including MRI and renal ultrasonography, to look for congenital vertebral anomalies or defects in other organ systems. Patients with congenital curves include those who have Klippel-Feil syndrome5,12 (Figure 7), Goldenhar syndrome5 (Figure 8), or Jarcho-Levin syndrome5 (Figure 9).

Neuromuscular scoliosis may be the result of myopathies and upper or lower motor neuron disorders. The key point to remember is that nonambulatory patients are more likely to develop progressive scoliosis than ambulatory patients.
The most common group of scoliotic patients with upper motor neuron lesions are those who have cerebral palsy. Almost 100% of nonambulators with cerebral palsy have scoliosis, whereas only 5% to 10% of ambulators with mild spasticity develop scoliosis.5,6,13 Early referral is encouraged because these patients may require surgery to lessen the risk of pulmonary complications and to allow them to sit upright in a wheelchair.
Lower motor neuron lesions secondary to trauma, spinal muscular atrophy, and viral myelitides such as poliomyelitis, and myopathies such as arthrogryposis14 and Duchenne and Becker muscular dystrophy,2 can all present with severe structural scoliosis.14
Scoliosis is the most common musculoskeletal presentation of neurofibromatosis. Radiographs may show sharp thoracic curves with pathognomonic erosions and flattening of the ribs, vertebral scalloping, foraminal enlargement, and spindling of the transverse processes thought to be due to the presence of local, dumbbell-shaped neurofibromas. Look for café au lait spots, and assess the lower leg for anterolateral tibial bowing and pseudarthrosis (nonhealing fractures).
Neurologic symptoms should prompt an inquiry for neural defects in addition to upper motor lesions. Intraspinal anomalies are found in up to 38% of patients with congenital spine deformities.15 These include syringomyelia, tethered cord, low conus (end of spinal cord below L2), lipoma, diplomyelia, diastematomyelia (a condition in which bone, cartilage, or fibrous bands invaginate or divide the spinal cord longitudinally), and Arnold-Chiari malformation. Any of these conditions can cause significant progressive scoliosis, and both the underlying pathology and the curve require treatment.16
Osteochondrodystrophies are relatively rare conditions often characterized by short stature. Spinal deformity may manifest in this group, which includes achondroplasia, diastrophic dysplasia, pseudoachondroplasia, spondyloepiphyseal dysplasia, Larsen syndrome, and some mucopolysaccharidoses. Diastrophic dwarfs (Figure 3) may develop severe scoliosis as well as thoracic and cervical kyphosis and are at risk for quadriplegia.17 Larsen syndrome is characterized by multiple congenital dislocations of large joints, a flat face, and ligamentous laxity with frequent congenital defects of the cervical, thoracic, and lumbar spine.5
Metabolic diseases such as osteogenesis imperfecta (OI), rickets, and homocystinuria may result in scoliosis and kyphosis. Spinal deformities are found in as many as 80% of patients with OI; progression may occur after skeletal maturity and is thought to be the result of weakened osteoporotic bones. Homocystinuria may appear phenotypically similar to Marfan syndromepatients are tall and slender and have scoliosis. They often require a urine metabolic screen and hypercoagulability test for differentiation.
Iatrogenic deformities may result from irradiation or surgery such as thoracotomy, rib resection, multilevel laminectomy, spinal fusion, and cord ischemia. Irradiation of Wilms' tumor or neuroblastoma commonly affects the growth of the vertebral epiphyseal plate, resulting in scoliosis or kyphosis; it should be anticipated, especially in children younger than 2 years of age. Irradiation of the iliac crest or femoral heads may lead to leg-length discrepancy and a secondary nonstructural scoliosis.2
Other syndromes of orthopedic significance, such as Turner syndrome (45XO), often present with an idiopathic scoliosis-like curve pattern, and the use of growth hormone to improve stature speeds their progression. Noonan syndrome resembles Turner, but the chromosomes and gonads are normal and there is a higher incidence of scoliosis (40%).5 Down syndrome has a 50% incidence of idiopathic-like scoliosis. Juvenile-onset scoliosis is the most significant orthopedic problem affecting Prader-Willi patients (Figure 10). A triad of organomegaly, omphalocele, and a large tongue characterizes Beckwith- Wiedermann syndrome. These patients frequently have idiopathic scoliosis.

Other causes of scoliosis worth mentioning include thoracic scarring secondary to empyema or burns. Most pediatricians will at some point diagnose spondylolisthesis, which is a slippage of one vertebra onto another. Lumbar scoliosis may occur as a result of torsion of the spine through the spondylolysthetic area (structural curve) or muscle spasm (nonstructural curve), which usually resolves with recumbency or pain relief. Patients may present with back discomfort that coincides with the adolescent growth spurt. Pain is often related to activities and may suggest a fracture of the pars interarticularis (spondylolysis), frequently seen in football linemen and ballet dancers. A structural step-off may be palpated in the lower spine.
Postural deformity and restricted motion of the lumbar spine with bending exercises and limitation of straight-leg raises secondary to hamstring tightness should tip off the examiner to the diagnosis of spondylolisthesis, among other conditions. Anteroposterior, lateral, and oblique plain radiographs of the lumbosacral spine will reveal some, but not all, cases. A good lateral standing view of L5S1 is worth the radiation, in our view.
Early referral is key
Scoliosis is often a sign of an underlying problem. That alone should prompt a thorough evaluation of the entire patient and family history, not just of the spine. The pediatrician and family physician are uniquely positioned to anticipate, evaluate, and monitor patients with scoliosis, referring cases early on. Doing so will improve the likelihood of a better outcome after bracing or surgery.
1. Morrissy RT, Goldsmith GS, Hall EC, et al: Measurement of the Cobb angle on radiographs of patients who have scoliosis: Evaluation of intrinsic error. J Bone Joint Surg 1990;72A:320
2. Garfin SR, Vaccaro AR: Orthopaedic Knowledge Update: Spine. Rosemont, Ill., American Academy of Orthopaedic Surgeons, 1997
3. Little DG, Sussman MD: The Risser sign: A critical analysis. J Pediatr Orthop 1994;14:569
4. Lewonoski K, King JD, Nelson MD: Routine use of magnetic resonance imaging in idiopathic scoliosis patients less than 11 years of age. Spine 1992;17(supp 16):S109
5. Morrissy RT, Weinstein SL: Lovell and Winter's Pediatric Orthopaedics, ed 4. Philadelphia, Pa., Lippincott- Raven, 1996
6. Winter RB, Lonstein JE, Denis F, et al: Prevalence of spinal canal or cord abnormalities in idiopathic, congenital, and neuromuscular scoliosis. JAMA 1993; 269(20);16:135
7. McMaster MJ, Ohtsuka K: The natural history of congenital scoliosis. J Bone Joint Surg (Am) 1982; 64A(8):1128
8. Dravic DM, Ruderman RJ, Conrad RW, et al: Congenital scoliosis and urinary tract abnormalities: Are intravenous pyelograms necessary? J Ped Orthop 1987;7:441
9. Thompson SK, Bentley G: Prognosis in infantile idiopathic scoliosis. J Bone Joint Surg 1980;62B:151
10. Lloyd-Roberts GC, Pilcher MF: Structural idiopathic scoliosis in infancy. J Bone Joint Surg 1965;47B:520
11. Wynne-Davies R: Infantile idiopathic scoliosis. J Bone Joint Surg 57B:138
12. Weinstein SL (ed): The Pediatric Spine: Principles and Practice. Raven Press, N.Y., 1994
13. Ferguson RL, Allen BL: Considerations in the treatment of cerebral palsy patients with spinal deformities. Orthop Clin North Am 1988;19(2):419
14. Shapiro F, Specht L: The diagnosis and orthopaedic treatment of childhood spinal muscular atrophy, peripheral neuropathy, Friedreich ataxia, and arthrogryposis. J Bone Joint Surg 1993;75A:1699
15. Bradford DS, Heithoff KB, Cohen M: Intraspinal abnormalities and congenital spine deformities: A radiographic and MRI study. J Pediatr Orthop 1991;11:36
16. Richards SB: Orthopaedic Knowledge Update: Pediatrics. Rosemont, Ill., American Academy of Orthopaedic Surgeons, 1996
17. Poussa M, Merikanto J, Ryoppy S, et al: The spine in diastrophic dysplasia. Spine 1991;16:881
DR. CHIN was a resident in the Harvard Combined Orthopaedic Residency Program, Harvard Medical School, Boston, at the time this article was written. He will be starting a fellowship in spine surgery with Henry Bohlman, MD, at Case Western University Medical School, Cleveland.
DR. PRICE is a resident in the Harvard Combined Orthopaedic Residency Program, Harvard Medical School.
DR. ZIMBLER is an instructor in orthopedic surgery, Boston Children's Hospital and Harvard Medical School, and clinical professor in orthopedic surgery, Tufts Medical School, Boston.
Kinsley Chin, Scott Price, Seymour Zimbler. A guide to early detection of scoliosis.
Contemporary Pediatrics
2001;9:77.