HEEADSSS 3.0: The psychosocial interview for adolescents updated for a new century fueled by media
The latest update to the HEEADSSS psychosocial interview for adolescents includes new questions on electronic media use in addition to its time-tested strategies for identifying the critical stressors that affect the overall well-being of teenaged patients.
This article is part of a resource center for the HEEADSSS psychosocial interview.
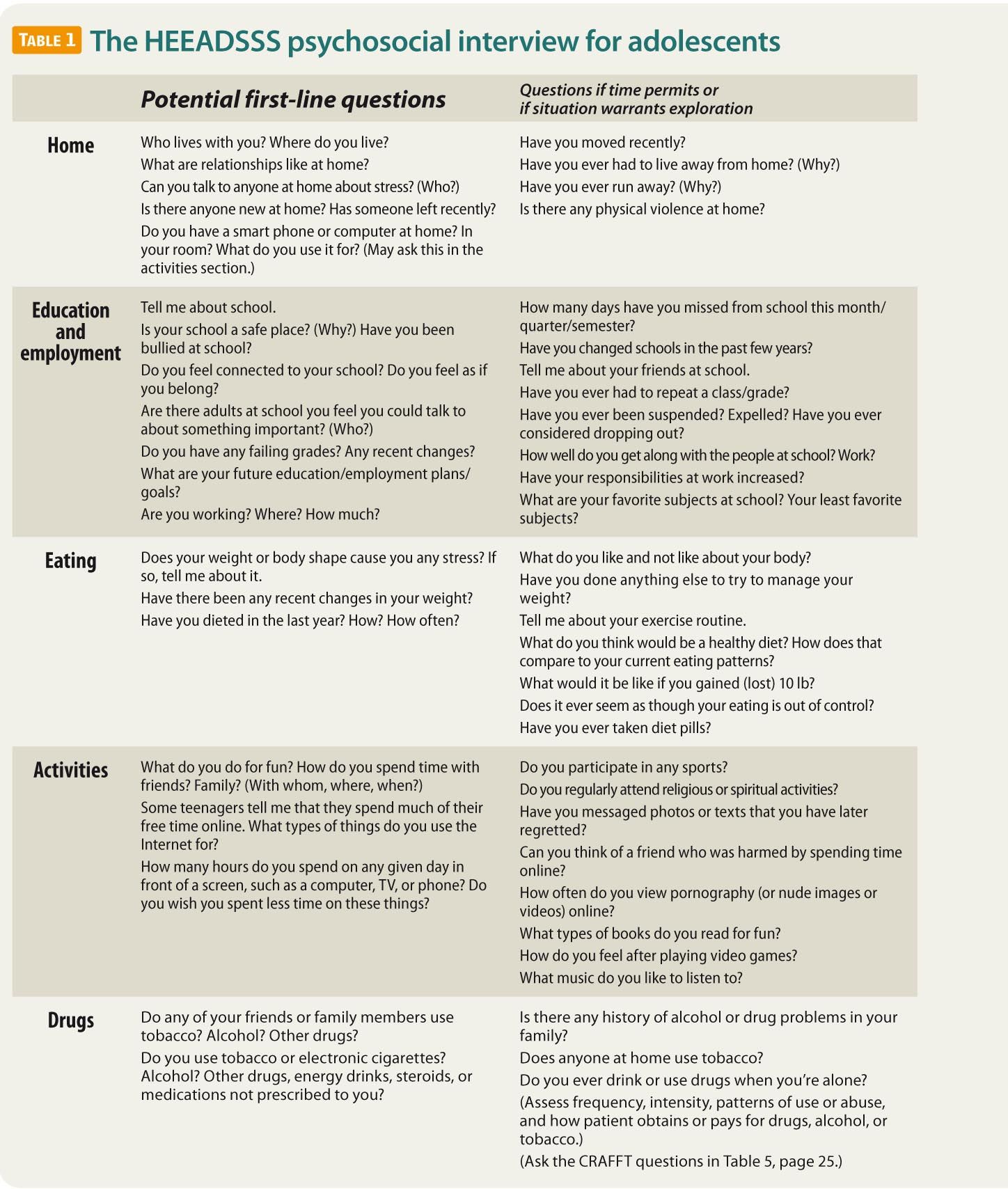
For most teenagers, a psychosocial history is at least as important as the physical exam. This essential psychosocial history can be obtained using the HEEADSSS method of interviewing adolescents. The HEEADSSS interview focuses on assessment of the Home environment, Education and employment, Eating, peer-related Activities, Drugs, Sexuality, Suicide/depression, and Safety from injury and violence (Table 1).1,2
Because adolescence is a time of growth and development when threats to health can arise, these threats are often related to physical and social exploration. For example, sexual exploration may lead to sexually transmitted infections or unintended pregnancies. Experimentation with drugs or alcohol is another cause of morbidity and mortality that is implicated in deadly motor vehicle crashes in the age group. In fact, unintentional injuries, homicide, and suicide are among the leading causes of adolescent deaths in the United States, and are the top 3 causes for those aged 15 years and older.3
Moreover, consequences of adolescents’ stressors may include obesity, eating disorders, depression, or other mental health problems. These issues are not easily identified or addressed using a strictly physiologic orientation.
Without an adequate psychosocial history, one is unlikely to spot problems early enough to significantly reduce adolescent morbidity and mortality. The HEEADSSS interview is a practical, time-tested strategy that physicians can use to obtain a “psychosocial review of systems” for adolescent patients.
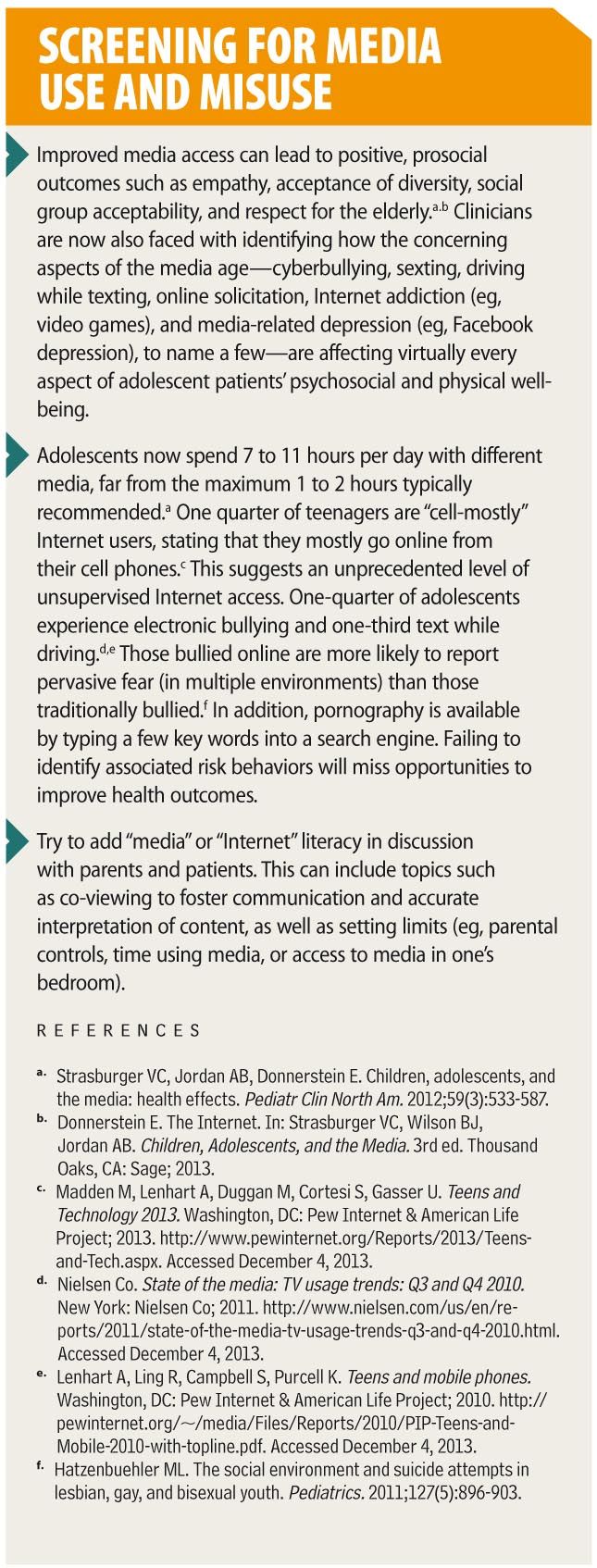
Since the second version of HEEADSSS was created in 2004, nearly all teenagers have obtained access to the Internet and three-quarters of them use cell phones and send text messages.4-7 This utilization of media profoundly affects the lives of adolescents; media may now contribute to 10% to 20% of any specific health problem.7 Thus, questions on new media use are critically important and are included in this HEEADSSS 3.0 update. In addition, this update emphasizes a strengths-based approach to the adolescent interview to foster patient-physician rapport and successful interventions.
How to use the psychosocial screen
You should begin spending time alone with your patients at whatever age they first exhibit the psychosocial changes associated with puberty. Generally, it is preferable to conduct the psychosocial interview when the adolescent is relatively well.8 Nonetheless, situations of crisis or illness may sometimes facilitate effective history taking because vulnerability may foster trusting relationships. At every visit, the adolescent should be assessed for new stressors and overall well-being.
Working with parents
If the parents are present, first introduce yourself to the adolescent to make clear that the teenager is the patient. Then try having the adolescent introduce the other people in the room. Parents, family members, or other involved adults should not be present during the HEEADSSS interview because a parent’s presence is likely to limit how much sensitive information the patient will provide. Allowing a parent to sit in on the interview also makes it more difficult to exclude him or her at subsequent visits when the patient may have more private issues to discuss.
This does not mean that parents should be ignored. Before asking adults to leave the room, always ask whether they have any concerns and assure them of further interaction once the interview is over. Be certain to explain the purpose, such as: “We speak privately with our patients about stressors that may appear during adolescence so they can practice taking responsibility for their health care needs.” With explanation, adults accept the need for confidential care.9
Making a good beginning
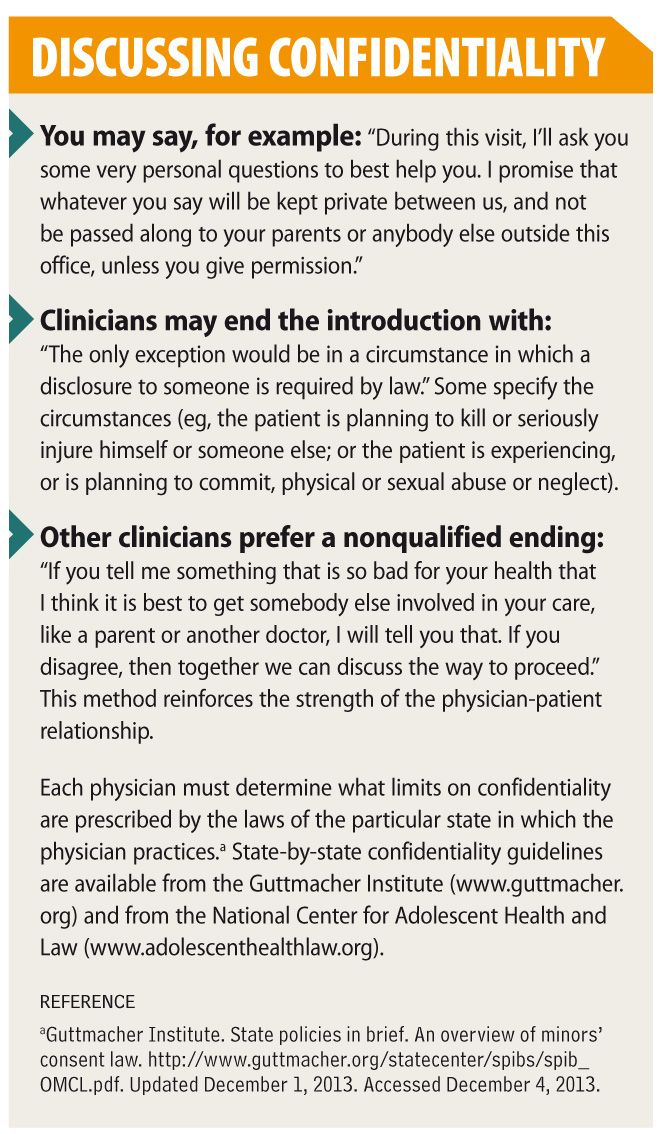
Starting the interview with nonthreatening conversation about the patient’s hobbies or current events may help to ease anxiety, foster rapport and trust, and encourage disclosure. Then you might say: “I would like to take a few minutes to see how you are handling stress and whether your behaviors are safe.”10,11 Once young people start talking, they are likely to keep talking. You will succeed better, however, if you explain the concept and limitations of confidentiality as part of this initial conversation.12,13
The beauty of HEEADSSS is that by using the acronym, you can naturally proceed from very important but usually less threatening questions to those most often considered highly personal. Nothing about the HEEADSSS interview, however, including the order of questioning should ever be treated rigidly. Although teenagers typically feel comfortable progressing in the order of the acronym, be aware of clues from the chief complaint or previous interactions that would modify your approach. For example, the home environment may be much more stressful to some adolescents than any issues they may have about sexuality.
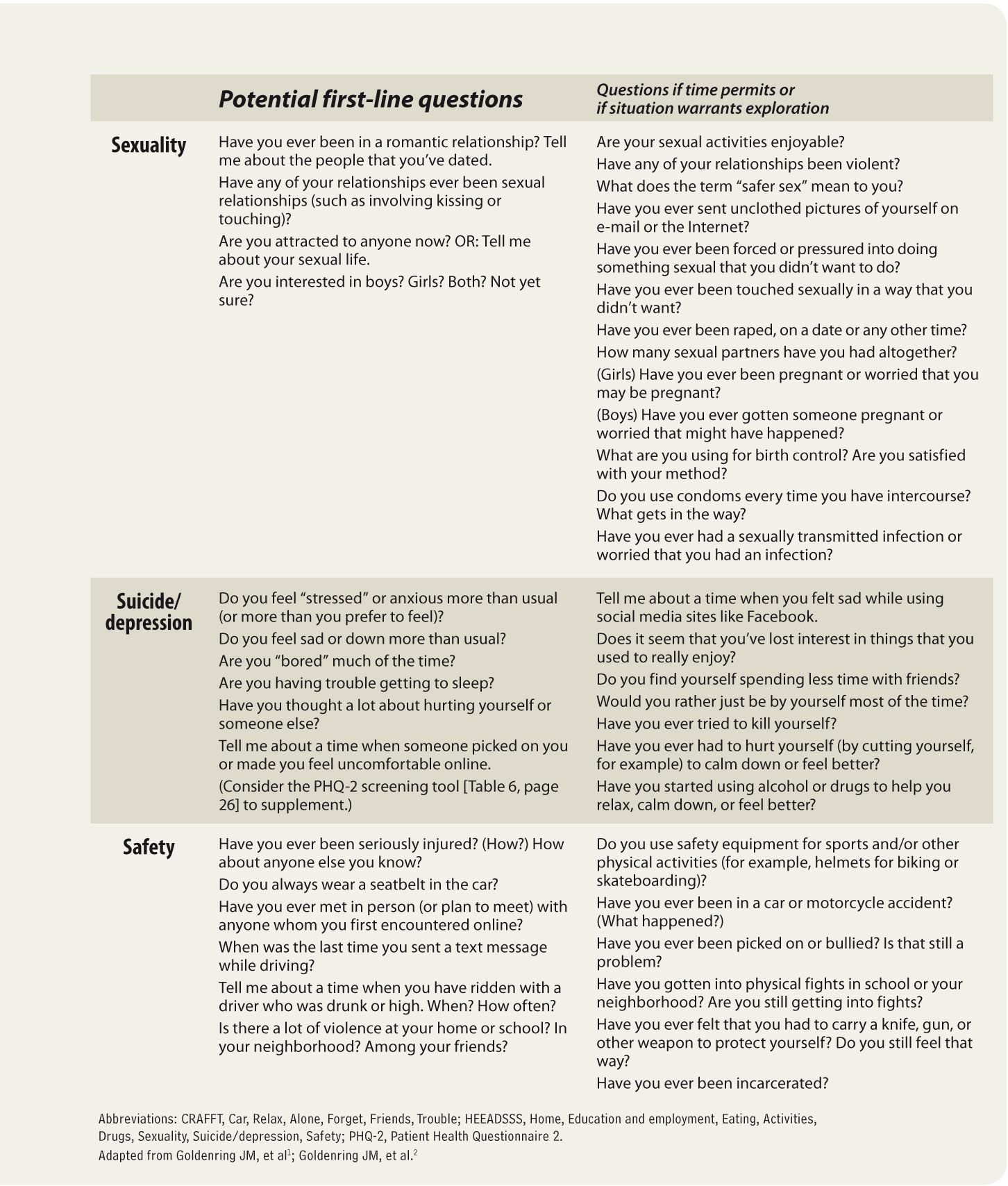
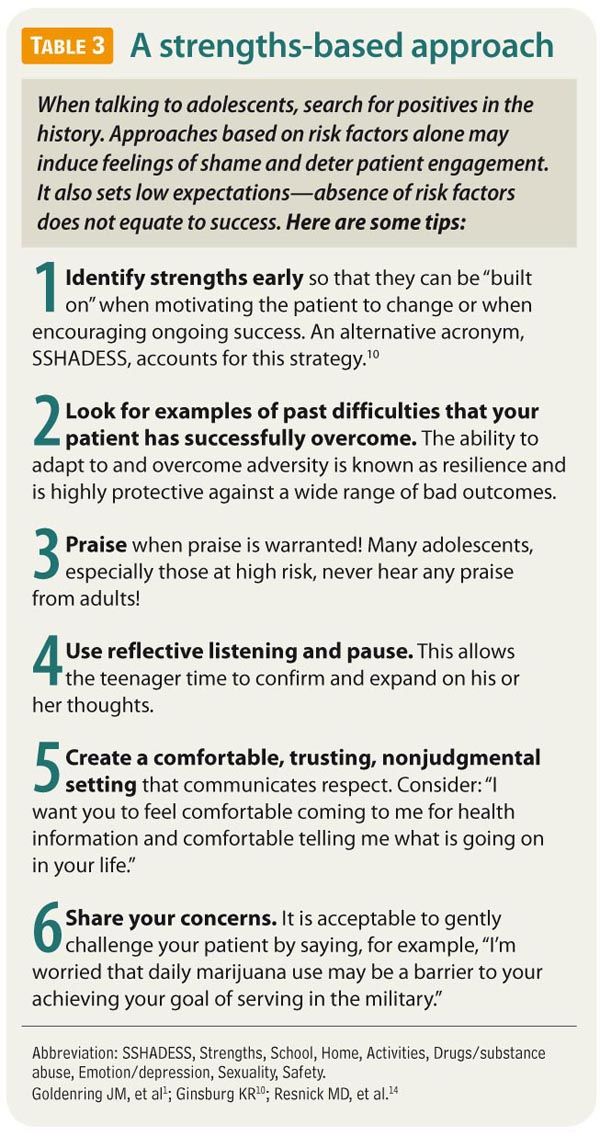
Remember to search for the patient’s strengths because positive attributes suggest the presence of resilience.8,10,11 In fact, some experts recommend first screening for markers of strength and resiliency to use throughout the rest of the visit (Table 2).1,10,14
Consider: “To help me get to know you, tell me something about yourself that makes you proud” or “Tell me how your friends describe you.”10 This may be postponed when patients are anxious to address their psychosocial concerns; however, positive factors may mitigate risks or point to productive interventions or an improved outlook.10,11,14
While counseling about risks you have uncovered, be certain to assess the patient’s readiness to change, the context of the patient’s situation, opportunities to praise the patient for significant accomplishments or avoiding risks, and implementation of patient-created solutions and coping strategies (Table 3).1,10,14
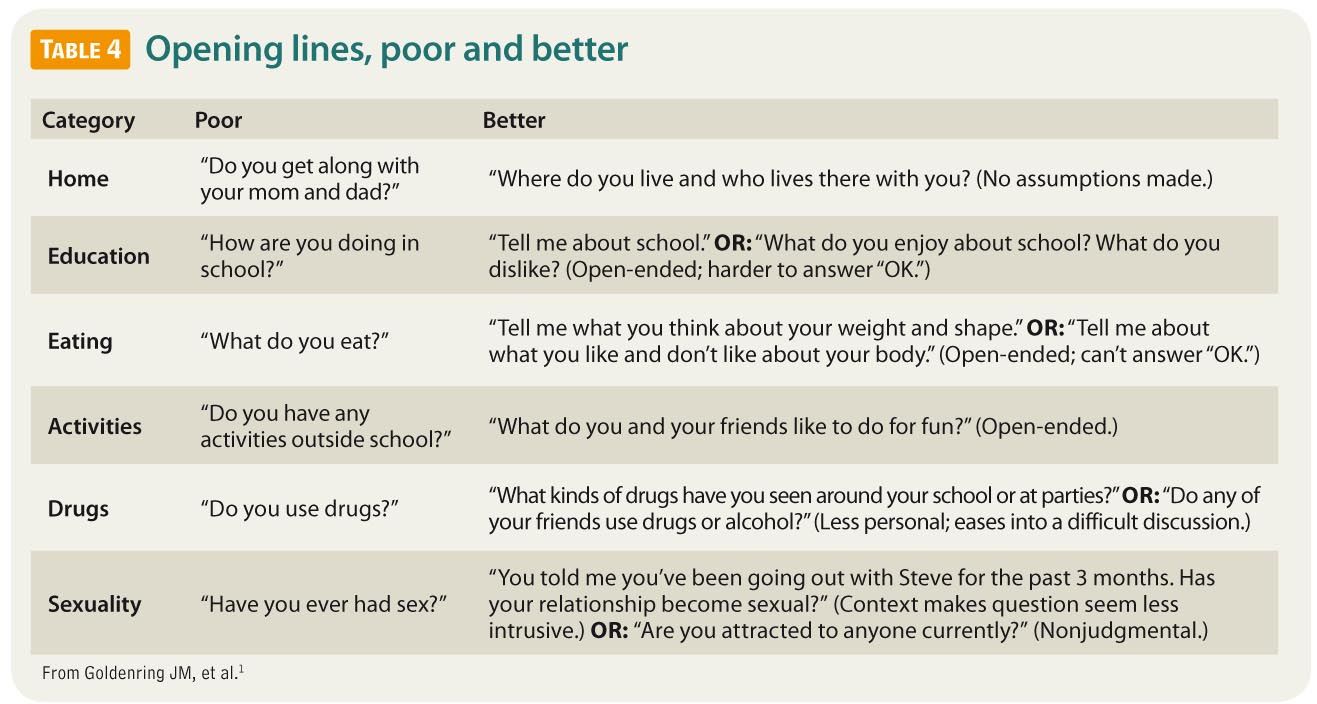
Consider starting at Home
Questions about the teenager's home environment are generally expected and are a good beginning for the psychosocial interview. Instead of making assumptions, ask open-ended questions if possible (Table 4).1 It is a mistake, for example, to say “Tell me about your mom and dad,” which assumes that the patient lives with 2 parents and that the parents are of different genders. Rather, start by asking “Where do you live?” or “Tell me about your living situation.” Then ask: “Who lives with you?” These questions allow the adolescent to describe what is most important in his or her home setting.
Proceed by asking what relationships are like at home and whether there has been a recent change: moving, running away, divorce, or having someone join or leave the household. Such events are often extremely stressful to teenagers, who prefer a stable environment in which to undertake the developmental tasks of adolescence, such as separating from parents, connecting with peers, and developing a positive self-image.
Because media-related morbidity can be reduced by enlisting parental supervision, it is important to screen for the patient’s home use (especially bedroom use) of computers, TVs, video games, smart phones, or other media devices.7 (See “Screening for media use and misuse.”)
It is extremely useful to ask in whom the teenager trusts to confide. Connection to supportive adults-parents or others-is highly protective against many health risks and high-risk behaviors.14 It is also important to remember to praise solid relationships with adults and assumption of responsibilities at home.
E is for Educationand employment
Most young people expect questions about their education and are seldom threatened by them. A common error is to ask “How are you doing in school?” Invariably, the patient will simply answer “fine” or “good,” necessitating additional questioning. Instead, try asking: “Tell me about school. What do you like about it, and what don't you like?”
Search for the patient’s degree of connectedness to the school and education; high connectedness predicts lower rates of substance use, early sexual initiation, violence, school absenteeism, and other causes of adolescent morbidity.14 Connectedness is specifically increased not only by educational commitment and adult mentorship but also by peer group belonging and a safe environment.15 Be certain to inquire about involvement in extracurricular activities and occurrences of bullying.
Ask specifically about academic performance (generally measured by grades). Declining academic performance correlates highly with psychosocial problems, such as drug use or suicide risk, and may indicate an underlying learning or attention disorder.
When a youth lives in a high-risk environment, begin the school section of the interview by ascertaining whether he or she regularly attends school. In some inner-city areas, the absenteeism rate for teenagers ranges from 15% to 40%.16 It also may be helpful to check how many schools and new sets of friends the student has adapted to in recent years. This is particularly important in military families for whom moving is often a way of life.17
The older the teenager, the more you should expect him or her to have some plans for future education or employment. Ask teenagers who are employed part time whether the work is intrusive and if economic circumstances necessitate it. Working more than 20 hours a week has been associated with negative outcomes of emotional distress and substance use.14 When interviewing adolescents who are employed full time, inquire about their strengths and weaknesses on the job, satisfaction level, nature of relationships at work, goals, and recent or frequent changes in employment.
Again, remember to look for and praise successes at school and at work. Such successes include not only academic ones but also leadership and achievement in extracurricular school activities or in the workplace.
E is also for Eating
Adolescents often have unhealthy eating habits, and the prevalence of obesity and eating disorders continues to increase, so questions about nutrition are important. Aim to help all adolescents develop healthy eating (and exercise) habits that can be maintained over a lifetime.
Obesity, which greatly increases the likelihood of developing diabetes and heart disease, is now clearly recognized to begin in childhood and adolescence.18 Sedentary adolescents often snack continually during the time that they spend in front of media devices, compounding their risk. Simple strategies, such as recommending appropriate portion sizes, eliminating sugared soda and fast food, and limiting screen time, can be helpful in improving adolescent eating habits and overall health.7,19
Physicians should also attempt to identify adolescents whose eating habits may signal body image or self-esteem problems, psychologic distress, or depression. Frequent dieting, compulsive exercise, and purging are all of concern. At least half of normal-weight young women surveyed in the United States believe they are overweight.20
Use this question, for example: “As I ask all my patients-does your weight or body shape cause you any stress? If so, tell me about it.” Then follow with specific questions about diet, eating habits, nutritional knowledge and beliefs, and pathologic dieting behaviors. Remember how much eating and exercise behaviors are influenced by genetic inheritance and by behavior modeled in the family or media. In 2010, there were at least 100 easily discoverable pro-anorexia websites encouraging and guiding disordered eating behaviors.21 Media “apps” for calorie counting are widely available and these can be used to increase health and/or contribute to pathologic behavior.
Remember, of course, to praise good diet and exercise choices whenever you find them.
Looking at peer-related Activities
When adolescents or young adults are not at home, in school, or at work, they tend to be with their peers. As a prelude to more sensitive HEEADSSS questions, it is wise to have the patient tell you about what things he or she really enjoys. Adolescents derive much of their identity and self-esteem from peer activities.
Begin by asking: “Tell me what you do with your friends” or “What do you do for fun?” Be concerned about teenagers who cannot readily name friends or describe their activities beyond “hanging out.” They may be at higher risk than teenagers who talk about specific activities with friends, such as sports, dancing, hobbies, games, or even shopping. Adolescents who say they are “bored all the time” may be depressed.
Ask teenagers about the nature and quantity of their use of television, computers, video games, and mobile media devices. Nearly one-third of high school students surveyed in a large nationwide study played video or computer games for 3 hours or longer on the average school day.22 You may uncover a lack of parental connection and control, an avoidance of homework or family/peer interaction, or addictive behavior. Seek the specifics when interviewing an adolescent who endorses constant text messaging or social media posting. This behavior may be detrimental (eg, leading to sexting, texting while driving, or media-related depression) and/or it may be protective (as when used to connect with a health peer group that is otherwise unavailable).
On to Drugs
The drug history is sensitive. For patients in early adolescence, approach the topic obliquely: “We talked about what you and your friends do to have fun. Do any of your friends use drugs or alcohol (or get drunk or high)?” Young adolescents who would not readily talk about their own drug or alcohol use are often very willing to tell about such behavior by their friends. Next you might ask: “Tell me about a time that you felt pressured by friends to use drugs or alcohol, if any.” The answer may lead to a discussion of specific circumstances and types of substances tried.
You may be able to ask older adolescents about drugs more directly. To elicit the most information, you need to know the latest trends of substance use within the patient’s specific community. Substances used may include, for example, new synthetic cannabinoids, caffeine-containing energy drinks, anabolic steroids, and prescription medications such as opioids, benzodiazepines, and stimulants.
Also, ask specifically about tobacco and cigarettes, including electronic cigarettes (inhaled doses of nicotine), because many teenagers do not consider chewing tobacco or smoking to be a form of drug use. Be sure to find out whether the adolescent drives while under the influence of drugs or alcohol and/or rides with drivers who are intoxicated.
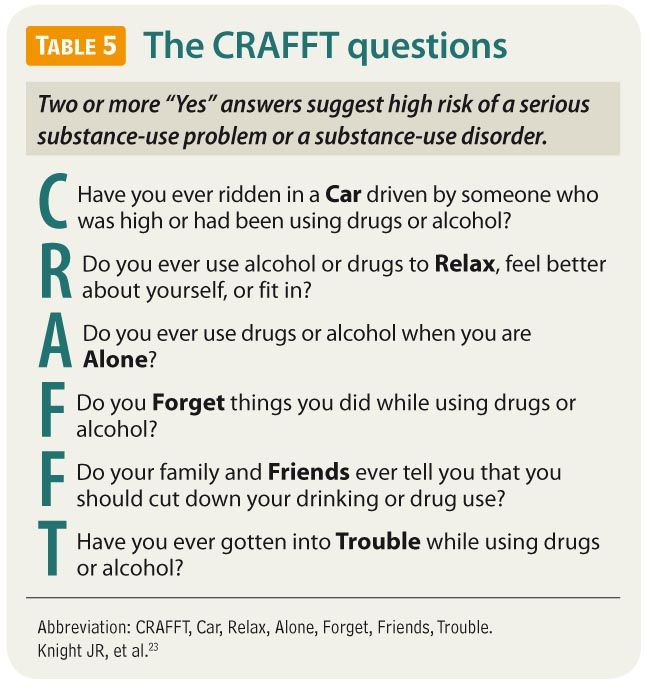
Explaining harms-without also evaluating readiness to change, acknowledging perceived benefits to substance use, using motivational interviewing techniques, and establishing trust and rapport-will likely not suffice to induce behavioral change. CRAFFT (Car, Relax, Alone, Forget, Friends, Trouble) is a brief, validated, office-friendly screening test useful in initially assessing the substance-using teenager (Table 5).23
The goal of obtaining a drug history is usually to have the adolescent reveal the nature of problematic substance use to his or her parents or guardians (with your facilitation, if the patient desires) so that these caregivers can provide the patient with a more robust support system and foster additional treatment. Alternatively, substance use can remain confidential as long as there is no clear and immediate threat to the patient.
Sexuality
The sexual history may be the most sensitive part of the interview. It may benefit rapport to seek permission before proceeding: “Do you mind if I ask you a few more personal questions to learn how I can best assist you?” It is also helpful to expressly acknowledge the discomfort most patients feel about discussing this topic. Say, for example: “I know that this may be embarrassing for you, but I ask these questions of all my teenaged patients to make sure I can give my best advice.”
Especially with younger adolescents, you might observe: “Tell me about any of your friends who are starting to be in romantic relationships.” To older adolescents, simply say: “Tell me about any romantic relationships you've been involved in.” The open-endedness of such questions allows adolescents to tell whether they are having relationships with people of the same sex, the opposite sex, or both.
From asking about relationships, it is a short step to asking about sexual relationships: “Since sexual activity can affect your health, please tell me whether any of your relationships involved kissing or touching?” If so, inquire about other sexual behaviors. Whether to screen for sexually transmitted infections, pregnancy, abuse, and other sequelae of sexual activity depends on the details.
Ask patients about their knowledge of fertility, contraception, and sexually transmitted infections, given that many teenagers use the Internet and social media as their primary sex educators. You might add: “Many people do not have anyone knowledgeable to talk to about sex. We're always happy to answer any questions you have.” And remember, adolescents may forgo contraceptive or reproductive services if they think (rightly or wrongly) that parental notification is mandatory.12,13
Do not assume that adolescents who are having sexual experiences are comfortable about it. You may say: “Some of my patients tell me they feel pressured or coerced into having sex. Have you ever felt this way?” Sometimes, you can serve as a trustworthy adult who gives adolescents permission to avoid sexual activity until they are more comfortable with engaging in it. A history of abuse (if any) may not come out on the first interview, but the very fact that you show interest establishes rapport and may lead the patient to reveal the facts at a later time.
In today’s Internet-linked world, sexual materials of all kinds are easily available. You may wish to ask teenagers about what sexual information and materials they have accessed online and how much and how often. Again, some experimentation with this is likely normal, but excessive use of such sites or accessing unusual or violent sexual content may indicate a risky behavior.7
Sometimes the greatest impediment to obtaining an adequate sexual history is a physician’s own discomfort with sexuality. With practice, these questions become easier to ask without appearing judgmental. You can offer advice and personal opinions, but only if the teenager solicits them and only if you clearly label them as such.
Screening for Suicideand depression
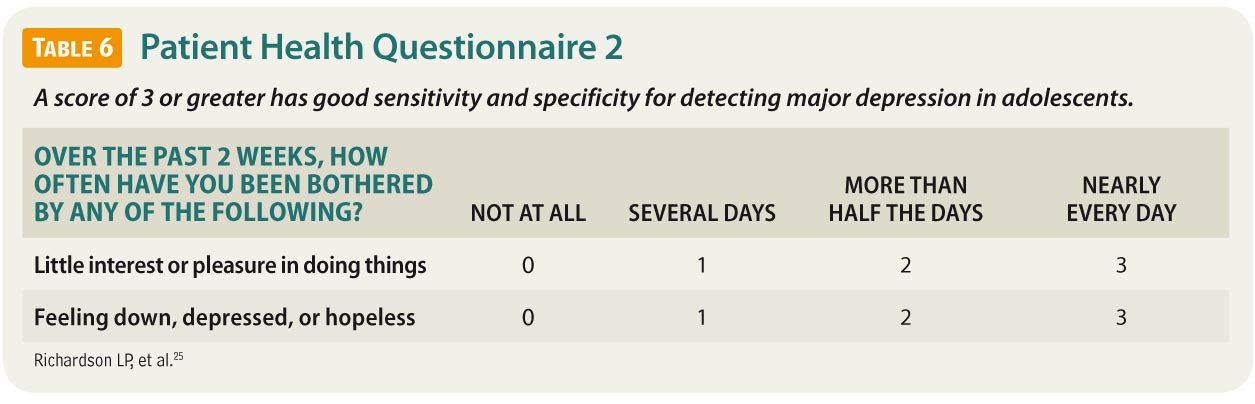
Adolescents should be screened for depression when systems are in place to ensure accurate diagnosis, psychotherapy, and follow-up.24 Teenagers often exhibit depression as boredom, irritability, anxiety, moodiness, sleep disturbance, and social withdrawal. Many are more willing to admit to “stress” than to overt depression or sadness. The Patient Health Questionnaire 2 (PHQ-2), a 2-item survey, may be used as an initial screening tool for depression in adolescents at each visit (Table 6).25
When depression seems likely, ask directly and clearly about self-harm. Asking about suicidal behavior does not precipitate or trigger it, and clinicians should not be reluctant to question patients unambiguously: “You’ve told me that you’ve been feeling bad lately. Have you felt so bad that you’ve thought seriously about harming yourself?” Adolescents attempt suicide more often than we realize, so physicians should not be surprised if a teenager has contemplated or even attempted it. Past suicide attempts are a strong risk factor for future attempts and future suicide. The clinical question is: How serious is the ideation, planning, or actual behavior?
Pay attention to sexual orientation. A recent study found that lesbian, gay, and bisexual (LGB) adolescents were more likely than heterosexual teenagers to have attempted suicide in the previous 12 months (21.5% vs 4.2%, respectively).26 The likelihood of attempting suicide was 20% higher for LGB teenagers in unsupportive environments than in supportive environments. Sexual minority adolescents benefit greatly from clinician-provided support, as well as a safe place for asking questions.
Some adolescents who are not contemplating suicide nevertheless harm themselves. Teenagers who engage in cutting describe it as a mood-stabilizing behavior; in these situations a careful risk assessment is important.
S for Safety
Injuries, suicide, and homicide-the major causes of morbidity and mortality in adolescents-are a constant environmental reality for many young people. Antecedents such as bullying, domestic and school violence, gang involvement, sexual abuse, online solicitation, and access to weapons must be identified in the psychosocial history. Family violence, which increases the risk for teenaged violence several-fold, occurs in all social and economic classes, as does dating violence, which is reported by as many as 25% of teenaged and young adult women.27,28
Proceed to questions about the threats most prevalent in the patient’s community. In some settings, these threats may be school violence and guns; in other settings, these may be sports injuries, sexual violence, or risk taking related to motor vehicles. Then ask about any other threats. Avoid letting assumptions based on the patient’s racial, ethnic, or socioeconomic status lead you to skip taking parts of the history.
Find out what strategies the patient uses for self-protection, conflict resolution, and avoidance of violence. (No gangs? How about local bullies? Is there an abusive partner or parent?) Know the school-based and community organizations in your area that offer programs on conflict resolution and violence avoidance so that you can make specialized referrals. Many young people respond to violence with violence because that is all they know from their homes, streets, and media. Before offering concrete solutions, ask adolescents whether they can think of ways to avoid violence using their reported strengths.
Wrapping it up
You may end the psychosocial interview by asking adolescents to tell you in whom they can trust and confide if they have problems. Emphasize that your approach is nonjudgmental and that you welcome future visits. You may say: “I’m here for you, and I want you to feel comfortable confiding in me. If you have something personal to talk about, I’ll try to give you my best advice and answer your questions.”
Take me to the HEADDSSS Resource Center!
Many adolescents do not recognize dangerous behavior patterns as dangerous because they see their activities not as problems but as solutions. Your challenge is to explore these behaviors and the context in which the adolescent lives, and to develop realistic solutions with patient buy-in.10,11 Depending on the nature of the risk factors identified and the intervention to be established, you can either extend the initial visit or arrange a follow-up.
Finally, by now you may be overwhelmed by the amount of issues to be covered in this interview and wonder how to do this in a limited time. Of course, you cannot cover every aspect in a single visit, but your goal is to establish an effective relationship in each case and leave the remaining questions for a later visit. You should feel free to add or remove priority questions based on the needs of your patient population. In other words, make HEEADSSS your own.
Try getting into the HEEADSSS of your adolescent patients. Your effort may have a lifelong impact.
Dedication
This manuscript is dedicated to the memory of David Rosen, MD, and Eric Cohen, MD, for their significant contributions to previous versions of the HEEADSSS psychosocial history and to the field of adolescent medicine.
REFERENCES
1. Goldenring JM, Rosen DS. Getting into adolescent heads: an essential update. Contemp Pediatr. 2004;21(1):64-90.
2. Goldenring JM, Cohen E. Getting into adolescent heads. Contemp Pediatr. 1988;5(7):75-90.
3. Centers for Disease Control and Prevention. Health, United States, 2012. Table 23: Leading causes of death and numbers of deaths, by age: United States, 1980 and 2010. http://www.cdc.gov/nchs/data/hus/2012/023.pdf. Updated May 30, 2013. Accessed December 4, 2013.
4. Nielsen Co. State of the media: TV usage trends: Q3 and Q4 2010. New York: Nielsen Co; 2011. http://www.nielsen.com/us/en/reports/2011/state-of-the-media-tv-usage-trends-q3-and-q4-2010.html. Accessed December 4, 2013.
5. Lenhart A, Ling R, Campbell S, Purcell K. Teens and mobile phones. Washington, DC: Pew Internet & American Life Project; 2010. http://pewinternet.org/~/media/Files/Reports/2010/PIP-Teens-and-Mobile-2010-with-topline.pdf. Accessed December 4, 2013.
6. Madden M, Lenhart A, Duggan M, Cortesi S, Gasser U. Teens and Technology 2013. Washington, DC: Pew Internet & American Life Project; 2013. http://www.pewinternet.org/Reports/2013/Teens-and-Tech.aspx. Accessed December 4, 2013.
7. Strasburger VC, Jordan AB, Donnerstein E. Children, adolescents, and the media: health effects. Pediatr Clin North Am. 2012;59(3):533-587.
8. Adolescence. In: Hagan JF Jr, Shaw JS, Duncan PM, eds. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008:515-575. http://brightfutures.aap.org/pdfs/Guidelines_PDF/18-Adolescence.pdf. Accessed December 4, 2013.
9. Hutchinson JW, Stafford EM. Changing parental opinions about teen privacy through education. Pediatrics. 2005;116(4):966-971.
10. Ginsburg KR. Viewing our adolescent patients through a positive lens. Contemp Pediatr. 2007;24(1):65-76.
11. Ginsburg KR. Engaging adolescents and building on their strengths. Adolesc Health Update. 2007;19(2):1-8.
12. Jones RK, Purcell A, Singh S, Finer LB. Adolescents’ reports of parental knowledge of adolescents’ use of sexual health services and their reactions to mandated parental notification for prescription contraception. JAMA. 2005;293(3):340-348.
13. Ford CA, Millstein SG, Halpern-Felsher BL, Irwin CE Jr. Influence of physician confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A randomized control trial. JAMA. 1997;278(12):1029-1034.
14. Resnick MD, Bearman PS, Blum RW, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823-832.
15. Centers for Disease Control and Prevention. School Connectedness: Strategies for Increasing Protective Factors Among Youth. Atlanta, GA: US Department of Health and Human Services; 2009. http://www.cdc.gov/healthyyouth/adolescenthealth/pdf/connectedness.pdf. Accessed December 4, 2013.
16. Balfanz R, Byrnes V. Chronic Absenteeism: Summarizing What We Know From Nationally Available Data. Baltimore, MD: Johns Hopkins University Center for Social Organization of Schools; 2012.
17. Jeffreys DJ, Leitzel JD, Cabral G, et al. Military Adolescents: Their Strengths and Vulnerabilities. MFI Technical Report 97-4. Scranton, PA: Military Family Institute, Marywood University; 1997:1-93.
18. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128 (suppl 5):S213-S256.
19. Jordan AB. Children’s television viewing and childhood obesity. Pediatr Ann. 2010;39(9):569-573.
20. Strauss RS. Self-reported weight status and dieting in a cross-sectional sample of young adolescents: National Health and Nutrition Examination Survey III. Arch Pediatr Adolesc Med.1999;153(7):741-747.
21. Borzekowski DL, Schenk S, Wilson JL, Peebles R. e-Ana and e-Mia: a content analysis of pro-eating disorder web sites. Am J Public Health. 2010;100(8):1526-1534.
22. Eaton DK, Kann L, Kinchen S, et al; Centers for Disease Control and Prevention (CDC). Youth risk behavior surveillance-United States, 2011. MMWR Surveill Summ. 2012;61(4):1-162.
23. Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607-614.
24. US Preventive Services Task Force. Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2009;123(4):1223-1228.
25. Richardson LP, Rockhill C, Russo JE, et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125(5):e1097-e1103.
26. Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics. 2011;127(5):896-903.
27. Rickert VI, Wiemann CM. Date rape among adolescents and young adults. J Pediatr Adolesc Gynecol. 1998;11(4):167-175.
28. Committee on Injury, Violence, and Poison Prevention. Policy statement-role of the pediatrician in youth violence prevention. Pediatrics. 2009;124(1):393-402.
DR KLEIN is an adolescent medicine fellow, Department of Pediatrics, San Antonio Military Medical Center, Fort Sam Houston, Texas. DR GOLDENRING is an adolescent medicine specialist, medical director, and a medical-legal consultant, Oceanside, California. DR ADELMAN is an adolescent medicine specialist and associate professor, Department of Pediatrics, Uniformed Services University of the Health Sciences, Bethesda, Maryland. The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Air Force, the US Army, or the US military at large. The authors have nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.