Juvenile Laryngeal Papillomatosis in a 30-Month-Old Girl
The patient had been born at term following an uncomplicated pregnancy and labor. Her growth and development were appropriate. Her immunizations were up-to-date. At about 1 year of age, she began to have "wheezing" episodes. Moderate persistent asthma was diagnosed, and treatment with fluticasone and inhaled albuterol was initiated.
A 30-month-old girl presented to the emergency department with a 2-day history of shortness of breath, cough, and "wheezing."
The patient had been born at term following an uncomplicated pregnancy and labor. Her growth and development were appropriate. Her immunizations were up-to-date. At about 1 year of age, she began to have "wheezing" episodes. Moderate persistent asthma was diagnosed, and treatment with fluticasone and inhaled albuterol was initiated.
Her current illness started 2 weeks earlier, with gradually worsening hoarseness, mild rhinorrhea, and cough. Her breathing was noisy. There was no report of fever or choking episodes. A review of systems was otherwise normal.
A presumptive diagnosis of croup was made. The patient received racemic nebulized epinephrine and intramuscular injections of dexamethasone. When her symptoms did not improve, nebulized albuterol was administered without benefit. The patient was hospitalized.
Physical examination showed a nontoxic-appearing afebrile child who was well perfused and hydrated. However, she required 1 liter of oxygen by nasal cannula to maintain an oxygen saturation level above 93%. Her voice was hoarse. She had biphasic stridor and labored breathing. There was no rhinorrhea or drooling. Her oropharynx appeared normal; there were no hemangiomas or goiter. Brachial pulses were equal in both arms. The quality of the stridor was not affected by neck flexion or assumption of a prone position. Lung fields were clear except for transmitted sounds. There were no other abnormal physical findings.
IS THIS CROUP?
Croup typically manifests with stridor-usually on inspiration-of acute onset following an upper respiratory tract infection (URI). A gradual worsening of symptoms, lack of any signs of URI, the presence of hoarseness and hypoxia, and failure to respond to the conventional management of croup suggested an alternate diagnosis. Further studies were done to determine the cause.
DIFFERENTIAL DIAGNOSTIC CONSIDERATIONS
A thorough head-to-foot examination may sometimes point to the cause of stridor in a child. For example, a dolicocephalic skull in an infant born prematurely with a history ofventilation problems may indicate subglottic narrowing. Any sign of hydrocephalus should raise suspicion of an Arnold-Chiari malformation leading to stridor. Hemangiomas, particularly those in the "beard area," may indicate a hemangioma in the larynx. A goiter or any other neck mass may point to a retrosternal extension that compresses the airways.
Flexion of the neck may exacerbate stridor caused by vascular rings or slings. If an aberrant right subclavian artery compresses the airways, the brachial pulses may be unequal. Stridor from laryngomalacia diminishes when the patient assumes a prone position. A weak or abnormal cry from birth indicates either vocal cord paralysis or a web.
In extrathoracic obstruction, the vibratory sound of stridor is inspiratory; in intrathoracic obstruction, it is expiratory. When obstruction is evident during both phases of breathing, the obstruction may be variable and may simultaneously affect both the intrathoracic and extrathoracic airways. If this has not occurred, the obstruction may have become critical.1
The Table lists causes of recurrent or persistent stridor in children.2

Table
WHAT INVESTIGATIONS ARE REQUIRED AT THIS STAGE?
Radiographs were taken of the patient's neck (Figure 1). The films showed a soft tissue shadow in the region of the vocal cords. Chest films showed normal findings.
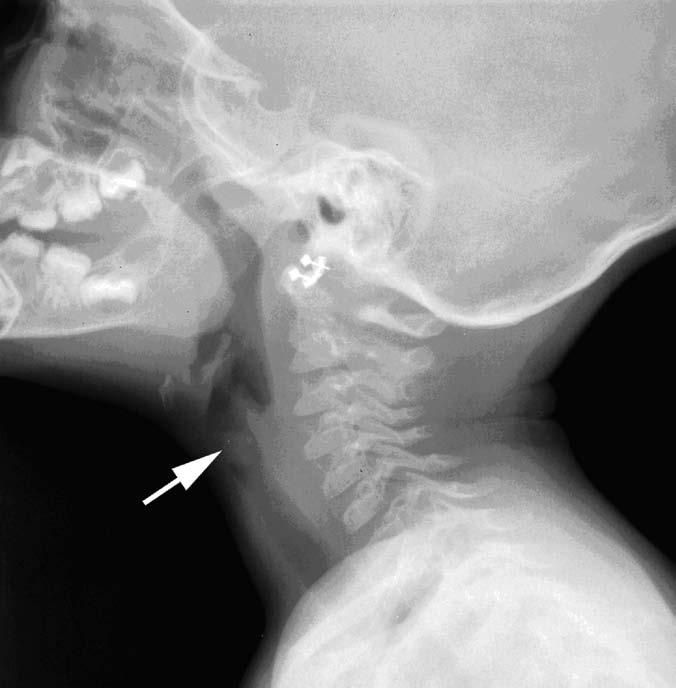
Figure 1 - A radiograph of the neck shows a soft tissue shadow at the vocal cord level.
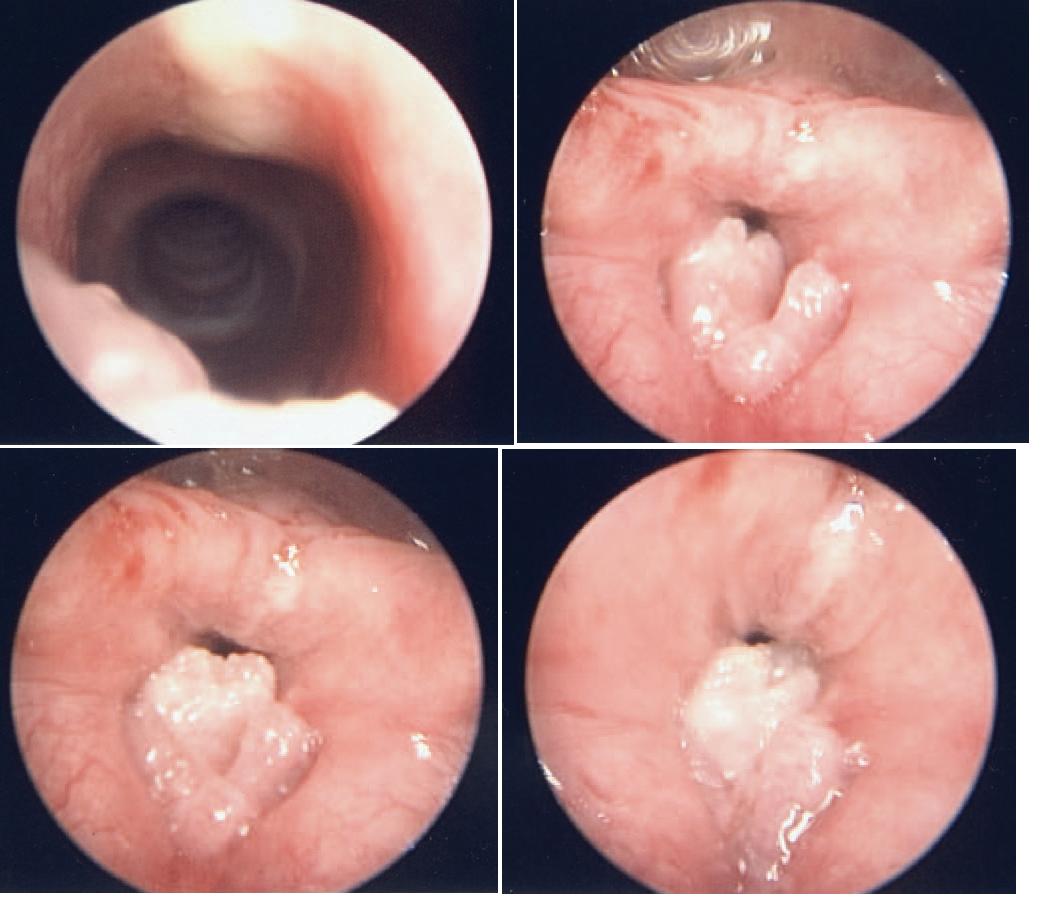
Figure 2 - These microlaryngoscopic pictures of the larynx show multiple papillomas.
The soft tissue irregularity on the vocal cords was of concern. Possibilities included a growth on the vocal cord or a non-radiopaque foreign body. Consultation with an otorhinolaryngologist was obtained, and surgery was recommended. Microlaryngoscopy showed papillomalike lesions on the vocal cord that almost obstructed the airway (Figure2). The lesions were surgically excised. The histological picture was consistent with papillomatosis.
JUVENILE LARYNGEAL PAPILLOMATOSIS
Epidemiology. Juvenile laryngeal papillomatosis-also known as juvenile respiratory papillomatosis or recurrent respiratory papillomatosis- is relatively uncommon. It is usually characterized by wart-like exophytic lesions that have a predilection for the larynx. The estimated incidence is 4.3 cases per million; the estimated cost of care in the United States ranges from $40 million to $123 million annually.3,4
Etiology. Juvenile laryngeal papillomatosis is caused by viral infection; the most common culprit is human papillomavirus (HPV) subtypes 6 and 11-the subtypes implicated in genital condylomata. There is strong evidence that the condition is acquired during childbirth. Retrospective studies suggest that about 30% of children who have juvenile laryngeal papillomatosis at a young age are born to mothers with genital condylomata at the time of delivery.5 Additional subtypes, such as 16 and 18, have been identified in juvenile laryngeal papillomas and are thought to pose a great risk for malignant transformation in approximately 2% of cases.6
Presenting symptoms. Juvenile laryngeal papillomatosis usually presents in young children, typically during infancy. Hoarseness is a common initial presentation. Stridor usu-ally occurs in later stages of the disease when the airway is obstructed.
Initially, the condition may be misdiagnosed as asthma, croup, or bronchitis.7 In most children, the condition presents acutely after a viral URI, which can further mislead the clinician. When hoarseness persists in children for more than 6 weeks, or when an acute airway obstruction does not respond to racemic epinephrine or bronchodilator therapy, careful thought should be given to the differential diagnosis, and further otolaryngology workup must be arranged.
Diagnosis. The diagnosis of juvenile laryngeal papillomas must be confirmed by direct laryngoscopy. In radiographs of the neck, however, the lesions may appear as subtle changes in the soft tissue-as in this case.
Therapy. There is no definitive treatment modality available for juvenile laryngeal papillomas. The goal of therapy is to diminish the airway obstruction and improve voice quality. The most common method of treatment is excision of the lesions by microlaryngeal surgery. Excision may be performed with different modalities, such as a microlaryngeal instrument, a carbon dioxide laser, microdebrider, or pulsed dye laser.
Many surgeons still prefer microlaryngeal surgery-the oldest method-because healthy tissue is not damaged, thus preventing scarring and persistent hoarseness. Disadvantages include aspiration of blood or fragments of papillomatous tissue into lower airways after the surgery.3
In a 1995 survey of otolaryngologists, a task force on recurrent respiratory papillomas reported that 92% of respondents preferred the carbon dioxide laser for initial treatment; the remaining 8% favored cold excision.4 However, recent studies have shown the pulsed dye laser to be useful in minimizing papilloma burden without scarring; the procedure is shorter and there is less associated morbidity. Moreover, it can be performed in the office.8,9
Treating recurrent lesions. Papillomas tend to recur, and repeated excisions are not uncommon. It is very difficult to eradicate the papillomavirus from mucosal surface.
Approximately 10% of patients with recurrent respiratory papillomatosis require adjuvant therapy. Such therapy is indicated when recurrences necessitate surgery more than 4 times in a year, when rapid regrowth of papillomas compromise the airway, or when there is distal spread.10 Numerous agents, including isotretinoin, alpha interferon, indole-3- carbinol, methotrexate, acyclovir, and ribavirin, have been tried. None has gained widespread acceptance because of systemic toxicity and dosing.
Cidofovir has antiviral activity against a number of DNA viruses, including herpes simplex virus and cytomegalovirus.11 Intralesional injections of this agent are currently recommended for patients with frequent recurrences. However, reports of carcinogenesis in animal studies have limited the widespread use of cidofovir.12
Tracheotomy is indicated if lesions completely obstruct the airway, or if the airway cannot be secured by intubations. Otherwise, tracheotomy should be avoided as much as possible to prevent dissemination of the papillomas to the rest of the respiratory tract.
Prevention. The currently available prophylactic quadrivalent HPV (6, 11, 16, 18) vaccine is highly effective in preventing cervical lesions. The combined efficacy against persistent infection with HPV types 6, 11, 16, and 18 was 90% thirty months after vaccination.13 Whether administration of this new HPV vaccine to female children and adolescents will prevent or reduce the incidence of juvenile laryngeal papillomatosis will become clear after a substantial period of use.
THE BOTTOM LINE
Pediatricians and emergency medicine physicians should entertain a wide differential in children with stridor that does not respond to conventional therapy for croup. Hypoxia is a sign of airway obstruction. Juvenile laryngeal papillomatosis is a rare condition that requires a high index of suspicion- and timely consultation with an otolaryngologist.
References:
- Brown MA, Morgan WJ, eds. Evaluation of the child with airway obstruction. In: Textbook of Pediatric Respiratory Medicine. New York: Mosby; 1999:145-146.
- Boat TF, Green TP. Chronic or recurrent respiratory symptoms. In: Kliegman R, Nelson WF, Behrman RE, et al, eds. Nelson Textbook of Pediatrics. 18th ed. Philadelphia: WB Saunders; 2007:1758-1762.
- Bishai D, Kashima H, Shah K. The cost of juvenile- onset recurrent respiratory papillomatosis. Arch Otolaryngol Head Neck Surg. 2000;126:935-939.
- Derkay CS. Task force on recurrent respiratory papillomas: a preliminary report. Arch Otolaryngol Head Neck Surg. 1995;121:1386-1391.
- Aaltonen L, Rihkanen H, Vaheri A. Human papilloma in larynx. Laryngoscope. 2002;112:700-707.
- Altman KW. Vocal fold masses. Otolaryngol Clin North Am. 2007;40:1091-1108.
- Derkay CS, Darrow DH. Recurrent respiratory papillomas. Ann Otol Rhinol Laryngol. 2006;115:1-11.
- Valdez TA, McMillan K, Shapshay SM. A new laser treatment for vocal cord papilloma-585-nm pulsed dye. Otolaryngol Head Neck Surg. 2001;124: 421-425.
- Koufman JA, Rees CJ, Frazier WD, et al. Officebased laryngeal laser surgery: a review of 443 cases using three wavelengths. Otolaryngol Head Neck Surg. 2007;137:146-151.
- Green GE, Bauman NM, Smith RJ. Pathogenesis and treatment of juvenile onset recurrent respiratory papillomatosis. Otolaryngol Clin North Am. 2000;33:187-207.
- De Clercq E. Therapeutic potential of Cidofovir (HPMPC, Vistide) for the treatment of DNA virus (i.e. herpes-, papova-, pox- and adenovirus) infections. Verh K Acad Geneeskd Belg. 1996;58:19-49.
- Derkay C; Multi-disciplinary Task Force on Recurrent Respiratory Papillomas. Cidofovir for recurrent respiratory papillomatosis (RRP): a re-assessment of risks. Int J Pediatr Otorhinolaryngol. 2005;69:1465-1467.
- Villa LL, Costa RL, Petta CA, et al. Prophylactic quadrivalent human papillomavirus (types 6, 11, 16, and 18) L1 virus-like particle vaccine in young women: a randomised double-blind placebo-controlled multicentre phase II efficacy trial. Lancet Oncol. 2005;6:271-278.