The latest news about minimally invasive surgery
Is MIS the best bet for a patient with Hodgkin's disease who needs a splenectomy? What about an ordinary hernia repair, or a child who may have appendicitis, or the teenager who might have an ectopic pregnancy?
The latest news about minimally invasive surgery
Is MIS the best bet for a patient with Hodgkin's diseasewho needs a splenectomy? What about an ordinary hernia repair, or a childwho may have appendicitis, or the teenager who might have an ectopic pregnancy?
Minimally invasive surgey (MIS) has made great strides since the firstlaparoscopic cholecystectomy was performed in 1987, in France by Mouret.Since then, the list of procedures performed laparoscopically has grownuntil it essentially duplicates the list of procedures done in an open fashion.The advantages of laparoscopic procedures are obvious: smaller, cosmeticallymore acceptable incisions; shorter recovery time; less discomfort. But theseadvantages may not outweigh the drawbacks: higher instrument costs, forsome procedures; problems of access to pediatric surgeons with the necessarytraining and experience; possibly heightened risk. Certainly, an MIS procedureshould not be recommended unless the results are at least as satisfactoryas those that can be obtained in open surgery.
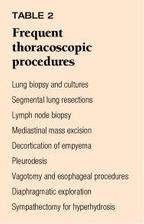
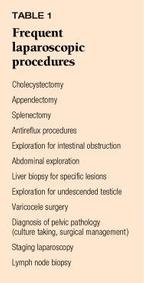
Our overview of this rapidly evolving field will help you make the choicesthat are best for your patients. We will describe the pros and cons of themost popular MIS procedures and let you in on some of the newest applications--fromadrenalectomy to the diagnosis of Pneumocystic carinii pneumonia in AIDSpatients. The most frequently performed laparoscopic procedures are listedin Table 1. Thoracoscopic procedures are listed in Table 2.
The technology evolves
In the 1950s, when gynecologists first began to use laparoscopy routinelyfor diagnostic purposes, they worked with open tube instruments derivedfrom the early esophagoscopes and sigmoidoscopes. The light sources wereprimitive, and the field of vision was restricted to organs very near thedistal end of the open tube. Only one person at a time could view the pelvicstructures, and a vivid imagination was an asset when describing the pathologythat might be present.
The development of rod lenses by Hopkins in England and the incorporationof fiberoptic bundles into the body of the laparoscopes greatly brightenedand enlarged the field of view. The unwieldy beam splitters used to allowassistants to share the surgeon's view were replaced by progressively smallerTV cameras that allow everyone involved in the operation to see, contribute,and learn at the same time.
In addition to the new viewing modalities, ingenious instruments weredevised to allow handling and manipulation of structures within the abdomen.The most remarkable of these was a multifiring clip applier, which permittedcontrolled cutting of vessels and ducts. Specialized catheters were developedfor intraoperative cholangiograms, and bipolar scissors and forceps wereinvented that made cauterization of bleeding points easier and safer. Inbipolar instruments, the cauterizing current does not pass through the patientbut rather goes down one arm of the instrument through the tissue and thenback up the second arm, reducing the chances of intra-abdominal injury andelectrical disturbances of conduction.
One of the newest instruments developed for MIS and used extensivelyin many procedures is the harmonic scalpel. It uses high-frequency ultrasonicenergy to cut and coagulate; since no current passes through the patient,no grounding is needed. Small vessels (up to 2 to 3 mm in diameter) maybe coagulated and cut safely without the use of clips, rendering the procedurefaster and eliminating the interference from clips that can complicate computedtomographic (CT) scans done later.
Gall bladder surgery: Still number one
Laparascopic gall bladder surgery, the procedure that launched the modernMIS era, is still one of the most commonly performed laparoscopic proceduresin children and adolescents. Hematologic diseases such as spherocytosisand sickle cell disease are common indications for cholecystectomy in children,as well as calculous and acalculous cholecystitis of idiopathic origin.The results are similar to those in adults, with a low incidence of complications,and this method has become the "gold standard" for treating biliarydisease.1 While early patients had a higher incidence of commonduct injury than patients operated with open cholecystectomy, the rate ofinjury now very closely approaches that of open surgery and continues todecrease.2
Appendectomy: Still controversial
While minimally invasive gall bladder surgery has become relatively common,using these techniques in appendectomy remains controversial.3In cases where the preoperative diagnosis is clearly acute appendicitis,most surgeons prefer the time-honored, open technique through a small transverseright lower quadrant (RLQ) incision. In small patients, the sum of the mini-trocarincisions used in MIS appendectomy is no less than the RLQ incision.
When the diagnosis is equivocal and a wider, more thorough abdominalexploration may be necessary, however, laparoscopy has many advantages.Often the absence of appendicitis can be documented, samples for culturetaken, and appropriate treatment initiated, for example in cases of primaryperitonitis. In adolescent females with lower abdominal pain, the diagnosisis sometimes unclear, and an exploratory laparoscopy can help decide whethera surgical approach is appropriate.4
A perforated appendicitis is not a contraindication to laparoscopic exploration,as effective peritoneal toilet as well as appendectomy may be performedin those difficult cases. It is not yet clear if MIS will become an acceptedtreatment modality for this indication. Interval appendectomies may alsoprove to be ideal situations for the use of MIS, because significant adhesionsare sometimes present following a missed appendicitis and three or foursmall trocar incisions are preferable to an extended McBurney or Rocky-DavisRLQ incision.
Splenectomy: Sometimes feasible, sometimes not
Many of the same hematologic diseases that cause biliary disease alsoare indications for splenectomy. Idiopathic thrombocytopenic purpura thatdoes not respond to medical therapy can often be improved by splenectomy,and spherocytosis symptoms can be alleviated by removal of the spleen. Inaddition, splenectomy is included in staging for Hodgkin's disease and othermalignancies, and the requisite biopsies may also be performed with MIS.The chances for complete remission in all these diseases are best when thesurgeon identifies and removes all accessory spleens. This can be done duringthe primary MIS procedure and, when necessary, as a second procedure regardlessof which method was used during the first operation.5
Laparoscopic splenectomy, when feasible, is advantageous because of thesignificantly smaller incisions. The postoperative wound discomfort is less,left lower lobe atelectesis is less common, and the patient walks sooner.Laparoscopic splenectomy is more difficult when the patient's spleen isvery much enlarged, and some surgeons believe this is a relative contraindicationto MIS.
In cases of splenic trauma, laparoscopy is rarely employed. Large amountsof intraperitoneal blood make it difficult to explore the abdomen for otherinjuries, and the splenic pedicle is more difficult to isolate laparoscopically.6
Surgical treatment for gastroesophageal reflux
One of the unfortunate consequences of our ability to keep severely compromisedinfants and children alive is that we now care for an increasing numberof children who are neurologically impaired and require gastrostomies andantireflux procedures for long-term maintenance in extended care facilities.The antireflux procedures reduce, but do not eliminate, the incidence ofreflux, and many surgeons now perform a fundoplication at the same timeas the gastrostomy. The presence of a ventriculo-peritoneal shunt is nota contraindication to MIS in these cases. It is important to stress thatthe indications for laparoscopic antireflux surgery are identical to thosefor open surgery; only the approach is different. The results so far havebeen excellent, with fewer postoperative respiratory problems and less needfor pain medication.7
Many centers that treat adult patients with gastroesophageal reflux arecontent to do so using the newer motility-enhancing drugs and various H2blockers. This choice essentially condemns the patient to long-term oralmedication with the attendant expenses and side effects. While the Nissenfundoplication (or its various modifications) is not a perfect operation,it has been used throughout the world for many years and has been performedusing MIS for the past five years with good success.
Intestinal obstruction
Exploratory laparoscopy and adhesiolysis for intestinal obstruction hasbeen performed successfully for postoperative adhesions, malrotation, andother indications.8 Intestinal resection and anastomosis hasalso been performed, but most surgeons now do laparoscopically assistedresections in which the bowel to be excised is prepared using MIS but isthen brought out through a small incision. The actual resection and anastomosisis performed extracorporeally, and the bowel then replaced into the peritonalcavity under direct vision. Bleeding Meckel's diverticula have been treatedin the same way, and several reports have also documented the advantagesof MIS in the surgical treatment of Crohn's disease.9
Liver disease, ulcers, and adrenal tumors
The technique of laparoscopically directed liver biopsies based on CTor magnetic resonance imaging (MRI) was one of the first widely accepted"interventional" uses of MIS and is still used today when thesuspected lesion is not readily accessible through a CT scan window.
Perforated duodenal ulcers are no longer as common as they were 20 yearsago, now that Helicobacter pylori has been discovered and successful treatmentsdevised. But they still occur. If a perforated ulcer is found at an exploratorylaparoscopy, an omental patch may be placed over it and medical treatmentinitiated. In many cases, this obviates an open surgical approach.
A new use for MIS that has recently been described and implemented inmany centers is adrenalectomy. This method has been successfully used forboth pheochromocytomas and cortical tumors, although MIS is not recommendedfor obvious malignancies with proven metastases or for tumors greater than5 cm in diameter, which are more likely to be malignant. Three approacheshave been used for laparoscopic adrenalectomy: the posterior, the lateral,and the anterior. Most surgeons now seem to be using the lateral approach.The posterior technique is preferred by some in cases where both adrenalsare to be removed, and the bilateral operation can be completed withoutmoving the patient from the prone position. The difference in the postoperativecourse between the open procedure, which usually requires a large laparotomywith its inherent morbidity, and the MIS procedure has been striking. Patientshave been up and around the day following surgery and discharged one ortwo days thereafter, compared with an average five- to seven-day hospitalstay with the open procedure.10
Hernia repair: Usually not for children
Although laparoscopic hernia repair has gained favor in some adult centers,it is rarely used in infants and children. The laparoscopic approach placesa mesh patch on the peritoneal side of the hernia defect and tacks the meshin place with specially developed staplers. This procedure is appropriatefor some teenage patients with bilateral hernias or when previous inguinaloperations have been unsuccessful.
Another use for MIS in hernia repair has been in patients with a symptomatichernia on one side and a questionable hernia on the other. A small, 30°scope may be placed through the open sac on the symptomatic side and theinternal ring and posterior wall of the contralateral side visualized. Thepresence or absence of a hernia can be established and an unnecessary operationprevented.
Undescended testicle and varicocele
MIS has also been used to explore the retroperitoneum in cases of undescendedtesticle. When the gonad is not palpable in the scrotum or inguinal canal,it may still be present retroperitoneally anywhere between the peritonealaspect of the internal ring and the inferior pole of the kidney. Althoughultrasound examination may be useful in some cases, identification of thetesticle is best done by direct visualization. The size and shape of thetesticle can be ascertained, and if there is any question as to whetherthe gonad is a testicle or ovary, a biopsy can be obtained. Based on theresults of the biopsy, a gonadectomy may be indicated. If the gonad is atesticle and the decision has been made to bring it down into the scrotum,the first stage of a Fowler- Stevens repair (clipping the testicular arteryto allow the artery parallel to the vas and other small accessory vesselsto perfuse the testicle) may be performed using MIS techniques.11
Ligation of the venous plexus for varicocele may also be performed usingMIS. The veins exiting the internal ring may be clipped or ligated underdirect vision and some of the anastomotic branches to the pelvic and abdominal-wallveins can be identified, separated from the arteries, and ligated. MIS iscertainly advantageous in recurrent cases to avoid entering the scar tissueof the previous incision and dissection.
Gynecologic disorders
In the years since the earliest observational laparoscopies, new technologyhas allowed more exact inspection and more accurately directed biopsiesand culture taking.
The treatment of ovarian cysts is an example of the greater flexibilitythat laparoscopic techniques can offer. Ovarian cysts are quite common ininfancy, most of them less than 5 cm in diameter. These small cysts maybe safely watched without intervention, since most will recede and disappear.Ovarian cysts that are larger than 5 cm in diameter can be followed, resected,or biopsied and drained by the use of MIS.
Cysts that appear during adolescence are most frequently follicular cystsand will eventually recede or rupture spontaneously. If they do not, laparoscopicintervention is indicated and the contralateral ovary may be inspected aswell. In older patients some controversy exists over using MIS for excisionor aspiration, since any spillage of malignant tumor cells into the peritonealcavity could significantly change the long-term prognosis in these patients;this is less of a concern with adolescents, since malignancy is so unlikely.
MIS may also be helpful for the diagnosis of ectopic pregnancy when ultrasoundis equivocal or the patient's condition calls for immediate intervention.Definitive treatment may also be accomplished endoscopically. Laparoscopycan also establish a diagnosis of congenital uterine malformation such asuterus didelphia, absent uterine horns, and vaginal atresia. Although thesediagnoses may be suspected on the basis of radiologic data, they are usuallybest substantiated by direct observation through the endoscope. Appropriatesurgical treatment may also be performed using MIS.
In oncologic cases requiring radiation along the course of the majorvessels, fixation of the ovaries in the midline is often recommended toavoid the direct effects of external beam radiation. The oophoropexy issometimes performed at the time of the primary procedure, but it may alsobe accomplished laparoscopically as a second stage.12
AIDS
Lung biopsies are being performed more often, especially in centers wherethe pulmonary complications of HIV infections have been identified withgreater frequency. The diagnosis of Pneumocystis carinii infection is sometimesdifficult to establish without a tissue culture and biopsy. Samples canbe obtained thoracoscopically with less morbidity and pain than by the openmethod. Often a bronchoscopy with washings is performed under the same anesthesia.Excision of lesions identified on CT scan or MRI may be accomplished easily,especially if the masses are close to or on the pleural surfaces.
Thoracic tumors and cysts
Neoplasms of the lung and chest wall may be biopsied or excised thoracoscopically.The new endoscopic stapling instruments and the harmonic scalpel have madesegmental lung resection much easier.
Mediastinal masses may be biopsied or excised thoracoscopically in manycases. Duplication cysts of the esophagus, bronchogenic cysts, and smallsequestrations, too, may be successfully excised using MIS. Pericardialwindows are easily performed thoracoscopically, and this procedure is arecent addition to the list of procedures that may be safely performed byMIS. Hyperhydrosis has been effectively treated by ablation of the uppersympathetic ganglia at the apex of the pleural cavity.13 In caseswhere vagotomy is indicated, the vagus nerves can usually be identifiedalong the lower esophageal wall and truncal vagotomy accomplished withoutresorting to open thoracotomy. Decortication and release of trapped lungsas well as drainage of loculated pleural effusions with precise placementof thoracostomy tubes for maximum efficiency can also be done without amajor thoracotomy incision. In achalasia patients, Heller procedures thatrelieve the stricture by dividing the esophageal musculature can be performedlaparoscopically.
MIS has also expanded into the field of spine surgery as increasing numbersof centers are using this technique for diskectomy. Thoracoscopy is usedto remove thoracic disks in scoliosis, and laparoscopy for diskectomy incases of lumbar scoliosis and lower back pain.14
What the future may hold
The scope of MIS in the care of pediatric patients is sure to expandas more surgeons are trained to perform more varied and complicated proceduressafely. These advances can only encourage more patients and pediatriciansto seek the benefits of modern technology and innovation in providing bettercare. In every case, pediatric surgeons and pediatricians will continueto weigh the safety, effectiveness, and costs of the new procedures againstthe proven record of conventional approaches.
REFERENCES
1. Kleinhaus S, Kaleya R, Canning R, et al: Laparoscopic cholecystectomyin teenagers. J Adol Health 1992;13:693
2. Deziel DJ, Millikan KW, Economou SG, et al: Complications of laparoscopiccholecystectomy: A nationalsurvey of 4,292 hospitals and an analysis of77,604 cases.Amer J Surg 1993;165:9
3. Hermans B-Ph, Otte JB: Laparoscopic appendectomy: Pros and cons; Literaturereview of 4,190 cases. Acta Chir Belg 1997;97:110
4. Kleinhaus S, Hein K, Sheran M, et al: Laparoscopy for diagnosis andtreatment of abdominal pain in adolescent girls. Arch Surg 1977;112:1178
5. Rogers J, Yousuf A, Kleinhaus S: Laparoscopic accessory splenectomyin recurrent chronic immune thrombocytopenic purpura. Surg Laparosc Endosc1997;7:83
6. Glasgow RE, Yee LF, Mulvihill SJ: Laparoscopic splenectomy: The emergingstandard. Surg Endosc 1997;11:108
7. Rothenberg SS: Experience with 220 consecutive laparoscopic Nissenfundoplications in infants and children.J Ped Surg 1998;33:274
8. Kleinhaus S: Laparoscopic lysis of adhesions for postappendectomypain. Gastrointestinal Endosc 1985;30:304
9. Ludwig KA, Milsom JW, Church JM, et al: Preliminary experience withlaparoscopic intestinal surgery for Crohn's Disease. Am J Surg 1996;171:52
10. Rutherford JC, Stowasser M, Tunny TJ, et al: Laparoscopic adrenalectomy.World J Surg 1996;20:758
11. Seibold J, Janetschek G, Bartsch G: Laparoscopic surgery in pediatricurology. Eur Urol 1996;30:394
12. Nagel TC, Sebastian J, Malo JW: Oophoropexy to prevent sequestrialor recurrent torsion. J Amer Assoc Gyn Laparosc 1997;4:495
13. Cohen Z, Shinhar D, Kurzbart E, et al: Laparoscopic and thoracoscopicsurgery in children and adolescents: A 3-year experience. Pediatr Surg Int1997;12:356
14. Olsen D, McCord D, Law M: Laparoscopic discectomy with anterior interbodyfusion of L5-S1. Surg Endosc 1996;10:1158
By Sylvain Kleinhaus, MD, and Scott J. Boley, MD.
DR. KLEINHAUS is Professor of Surgery and Pediatrics, Albert Einstein College of Medicine,Montefiore Medical Center, Bronx, NY.
DR. BOLEY is Professor of Surgery and Pediatrics, Albert Einstein College of Medicine, Montefiore MedicalCenter, Bronx, NY.
The latest news about minimally invasive surgery. Contemporary Pediatrics 1999;0:125.
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.