Lead poisoning: What’s new about an old problem?
The reduction of blood lead levels (BLLs) in children in the United States over the past 4 decades is a great public health success. There are, however, groups of children who are at higher risk for lead exposure.
Over 4 million children in the United States are still at risk of exposure to lead.1 Now prevention of childhood lead poisoning must move to the forefront, and pediatricians need to provide anticipatory guidance as well as appropriate interventions to minimize and manage risks of lead exposure to their patients.
The reduction of blood lead levels (BLLs) in children in the United States over the past 4 decades is a great public health success. There are, however, groups of children who are at higher risk for lead exposure. Pediatricians need the tools to identify these high-risk children and provide primary prevention and lead testing, as well as respond appropriately to lead testing results.
More from this issue: Prediabetes or T2D?
Although pediatricians report good familiarity regarding the management of lead exposure in children, approximately 40% of calls to the Pediatric Environmental Health Specialty Unit (PEHSU) network are regarding lead exposure.2 Over the past few years, even the definition of what constitutes a significant exposure has changed as the Centers for Disease Control and Prevention (CDC) has updated its guidance to emphasize that clinicians should counsel on exposure prevention and perform surveillance for lead exposure.3
This article aims to translate the research regarding lead exposure in children into a practical form that pediatricians can use in their offices and clinics. As the effects of lead on the developing brain are not reversible, our secondary purpose is to stress the importance of pediatricians providing counseling on primary prevention of lead exposure in their patients.
Background
Lead is a malleable, corrosion-resistant metal used by humans since at least 3500 BCE. In the ensuing millennia, atmospheric lead levels have increased a million times over those in prehistoric times. Lead has long been known to be hazardous, with early physicians and scientists describing various symptoms of lead poisoning in adults, one of the earliest being the Greek physician Nicander in the 2nd century BCE.4
Lead toxicity in children was first described by Dr. John Lockhart Gibson in 1892 when he reported children with severe neurologic disease that was associated with exposure to deteriorating white lead paint.4,5 Although the toxic effects of lead were well known for millennia, sale of lead-based residential paint was not banned in the United States until 1978.5,6 Additionally, the sale and use of leaded gasoline nationally in automobiles was gradually phased out over 25 years until its complete elimination in 1996.7
NEXT: The health effects of lead
Epidemiology
There has been a greater than 90% drop in BLLs for children aged 1 to 5 years in the United States over the past 40 years. The geometric mean (GM) BLL for children aged 1 to 5 years in the 1976-1980 National Health and Nutrition Examination Survey (NHANES) was 15 µg/dL, whereas in the most recent NHANES (2007-2010), the GM BLL was 1.3 µg/dL.8 This decrease in childhood BLLs, combined with evidence suggesting that there is no “safe” level for lead, prompted the CDC to create a “reference level” for children aged 1 to 5 years. This value is 5 µg/dL and is based on the 97.5th percentile BLL in the NHANES sample.3,9
The CDC estimates that 2.6% of US children aged 1 to 5 years have a BLL greater than 5 µg/dL, translating to an estimated 535,000 children based on the 2010 US census.8 Certain demographic subpopulations are associated with having higher BLLs. Nonwhite children or children of lower family income are at higher risk.8,10 In particular, children living in housing built prior to 1978 or those living closer to point sources of lead contamination (such as smelting or battery recycling operations) tend to have more lead exposure and higher BLLs. There are approximately 24 million US housing units with deteriorating lead paint that contain lead-contaminated house dust.11 Demolition of this older housing also has been associated with increases in ambient lead dust contributing to elevated BLLs in children living near the demolition.12,13
Read more: Mobile health clinic to the rescue
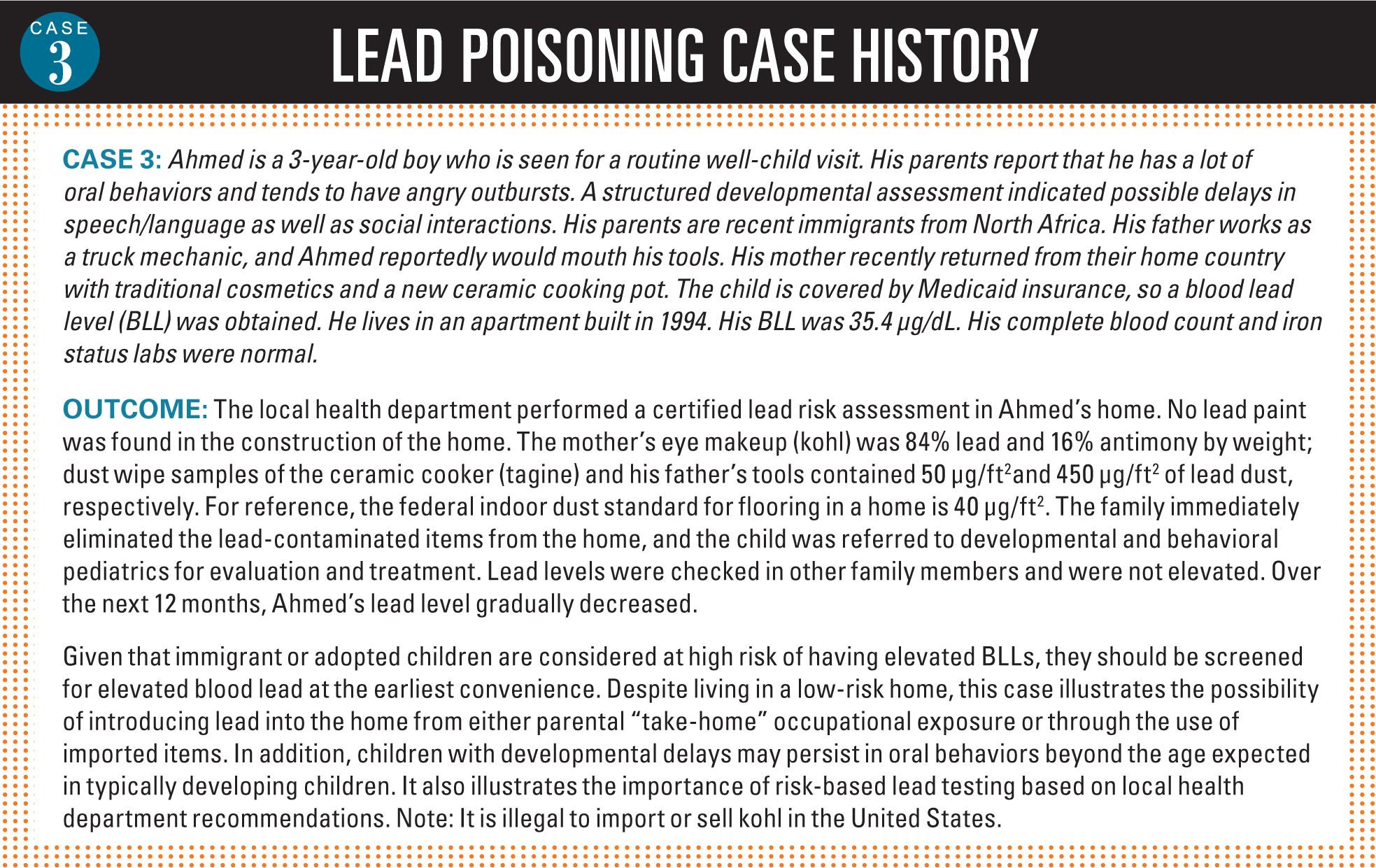
Children’s BLLs tend to peak at approximately 2 years of age, then decrease in most children as a result of normal development leading to the extinguishing of oral behaviors.13 Children with developmental delays in whom there is persistent hand-to-mouth behavior have longer periods during which they are at risk of lead poisoning.14

Health effects of lead exposure
The inhalation, ingestion, or absorption of lead resulting in an elevated blood level of lead is known as lead poisoning. Lead is known to have a myriad of acute and chronic effects including loss of appetite, constipation, abdominal colic, decreased IQ, behavioral problems (inattentive, hyperactive, or disorganized behaviors), hearing and balance problems, encephalopathy, anemia, growth retardation, delayed sexual maturation, increased dental caries, cardiovascular disease, renal disease, convulsions, coma, and death.5,6,14,16,17
Rarely do children have acutely symptomatic lead poisoning compared with previous decades. This is because of the overall reduction in average BLL since the commercial use of lead in paint and gasoline was banned. Studies have shown that lead is neurotoxic at low BLLs, with harmful effects detectable even at levels of 2 µg/dL.18-20 A recent study showed an adverse effect on children’s academic performance at school in those with a history of BLLs below 5 µg/dL in early childhood.21
Unfortunately, there are no effective treatments to reverse the neurodevelopmental effects of lead poisoning. This necessitates a shift of emphasis for medical providers from only screening to detect asymptomatic lead poisoning to providing anticipatory guidance on the primary prevention.
NEXT: Common sources for lead poisoning
Sources and routes of lead exposure
Most lead exposure in US children occurs as a result of ingesting lead paint dust in older homes and buildings that contain deteriorating lead paint.15 Prior to 1950, the average lead content in paint was 50% lead by dry weight. It can be released during sanding or stripping lead-based paint while renovating, repairing, or painting a structure built prior to 1978. Despite these risk factors, more than 30% of children with elevated BLLs were not exposed by way of lead-based paint.22
More: Funding extended for prenatal cocaine exposure study
Lead-contaminated soil is another common source of lead exposure in children. Soil can be contaminated by deteriorating lead-based paints on the exterior of buildings, lead dusts from deposition of leaded gasoline vapor, or from industrial activities. Because it tends to bind to organic compounds in the soil, lead stays in the upper soil layers and therefore remains a source of exposure.22
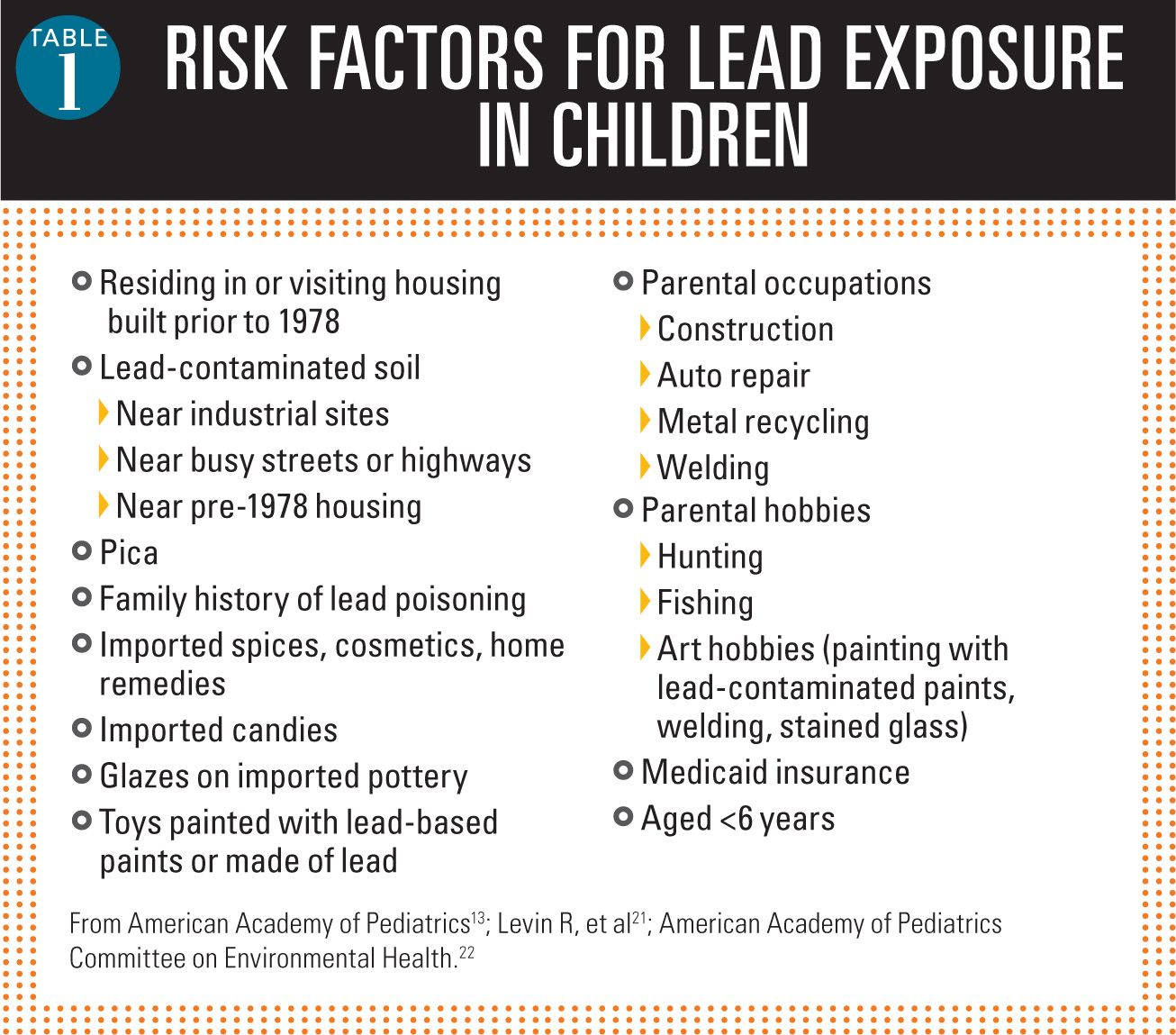
In addition, children can be exposed to lead as a result of an occupational “take-home” exposure from an adult who works in a lead-contaminated environment (eg, battery or metal recycling plant; welding jobs; auto/truck repair; demolition or construction work; bridge painting). Other sources of lead exposure in children that have made headlines in the popular media include toys painted with lead-based paints; ceramic glazes; folk remedies; imported spices; cosmetics; adult occupations or hobbies involving metal (soldering, welding, fishing, hunting); or from water that has traveled through older lead pipes or pipes soldered with lead. See Table 1 for risk factors for lead exposure in children.14,22,23
Young children become exposed to the lead dust or paint chips when they crawl on the floor and engage in normal hand-to-mouth behaviors, which are highly prevalent between ages 9 and 24 months. Although there are certainly concerns regarding homes with chipping paint, many children are exposed to lead through the dust that comes off of friction surfaces (doors, door frames, windows, window frames) painted with lead-based paint. A very small amount of dust (40 µg/ft2) distributed around the floor of a home may significantly raise a child’s lead level. Other behaviors include pica (eating nonfood items such as rocks, dirt, or paper) or chewing on lead-based paint on windowsills or interior woodwork.14,22,23
Evaluation
Obtaining a BLL makes the diagnosis of lead poisoning. Venous BLLs are preferred as these more accurately reflect lead exposures.15 Screening for elevated lead is possible using capillary blood samples, but environmental lead contamination on the skin can lead to false positives.14 Any elevated capillary BLL level needs confirmation with a venous sample. Hair and urine lead-level determinations should not be performed.15
Noninvasive lead screening tests are not available outside a research setting, and determination of the total body lead burden is not feasible.15 The half-life of lead in the bloodstream is about 35 days; however, circulating levels of lead in blood reflect not only recent exposure but also ongoing mobilization of lead from soft tissues and long-term physiologic depots such as bone.24 Provoked urine testing for heavy metals following administration of a chelating agent such as succimer is not recommended.25
Following recommendations of the CDC, state and local health departments have developed screening plans to identify children at high risk for lead exposure.26 In general, those at high risk include: children from households below the federal poverty level; non-Hispanic blacks; Mexican Americans; children living in areas with a known high prevalence of lead poisoning or older housing; immigrants; refugees; and recent international adoptees.9,17 Certain states require Medicaid-enrolled children to be screened at 1 and 2 years of age.16,17 Children aged between 36 and 72 months who missed recommended screening should also be screened.14 Immigrants, refugees, and internationally adopted children should be screened at the earliest opportunity and again in 3 to 6 months. In jurisdictions where there is no high-risk screening plan, universal screening at ages 12 and 24 months is recommended.26
It is important to obtain an environmental exposure history to attempt to find the source of the exposure so that it may be eliminated. Children should be assessed for iron deficiency anemia because iron deficiency increases gastrointestinal (GI) tract absorption of lead. Iron deficiency and other micronutrient deficiencies are associated with pica behaviors.15,16 Ensuring an adequate intake of iron, calcium, and vitamin C may help to minimize lead absorption.9 Other children in the home also may be exposed to lead and should be tested. Finally, referrals to the local health department or to a PEHSU should be carried out as appropriate (see “Resources for physicians and clinicians, page 15).
NEXT: What's your role in treatment?
Actions for specific lead levels
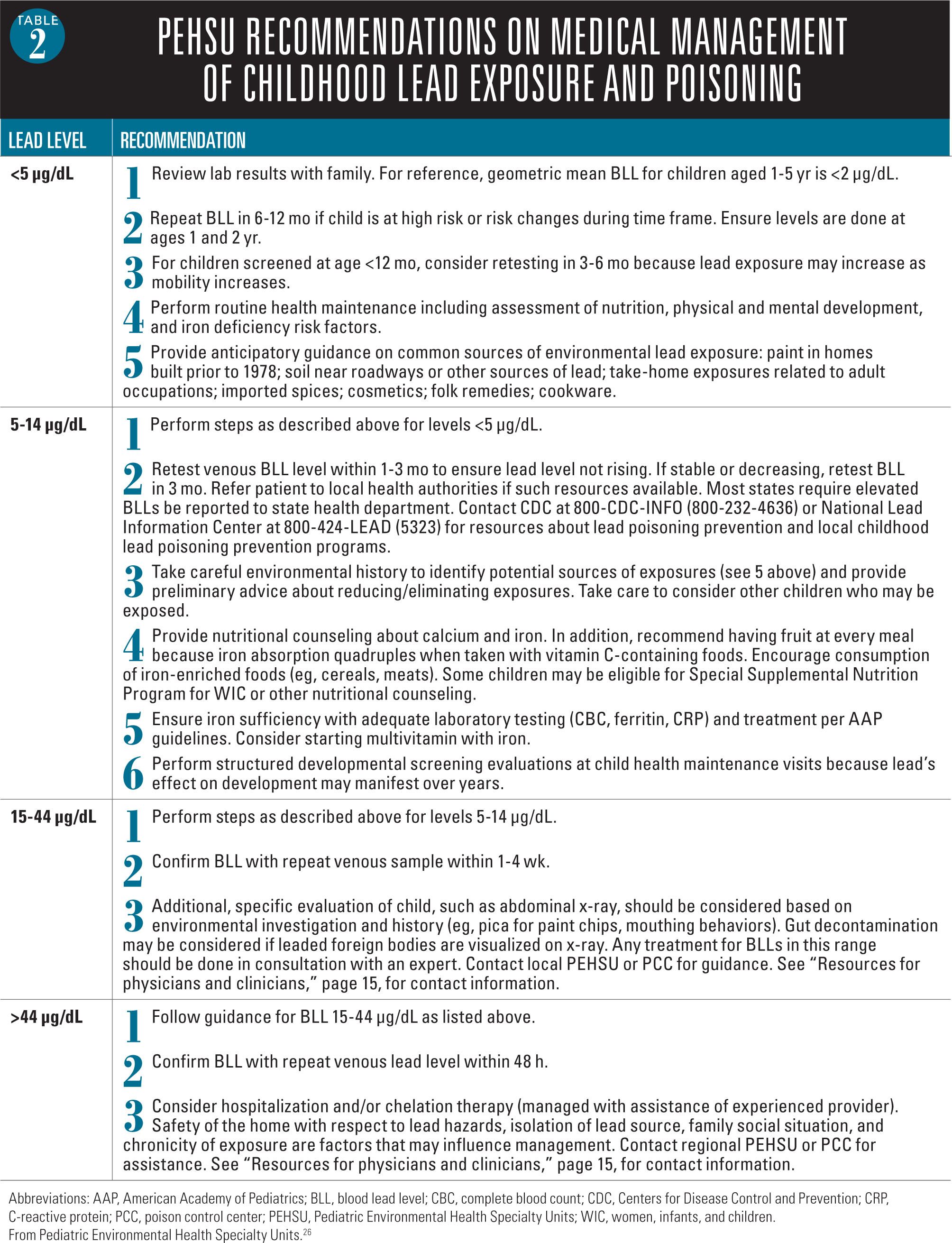
The PEHSU program, with endorsement by the American Academy of Pediatrics (AAP), developed recommendations for the management of elevated lead levels according to the level of blood lead (Table 2).27 An environmental history should be obtained to help identify possible sources of lead exposure. In general, for a BLL <5 µg/dL, the level should be repeated in 6 to 12 months if the child remains at an increased risk of lead poisoning or if a child’s risk level changes. If the child is aged younger than 12 months, consideration to retest in 3 to 6 months should be given because lead exposure tends to increase as the child’s mobility increases. If a child is found to have a BLL between 5 µg/dL and 14 µg/dL, the BLL should be retested in 1 to 3 months to ensure that the lead level is not rising. A BLL between 15 µg/dL and 44 µg/dL should be confirmed within 1 to 4 weeks. For BLLs in excess of 44 µg/dL, a repeat lead level should be obtained within 48 hours. Patients with BLLs that are 5 µg/dL or more should be referred to the local health department for possible case management.
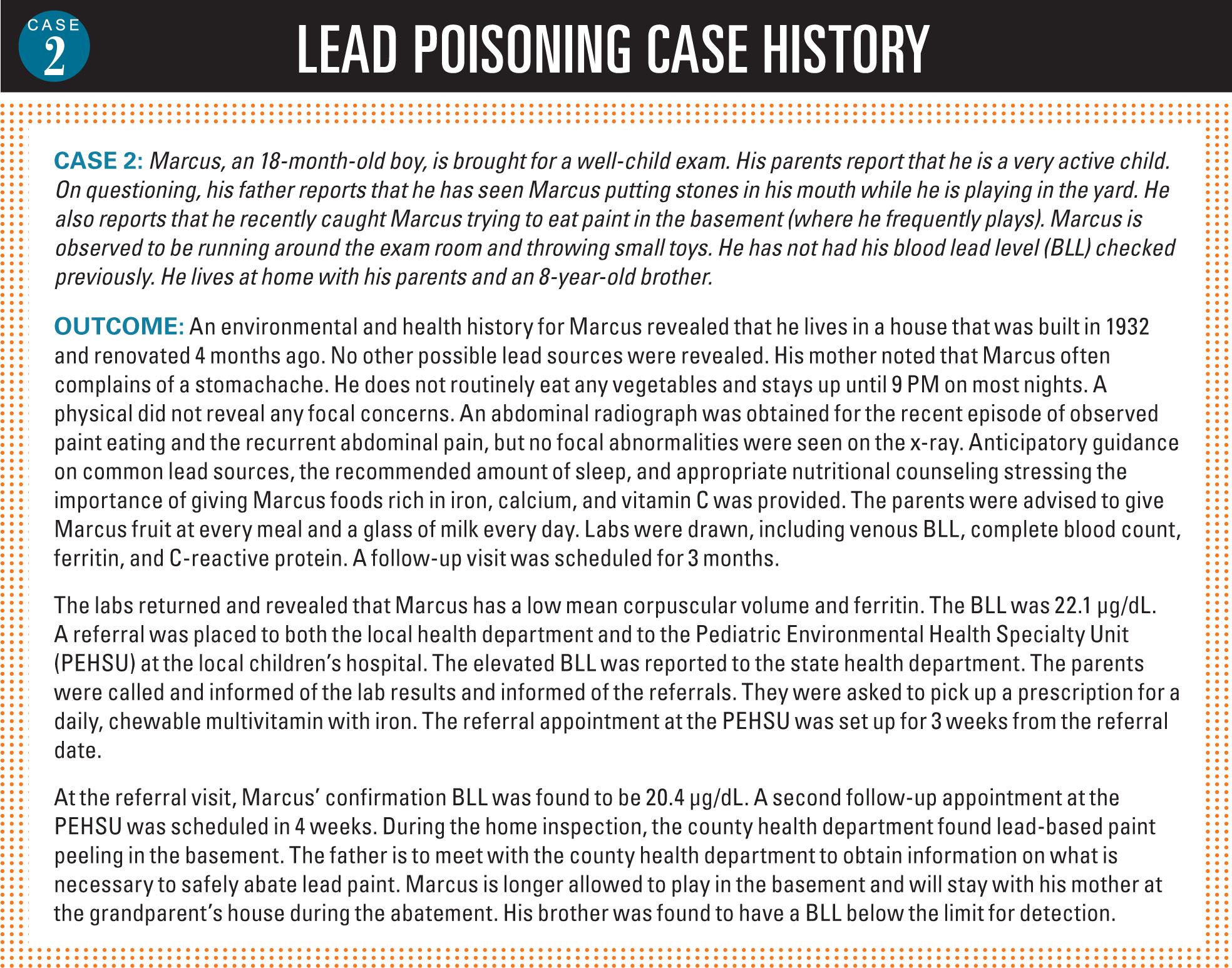
Many states require that elevated BLLs be reported to the state health department. However, because funding of state childhood lead poisoning and prevention programs has decreased, home assessments may not be performed. Thus, case management and education should occur within the physician’s office.
More: Schools providing water, but kids don't drink
Additional evaluations, such as performing an abdominal radiograph, should be considered based on the history. Evidence is lacking to recommend either gastric lavage or whole bowel irrigation to clear lead chips from the GI tract.28 Hospitalization and/or chelation therapy should be considered in consultation with an experienced provider and must be carried out in a lead-free environment.
Children with BLLs greater than 45 µg/dL should be moved to a lead-safe environment as soon as possible so that chelation therapy can begin. In children without encephalopathy, and lead levels between 45 µg/dL and 70 µg/dL, meso-2,3-dimercaptosuccinic acid (DMSA, succimer) is recommended.23 The most common adverse effects of succimer are neutropenia, elevated transaminases, rash, and abdominal pain. Although succimer will decrease lead levels in children with BLLs below 45 µg/dL, a randomized, controlled trial did not demonstrate neurocognitive or neurobehavioral benefit and therefore it is not recommended for use in these children.29
For children with encephalopathy or lead levels greater than 70 µg/dL, inpatient chelation therapy with the combination of dimercaprol (British anti-Lewisite [BAL]) and CaNa2EDTA is recommended.23 However, because of small muscle mass in children, use of peanut oil as a diluent, and the need for dosing every 4 hours, BAL may not be an option. As succimer is an oral congener of BAL, it may be substituted for BAL. Chelation therapy should be carried out with the guidance of an experienced practitioner including those at the regional PEHSU or Poison Control Center.
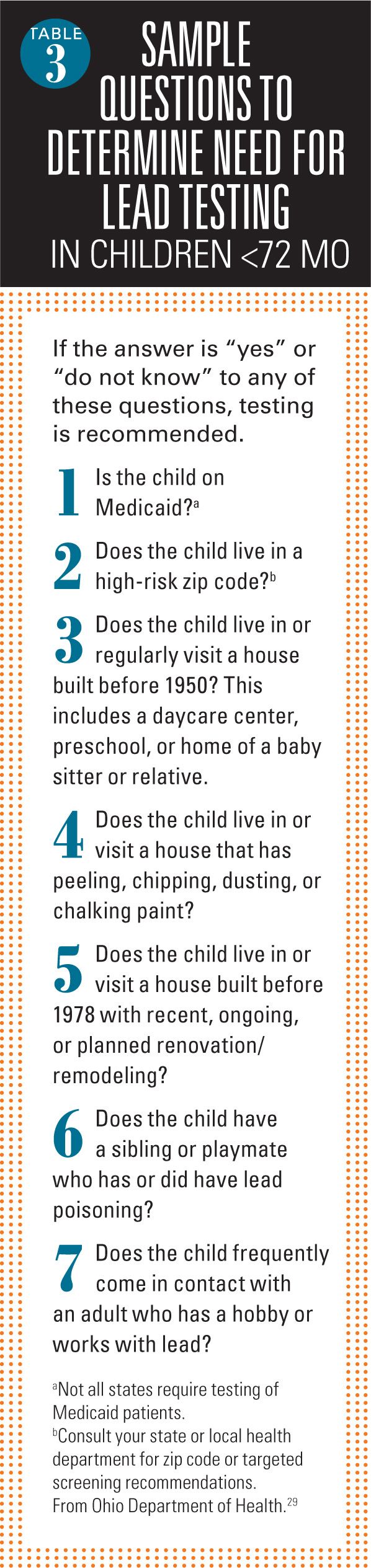
Role of the pediatrician in prevention
Clinicians play an important role in the prevention of lead exposure. This job can be broken down into several manageable tasks. The first is to ask essential screening questions (Table 3).30 Other tasks include conducting outreach and education to minimize exposures; emphasizing healthy nutrition and/or dietary supplements to prevent lead absorption; performing lead testing (to identify children for whom primary prevention efforts have failed); and performing appropriate clinical interventions for children with elevated BLLs, including ongoing monitoring and coordinating with local health departments to minimize risks to children from lead exposure.9
Clinicians also should be familiar with the specific anticipatory guidance that is helpful in preventing lead exposure, which fortunately overlaps with other anticipatory guidance that is being delivered during routine office visits. Encouraging an adequate intake of calcium (2 to 3 8-oz cups of milk or equivalent/day), vitamin C (5 fruits or vegetables/day), and iron (either through iron-rich foods or supplementation per AAP guidelines) should be discussed at well-child care appointments.
In addition, clinicians should inquire about the age and conditions of the home during well-child visits and introduce families to local resources (usually the local health department) that may help families address lead hazards before their child is exposed. Because many children (and adults) are exposed to lead during painting and renovation of older homes, families should be encouraged to seek advice from both governmental sources and from their local home centers on how to safely renovate an older home.
NEXT: Conclusion
Conclusion
Childhood lead poisoning remains a serious problem in the United States, even though average blood lead levels are significantly lower than those in the middle-to-late 20th century. Evidence of irreversible damage to a child’s developing brain resulting in both psychologic pathology and cognitive deficits can occur at lead levels much lower than previously believed. As a result of these new findings, the PEHSUs, with endorsement by the AAP, developed updated recommendations on the screening and management of lead poisoning.
Because evidence suggests that the effects of an elevated BLL on intelligence and behavior are irreversible, emphasis should be placed on providing anticipatory guidance to prevent lead exposure. Simply testing for lead is no longer acceptable. Primary prevention must move to the forefront. As funding for childhood lead poisoning prevention programs within health departments declines, physicians will be required to provide appropriate measures for diagnosis and management of their patients.
Next: Wet wraps relieve eczema in kids
Acknowledgment: The US Environmental Protection Agency (EPA) supports the Pediatric Environmental Health Specialty Unit (PEHSU) by providing funds to the Agency for Toxic Substances and Disease Registry (ATSDR) under Inter-Agency Agreement no. DW-75-92301301-0. Neither the EPA nor the ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications.
REFERENCES
1. Centers for Disease Control and Prevention. Lead. http://cdc.gov/nceh/lead/default.htm. Updated Febraury 9, 2015. Accessed March 24, 2015.
2. Trasande L, Newman N, Long L, et al. Translating knowledge about environmental health to practitioners: are we doing enough? Mt Sinai J Med. 2010;77(1):114-123.
3. Centers for Disease Control and Prevention. CDC response to Advisory Committee on Childhood Lead Poisoning Prevention Recommendations in “Low Level Lead Exposure Harms Children: A Renewed Call of Primary Prevention.” Available at: http://www.cdc.gov/nceh/lead/ACCLPP/CDC_Response_Lead_Exposure_Recs.pdf. Modified June 7, 2012. Accessed March 13, 2015.
4. Needleman H. Low level lead exposure: history and discovery. Ann Epidemiol. 2009;19(4):235-238.
5. Rabin R. Warnings unheeded: a history of child lead poisoning. Am J Public Health. 1989;79(12):1668-1674.
6. Lanphear BP. Childhood lead poisoning prevention: too little, too late. JAMA. 2005;293(18):2274-2276.
7. Needleman HL. The removal of lead from gasoline: historical and personal reflections. Environ Res. 2000;84(1):20-35.
8. Centers for Disease Control and Prevention (CDC). Blood lead levels in children aged 1-5 years-United States, 1999-2010. MMWR Morb Mortal Wkly Rep. 2013;62(13):245-248.
9. Advisory Committee on Childhood Lead Poisoning Prevention. Low level lead exposure harms children: a renewed call for primary prevention.. Available at: http://www.cdc.gov/nceh/lead/ACCLPP/Final_Document_030712.pdf. Published January 4, 2012. Accessed March 13, 2015.
10. Lowry JA, Paulson JA. Recommendations updated for managing lead exposure in children. AAP News. 2013;34(12):23.
11. National Center for Environmental Health, Centers for Disease Control and Prevention. Lead. Prevention tips. Available at: http://www.cdc.gov/nceh/lead/tips.htm. Updated June 19, 2014. Accessed March 13, 2015.
12. Farfel MR, Orlova AO, Lees PS, Rohde C, Ashley PJ, Julian Chisolm J Jr. A study of urban housing demolition as a source of lead in ambient dust on sidewalks, streets, and alleys. Environ Res. 2005;99(2):204-213.
13. Rabito FA, Iqbal S, Shorter CF, et al. The association between demolition activity and children’s blood lead levels. Environ Res. 2007;103(3):345-351.
14. American Academy of Pediatrics, Council on Environmental Health. Lead. In: Etzel RA, Balk SJ, eds. Pediatric Environmental Health. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2012:439-449.
15. Abelsohn AR, Sanborn M. Lead and children: clinical management for family physicians. Can Fam Physician. 2010;56(6):531-535.
16. Schnur J, John RM. Childhood lead poisoning and the new Centers for Disease Control and Prevention guidelines for lead exposure. J Am Assoc Nurse Pract. 2014;26(5):238-247.
17. Warniment C, Tsang K, Galazka SS. Lead poisoning in children. Am Fam Physician. 2010;81(6):751-757.
18. Canfield RL, Henderson CR Jr, Cory-Slechta DA, Cox C, Jusko TA, Lanphear BP. Intellectual impairment in children with blood lead concentrations below 10 microg per deciliter. N Engl J Med. 2003;348(16):1517-1526.
19. Jusko TA, Henderson CR, Lanphear BP, Cory-Slechta DA, Parsons PJ, Canfield RL. Blood lead concentrations <10 microg/dL and child intelligence at 6 years of age. Environ Health Perspect. 2008;116(2):243-248.
20. Lanphear BP, Hornung R, Khoury J, et al. Low-level environmental lead exposure and children’s intellectual function: an international pooled analysis. Environ Health Perspect. 2005;113(7):894-899.
21. Zhang N, Baker HW, Tufts M, Raymond RE, Salihu H, Elliott MR. Early childhood lead exposure and academic achievement: evidence from Detroit public schools, 2008-2010. Am J Public Health. 2013;103(3):e72-e77.
22. Levin R, Brown MJ, Kashtock ME, et al. Lead exposures in U.S. children, 2008: implications for prevention. Environ Health Perspect. 2008;116(10):1285-1293.
23. American Academy of Pediatrics Committee on Environmental Health. Lead exposure in children: prevention, detection, and management. Pediatrics. 2005;116(4):1036-1046.
24. Rabinowitz MB. Toxicokinetics of bone lead. Environ Health Perspect. 1991;91:33-37.
25. American College of Medical Toxicology. American College of Medical Toxicology position statement on post-chelator challenge urinary metal testing. J Med Toxicol. 2010;6(1):74-75.
26. Wengrovitz AM, Brown MJ; Advisory Committee on Childhood Lead Poisoning, Division of Environmental and Emergency Health Services, National Center for Environmental Health; Centers for Disease Control and Prevention. Recommendations for blood lead screening of Medicaid-eligible children aged 1-5 years: an updated approach to targeting a group at high risk. MMWR Recomm Rep. 2009;58(RR-9):1-11.
27. Pediatric Environmental Health Specialty Units. Recommendations on medical management of childhood lead exposure and poisoning. Available at: http://www.pehsu.net/documents/medical-mgmnt-childhood-lead-exposure-June-2013.pdf. Updated June 2013. Accessed March 13, 2015.
28. Dapul H, Laraque D. Lead poisoning in children. Adv Pediatr. 2014;61(1):313-333.
29. Rogan WJ, Dietrich KN, Ware JH, et al; Treatment of Lead-Exposed Children Trial Group. The effect of chelation therapy with succimer on neuropsychological development in children exposed to lead. N Engl J Med. 2001;344(19):1421-1426.
30. Ohio Department of Health. Blood lead testing requirements for Ohio children less than 6 years of age. Available at: http://www.odh.ohio.gov/~/media/ODH/ASSETS/Files/cfhs/lead%20poisoning%20-%20children/2014/Updated%20Brochures-Forms/BloodLeadTestingRequirementsandZipCodes.ashx. Revised January 2015. Accessed March 13, 2015.
Resources for physicians and clinicians
US Environmental Protection Agency lead information page:
Centers for Disease Control and Prevention (CDC) webpage for lead poisoning:
CDC webpage on lead testing in immigrant and refugee populations: http://www.cdc.gov/immigrantrefugeehealth/guidelines/lead-guidelines.html
US Department of Housing and Urban Development page on lead-based paint: http://portal.hud.gov/hudportal/HUD?src=/program_offices/healthy_homes/healthyhomes/lead
Legal Services Corporation’s list of local legal aid organizations that can help families with housing and landlord problems:
http://www.lsc.gov/find-legal-aid
Pediatric Environmental Health Specialty Units website:
Dr Bennett, a former occupational/environmental medicine resident at the University of Cincinnati, Ohio, is a pharmacovigilance physician with Advanced Clinical at Otsuka Pharmaceutical Co Ltd. Dr Lowry is chief of clinical toxicology, Children’s Mercy Hospital and Clinics, Kansas City, Missouri, and director, Mid-America Pediatric Environmental Health Specialty Unit. Dr Newman is director of the EnvironmentalHealth and Lead Clinic, Cincinnati Children’s Hospital Medical Center, and director of the Region 5 Pediatric Environmental Health Specialty Unit Satellite, Cincinnati.
Drs Lowry and Newman were supported by the Association of Occupational and Environmental Clinics (AOEC) and funded (in part) by the cooperative agreement award number 1U61TS000118-03 from the Agency for Toxic Substances and Disease Registry (ATSDR). Drs Bennett and Newman were supported by the National Institute for Occupational Safety and Health (NIOSH) Education and Research Center grant T42-OH008432. Dr Newman received additional funding from the Center for Environmental Genetics NIH/NIEHS P30-ES006096.