Localized Scleroderma
Scleroderma may present at any age and can be localized or systemic. Localized scleroderma affects the skin, subcutaneous fascia, and occasionally muscle and bone. Systemic scleroderma is characterized by chronic disease with both skin changes and visceral abnormalities. Rarely, localized scleroderma may progress to systemic disease; however, screening for this form is unnecessary in patients who have no systemic symptoms.1-5

Figure
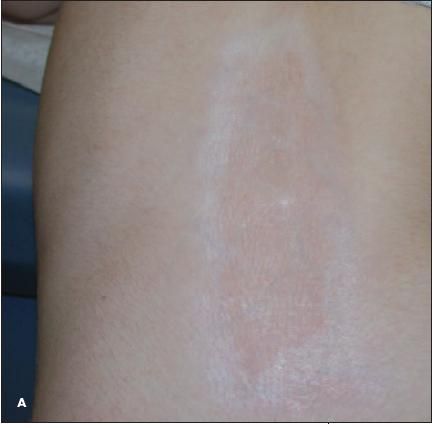
FigureA 13-year-old developmentally delayed girl was brought for evaluation of fibrotic plaques with overlying atrophy and surrounding hyperpigmentation on the middle back (A), lower right breast (B), and upper arms and thighs. The lesions had appeared 6 to 8 months earlier as purplish patches that "hurt a little." They subsequently progressed to firm, white lesions with an outer rim of violaceous discoloration. Results of a skin biopsy confirmed the clinical diagnosis of localized scleroderma.
Scleroderma may present at any age and can be localized or systemic. Localized scleroderma affects the skin, subcutaneous fascia, and occasionally muscle and bone. Systemic scleroderma is characterized by chronic disease with both skin changes and visceral abnormalities. Rarely, localized scleroderma may progress to systemic disease; however, screening for this form is unnecessary in patients who have no systemic symptoms.1-5
Localized scleroderma primarily affects children and young adults. The incidence is 0.4 to 1 per 100,000 persons; the female-to-male ratio is 2:1 to 3:1. In children, the localized form occurs at least 10 times more often than the systemic form.
Localized scleroderma is subdivided into 2 types:
- Morphea (plaque-type, generalized, guttate, and profunda).
- Linear scleroderma (en coup de sabre and Parry-Romberg syndrome).
This patient had plaque-type morphea. Plaque-type morphea occurs in 36% to 48% of affected children.6
Sclerodermiform dermatitis has no definitive cause; it is associated with certain drugs and toxic agents and possibly skin trauma. Some reports have suggested that Borrelia burgdorferi plays a role in the pathogenesis of morphea; however, treating morphea with the antibiotic therapy used for Lyme disease has not proved beneficial,4 and serological and polymerase chain reaction testing have failed to confirm the presence of B burgdorferi in affected patients.7 No immunological markers are clearly associated with morphea; however, elevated serum concentrations of transforming growth factor ?1 were found in patients with all subtypes of localized scleroderma irrespective of clinical disease activity.8
Plaque-like morphea usually begins with erythematous or purplish patches that evolve over weeks to months into firm, hyperpigmented or ivory plaques.6 The rash most commonly affects the trunk, neck, and extremities but may also involve the face. Superficial facial involvement is termed en coup de sabre, whereas progressive atrophy of one side of the face is known as Parry-Romberg syndrome. Associations between facial scleroderma and neurological symptoms (including headache, trigeminal neuralgia, myopathy of external eye muscles, and seizure) have been reported.2,6
Treatment of localized scleroderma is determined by the severity and duration of the lesions. Potent topical or injectable corticosteroids, while somewhat effective, are generally not recommended because they may contribute to local atrophy. Topical calcipotriene ointment has been shown to halt the progression of morphea and linear scleroderma when used early in the disease course, especially when used twice daily under occlusion. 7 For more extensive and disabling lesions, systemic therapy with methotrexate, corticosteroids, oral calci-triol, D-penicillamine, cyclosporine, interferon, or UV light may be required. For lesions overlying a joint (which pose a risk of contractures), physiotherapy, warm baths, massage, and exercise may be helpful. Surgical reconstruction may be needed for deforming lesions, after the active disease phase has abated and the child's growth is complete.1-5
This child was treated with calcipotriene cream but was lost to follow-up.
References:
- Bono W, Dupin N. Localized scleroderma (morphea) [in French]. Presse Med. 2006;35(12, pt 2):1923-1928.
- Ruiz-Sandoval JL, Romero-Vargas S, Gutierrez-Aceves GA, et al. Linear scleroderma en coup de sabre: neurological symptoms, images and review [in Spanish]. Rev Neurol. 2005;41:534-537.
- Al-Khenaizan S, Al-Watban L. Parry-Romberg syndrome. Overlap with linear morphea. Saudi Med J. 2005;26:317-319.
- Rosenwasser TA, Eizen AZ. Scleroderma. In: Fitzpatrick, Eizen AZ, Wolff K, eds. Fitzpatrick's Dermatology in General Medicine. New York: McGraw-Hill; 2003: 2156-2159.
- Black CM, Stephens CO. Systemic sclerosis (scleroderma) and related disorders. In: Maddison PJ, Isenberg DA, Woo P, et al, eds. Oxford Textbook of Rheumatology. Oxford, UK: Oxford Medical Publications; 1993:771.
- Paller AS, Mancini AJ, eds. Hurwitz Clinical Pediatric Dermatology: A Textbook of Skin Disorders in Childhood and Adolescence. 3rd ed. Philadelphia: Elsevier Saunders; 2006:595-599.
- Weide B, Schittek B, Klyscz T, et al. Morphoea is neither associated with features of Borrelia burgdorferi infection, nor is this agent detectable in lesional skin by polymerase chain reaction. Br J Dermatol. 2000;143:780-785.
- Uziel Y, Feldman BM, Krafchik BR, et al. Increased serum levels of TGFbeta1 in children with localized scleroderma. Pediatr Rheumatol Online J. 2007;5:22.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.