Making a difference Point of care screening for hyperlipidemia
Many pediatricians find point-of-care (POC) office lab tests advantageous because these avoid callbacks and allow pediatricians to direct care at the time of the office visit. It has been my experience that when parents are called with a lab result, there is an opportunity for ineffective or even failed communication.
Many pediatricians find point-of-care (POC) office lab tests advantageous because these avoid callbacks and allow pediatricians to direct care at the time of the office visit. It has been my experience that when parents are called with a lab result, there is an opportunity for ineffective or even failed communication.
A POC lipid screen is a perfect example of something that’s easily done, and the results can be discussed with parents immediately face to face rather than waiting for lab results to come in, trying to communicate those results with parents, and taking the chance that parents may not follow up as advised. Here we discuss the latest recommendations regarding lipid screening in children and the POC devices that can facilitate office-based lipid testing.
Hyperlipidemia in children
Atherosclerotic changes in blood vessels begin in childhood, long before they produce symptoms decades later. Postmortem autopsies of children and adolescents who died accidentally have shown a correlation between elevated lipid levels and early atherosclerotic lesions.1,2 In 2010, the Centers for Disease Control and Prevention analyzed results from the National Health and Nutrition Examination Survey for 1999-2006 and found that the prevalence of abnormal lipid levels among children aged 12 to 19 years was an astounding 20.3%. This prevalence varied by body mass index: 14.2% of normal weight children, 22.3% of overweight children, and 42.9% of obese children had at least 1 abnormal lipid level.3
Pediatricians are aware that hyperlipidemia is just 1 of many risk factors for heart disease that can be improved via changes in diet and exercise or with medication when indicated. Experts have long agreed that screening for elevated lipids should begin in childhood. The National Cholesterol Education Program published previous guidelines for lipid management more than 20 years ago.4
Over the course of the last 2 decades, the incidence of obesity in childhood has increased dramatically, and many studies have demonstrated a definite correlation between hyperlipidemia diagnosed in childhood and the severity of atherosclerosis as these patients grow into adults. The most recent recommendations were published in 2011 by the National Heart, Lung, and Blood Institute.5 These guidelines have been endorsed by the American Academy of Pediatrics and fully describe how pediatricians should encourage a heart-healthy lifestyle by promoting a nutritious diet as well as exercise, discouraging children from smoking, and screening patients for hypertension and hyperlipidemia.
Also included in the guidelines are management recommendations for treating patients for obesity, hypertension, and smoking, as well as for elevated lipid levels. The report makes for a good read because the full document is in excess of 200 pages. A thorough review of the recommendations of the panel in regard to managing elevated lipids was published last year in Contemporary Pediatrics.6 The bottom line is that it is important for pediatricians to screen our patients for elevated lipids while encouraging a heart-healthy lifestyle.
Two approaches
In the past, 2 approaches regarding screening children for hyperlipidemia were promoted. One was a targeted approach based on a history of elevated lipids or early onset of angina, myocardial infarction, or stroke in family members. The other was a universal screening approach in which every child is screened for elevated lipids.
The new guidelines integrate both approaches. The Expert Panel recommended that all children aged 9 to 11 years should have lipid screening once and again when aged 17 to 21 years. If, however, there is a family history of elevated lipids or early onset heart disease or stroke, then children may be screened when aged between 2 and 8 years or between 12 and 16 years.
This means that pediatricians need to ask about details of family history regarding hyperlipidemia, early onset heart disease, or stroke at every well visit. Many practices expedite the process of updating family history by having parents fill out a previsit questionnaire while they are in the waiting area or the exam room before their visit. Parents should be questioned about a history of cardiovascular disease in grandparents, aunts, and uncles. They should be asked whether family members have experienced heart attacks, angina, or strokes in males aged younger than 55 years, or in females younger than 65 years, or if either parent has a total cholesterol of 240 mg/dL or higher.
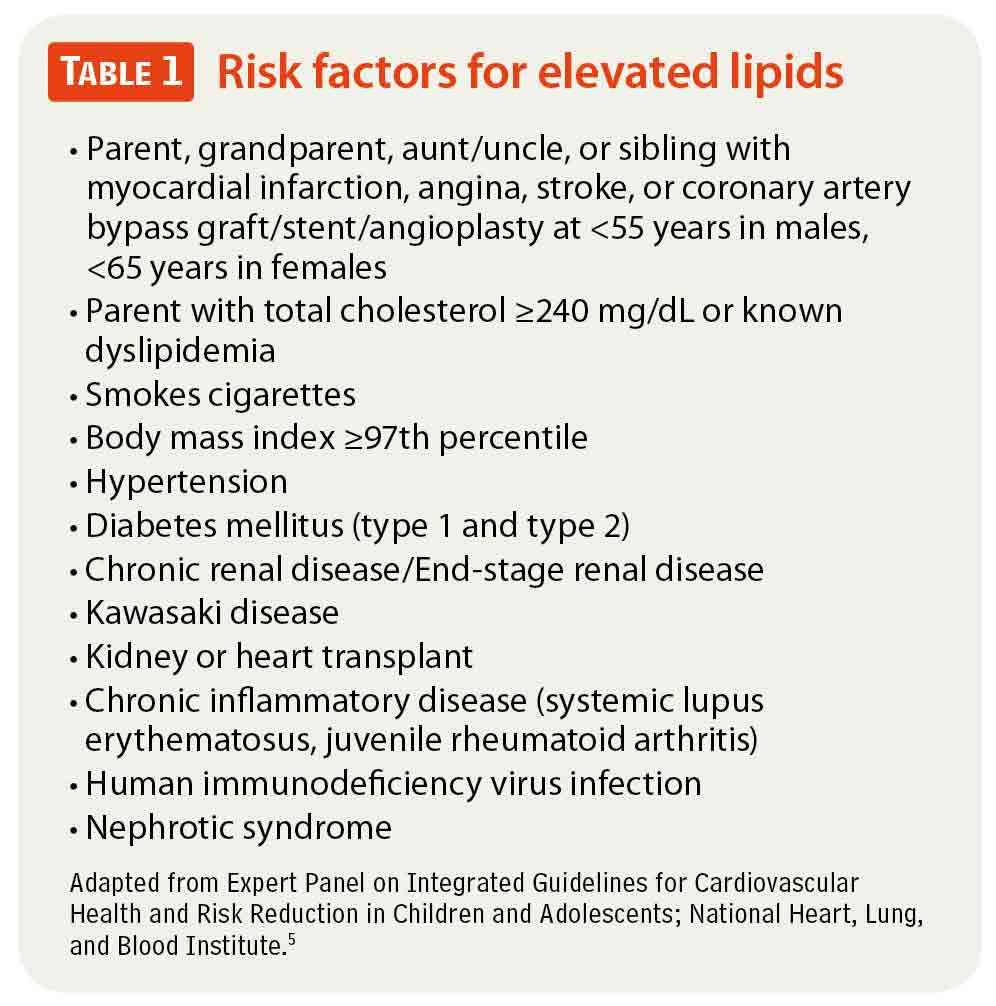
Interestingly, studies have determined screening by family history can miss anywhere from 30% to 60% of children with hyperlipidemia identified by universal screening. One reason is that young parents frequently don’t take as good care of themselves as they do their children and may not know whether they have elevated lipids. Likewise, parents may be unaware of the status of cardiovascular disease in family members. Additional risk factors for hyperlipidemia in children also include obesity, hypertension, and kidney disease, among others (Table 1).5 Consider screening children with these conditions as well if they are not in the age ranges recommended for universal screening.
What to screen for
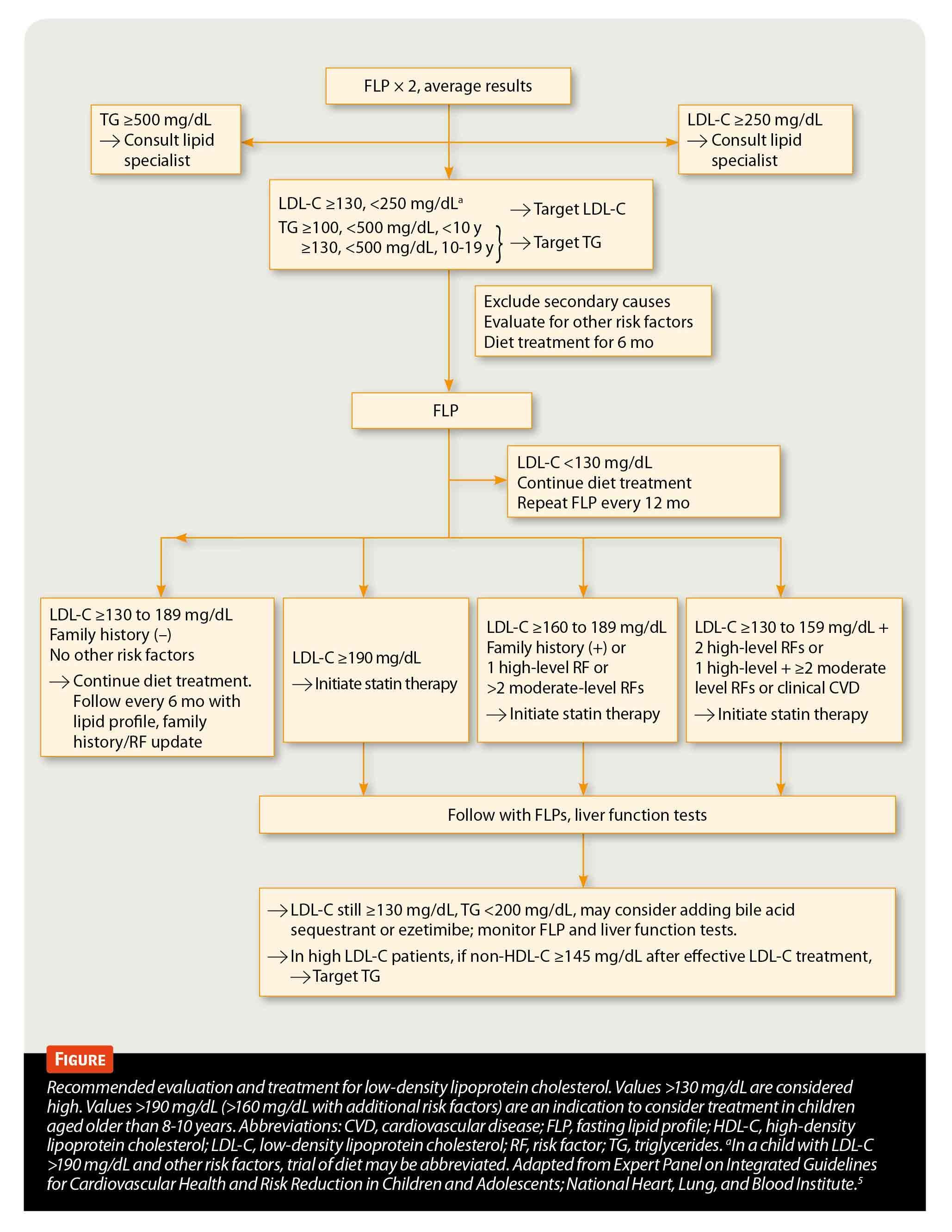
The Expert Panel recommends that children aged between 2 and 8 years or between 12 to 16 years with risk factors for hyperlipidemia be screened with 2 fasting lipid profiles at least 2 weeks but less than 3 months apart and the results averaged.
Children who are aged 9 to 11 years or 17 to 21 years should be universally screened with either:
- A nonfasting lipid profile so that the non–high-density lipoprotein (HDL) cholesterol can be calculated (non-HDL cholesterol=total cholesterol–HDL cholesterol). Those with abnormal results-a non-HDL cholesterol of 145 mg/dL or higher or an HDL of 40 mg/dL or less should then have 2 fasting lipid profiles obtained, with the results averaged.
- A single, fasting lipid profile. If the low-density lipoprotein (LDL) cholesterol is 130 mg/dL or higher, the non-HDL cholesterol is 145 mg/dL or higher, or if triglycerides are 100 mg/dL or higher for children aged younger than 10 years or are 130 mg/dL or higher for children aged 10 years and older, then the fasting lipid should be repeated, with the results averaged.
Devices for lipid screening
Choices for POC testing for lipids include 2 excellent devices that are both CLIA ’88 waived, affordable, and provide results in 5 minutes or fewer. These include the Cholestech LDX System from Alere (Stow, Ohio) and the CardioChek System from Polymer Technical Systems (Indianapolis, Indiana). Both devices are very easy to use, and both manufacturers have done multiple studies, indicating that the devices provide results that correlate extremely well with standard laboratory tests.
The Alere Cholestech LDX System uses a cassette and stationary tabletop analyzer. Every day, the Cholestech LDX is tested with an optics-check cassette to ensure that the device is operating correctly. Alere recommends that controls be run whenever a new shipment of cassettes is received or at least once a month to ensure accuracy.
Performing a screen is very simple. A drop of fingerstick blood is drawn into a collection capillary tube, which in turn is placed in the test cassette. The cassette is inserted into the device, and in fewer than 5 minutes, the results are displayed on the liquid crystal display (LCD) and can be printed via an optional thermal printer. Multiple testing options are available, including a full lipid panel for a fasting test or a total and HDL cholesterol panel for a nonfasting test. A liver function panel and glucose test are available as well, important for screening patients who are obese for metabolic syndrome.
In contrast, the CardioChek PA system is a battery-operated, handheld device that can be brought into a room with a patient. Test strips are available for a fasting lipid panel or a nonfasting total and HDL cholesterol panel, as well as glucose.
A test strip is first inserted into the device, and then fingerstick blood is collected in a capillary tube. The sample is placed on the test strip, and results are displayed on the LCD within 2 minutes. These can be printed by connecting the CardioChek to an optional printer or can be transferred by cable to a laptop running CardioChek software. As with the Cholestech device, controls should be run with each new shipment of testing strips, when a new lot number is used, or at least once per month. The Cholestech LDX sells for approximately $2,000, whereas the CardioChek sells for approximately $800. Tests for both devices cost approximately $10 each. Insurance reimbursement is usually about $20 per test.
What if tests are abnormal?
The Expert Panel guidelines have specific recommendations about treatment when a child is discovered to have abnormal lipid tests (Table 2; Figure).5 Usually dietary changes are recommended for mild abnormalities and referral to a lipid specialist suggested when results are extremely high or when a child does not respond to recommended changes in diet and exercise. Initial dietary management usually includes fat-free, unflavored milk as a primary beverage, limiting sugar-sweetened beverages, and limiting total fat to 25% to 30% of daily caloric requirements while limiting saturated fats to 8% to 10% of daily caloric requirements. Additionally, children and adolescents should avoid trans fats and limit saturated fats to 20% of daily requirements and cholesterol consumption to less than 300 mg per day.
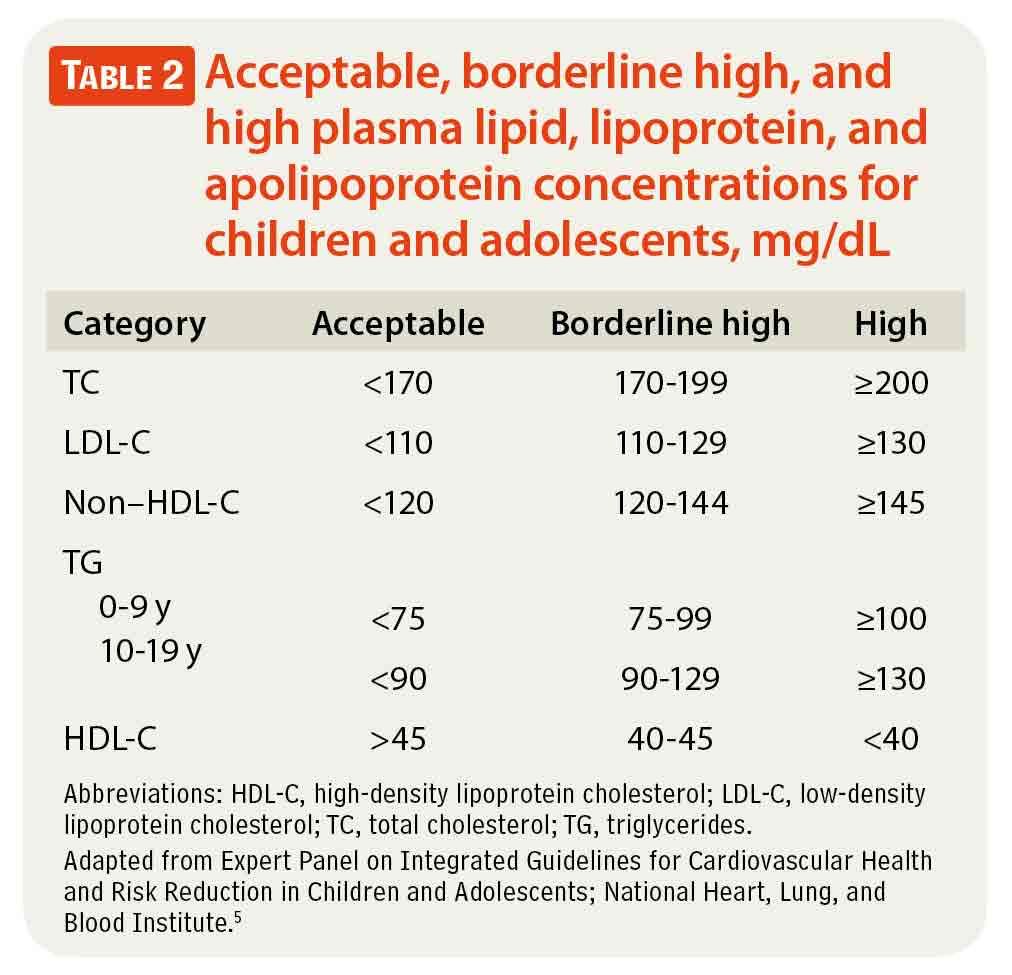
If after 6 months of dietary changes the lipid levels remain elevated, then a more restrictive diet is instituted, with reduction of saturated fats to less than 7% of daily caloric requirements and about 10% from monounsaturated fat and less than 200 mg/day of cholesterol, while continuing to avoid trans fats as much as possible. It is usually recommended that pediatricians refer patients to a nutritionist to help with dietary management and consider referral to a lipid specialist if drug therapy may be necessary.
More POC tests are available . . .
To upgrade your practice to v2.0, consider integrating the latest technology into your daily practice routine. Lipid screening is just one of many office-based POC tests that can provide important results for patients at the time of the health maintenance or illness visit.
References
1. Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650-1656.
2. McGill HC Jr, McMahan CA, Zieske AW, et al. Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. The Pathobiological Determinants of Atherosclerosis in Youth (PDAY) Research Group. Arterioscler Thromb Vasc Biol. 2000;20(8):1998-2004.
3. Centers for Disease Control and Prevention (CDC). Prevalence of abnormal lipid levels among youths-United States, 1999-2006. MMWR Morb Mortal Wkly Rep. 2010;59(2):29-33.
4. National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992;89(3):495-501.
5. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents; National Heart, Lung, and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128(suppl 5):S213-S256.
6. Gidding SS. An emerging dyslipidemia: assessing future CV risk in children. Contemp Pediatr. 2012;29(6):14-24.â¨