New guidelines for community-acquired pneumonia
Recommendations on the diagnosis and management of community-acquired pneumonia.
According to Mark H Sawyer, MD, and professor of clinical pediatrics at the University of California San Diego School of Medicine and Rady Children’s Hospital in San Diego, we should see updates to the guidelines for community-acquired pneumonia (CAP) in 2021. In his session from the virtual 2020 American Academy of Pediatrics National Conference & Exhibition, Sawyer reviewed the present guidelines and discussed the newest approaches to CAP.
Testing and diagnosis
A summary of the guidelines recommends hospitalization of infants (3-6 months) for hypoxia and known Staphylococcus aureus. Use of pulse oximetry is useful to guide severity and is available in the clinic setting, notes Sawyer. Blood cultures, a complete blood count (CBC), and chest x-ray (CXR) have not proven to be helpful in the outpatient setting but does assist in the diagnosis for inpatients. Presently, no urine antigen testing is available as it is with adults. Viral testing is helpful if positive to avoid unnecessary antibiotics, and Sawyer says it is recommended to test for mycoplasma in the school age patient (but not for chlamydophila). Erythrocyte sedimentation rate/C-reactive protein (CRP)/procalcitonin tests may be helpful to follow moderate to severe pneumonia but not in the diagnosis of CAP.
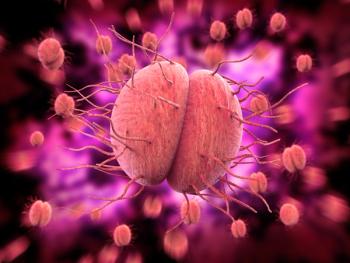
Diagnosis is key to treatment but often signs and symptoms are nonspecific and vary with age. The challenge of diagnosis is furthered by the inability to obtain lower respiratory tract samples. Viruses are the most common cause of pneumonia, but viral and bacterial infections do coexist, and antibiotic management is made more challenging by variable rates of antibiotic resistance in communities, Sawyer reminds us. Community-acquired pneumonia is further complicated now with COVID-19 as well as the increased incidence of vaping. Sawyer did note that ultrasound and nucleic acid-based tests provide some newer advancements in the diagnosis of pneumonia.
Sawyer also reviewed a multicenter study1 looking at CAP in children, diagnostic methods, and coinfections. The study found the median age to be 2 years of age and that underlying disease increased severity of the pneumonia. Common pathogens included respiratory syncytial virus (RSV), influenza, human rhinovirus (HRV), human metapneumovirus (hMPV) with RSV and HRV the most frequently seen and (no surprise here) seen more in winter months. A sub-study2 of this study, done in 2018 showed 26% of hospitalized children had coinfection, with younger children more likely to have viral infections and coinfected patients sicker.
Sawyer further discussed the tools available for diagnosis with ultrasound a growing alternative to CXR, noting that CXR use is decreasing in emergency departments and use of CRP and procalcitonin is not all that helpful, with blood cultures rarely positive. So, what is promising? Included are the increased use of multiplex polymerase chain reaction (PCR) panels and even 16S rRNA PCR, but in particular metagenomics next generation sequencing. Sequencing detects pathogen nucleic acid in plasma or other sources. Sawyer states that “an unlimited number of pathogens could be identified” and performed quickly.
Treatment
Treatment in the outpatient setting is often none for preschool-age children, as viral etiologies are more common in this age group. For suspected bacterial disease, amoxicillin is the drug of choice but in the school-age child, the addition of a macrolide may be considered for the coverage of mycoplasma.
Sawyer suggests to test and treat for influenza; for the inpatient, ampicillin is appropriate, unless there is a high level of penicillin resistance in the community. Says Sawyer, “It is important to know your immunization status as ceftriaxone is recommended for those who are unimmunized. If S aureus is a concern, then addition of clindamycin or vancomycin should be considered. Pneumococcal conjugate vaccine (PCV) and influenza vaccines are key to the prevention of CAP, yet according to Sawyer “a significant number of children still do not get an annual influenza vaccine” and only 83.9% completed the PCV series in 2015. Sawyer suggests evaluating your personal patient’s vaccination coverage rate for PCV13 and influenza vaccines, and “see if you can raise them.”
COMMENTARY
Community-acquired pneumonia is a common problem for every pediatrician. Sawyer gave me a different way of looking at pneumonia. I typically think of CAP as bacterial and approach the diagnosis and treatment with this as my focus. We typically use other terms such as bronchiolitis and bronchitis to describe lower respiratory infections in younger children. Even though an appropriate diagnosis, these terms don’t lend you to see the infections as possible pneumonia. Pneumonia can be viral, bacterial, or a combination, as noted with the rate of coinfection.
The important take-home here is to know when to treat with antibiotics and the appropriate choice of antibiotic. In this time of antibacterial resistance, it is key to know what we are treating and not simply empirically treat all with an antibiotic, particularly when a majority are viral.
The ability to identify the cause of pneumonia with better testing such as next-generation sequencing will only enhance diagnosis and treatment. Vaccinating and encouraging parents to vaccinate not only their children but themselves is interwoven in the health care maintenance visit. This is certainly something I deal with every day as a general pediatrician. New vaccines such as PCV (PCV15 and PCV20) can only further decrease the incidence of bacterial pneumonia and you would expect to see a continued decrease in the rates of pen-resistant pneumococcal disease that has been noted since PCV were introduced. With the right tools available, we will be able to diagnose, treat, and prevent CAP.
References
1. Jain S, Williams DJ, Arnold SR, et al. Community-acquired pneumonia requiring hospitalization among U.S. children. New Engl J Med. 2015;371: 835-845. doi: 10.1056/NEJMoa1500245
2. Nolan VG, Arnold SR, Bramley AM, et al. Etiology and impact of coinfections in children hospitalized with community-acquired pneumonia. J Infect Dis. 2018;2018 (2): 179-188. doi: 10.1093/infdis/jix641
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.