New trends in type 1 diabetes management
The recent advent of "intensive" management has improved the outlook for patients with type 1 diabetes. Its success in children and teens depends on control of hypoglycemia and well-coordinated support from specialists and the primary care pediatrician.
New trends in managing type I diabetes
CME LEARNING OBJECTIVES:

After reviewing this article the physician should be able to:
- Explain the rationale for intensive diabetes management.
- Recommend different diabetes regimens, including insulin pump therapy, and use insulin adjustment algorithms.
- Institute the sick-day management protocol.
- Name several ways to reduce hypoglycemia.
By Francine Ratner Kaufman, MD, and Mary Halvorson, RN, MSN, CDE
The recent advent of "intensive" management has improved the outlook for patients with type 1 diabetes. Its success in children and teens depends on control of hypoglycemia and well-coordinated support from specialists and the primary care pediatrician.
Diabetes mellitus has a unique impact on affected children and their families. The rigors of the diabetes regimen--the need to monitor blood glucose levels often, give insulin injections and adjust insulin dosages, and balance the effects of activity and food--govern their daily lives. They live with fears of severe hypoglycemia or ketoacidosis and diabetic complications that could lead to morbidity or death. In addition to coping with the many issues that surround their disease, children with diabetes must reach the normal developmental milestones of childhood and adolescence and strive to succeed in school and develop autonomy.
Helping these children and their families both to manage diabetes and to accomplish the normal tasks of childhood requires the care of a multidisciplinary team that can address their medical, developmental, psychological, recreational and nutritional needs. The team must consist not only of diabetes specialists and educators who teach diabetes nutrition and self-management principles, but also of primary care physicians who address and coordinate the many aspects of pediatric care.
We will review current principles of diabetes management--specifically so-called intensive management--including insulin regimens, adjustment algorithms for use when a regimen needs modifying, and strategies to prevent severe hypoglycemia and recurrent ketoacidosis during illnesses. We will also address what should be done during follow-up diabetes visits and the importance of coordination between those who provide primary pediatric care and the diabetes care team.
The new approach: "Intensive" management
The goals of current diabetes management are derived from the Diabetes Control and Complications Trial (DCCT).1,2 This primary prevention and secondary intervention trial, which followed 1,441 type I patients between 13 and 39 years of age from 1984 through 1993, showed a significant reduction in the long-term microcirculatory and neuropathic complications of diabetes as a result of intensive management (Table 1). This result was achieved without deterioration of quality of life but at the expense of an increase in severe hypoglycemia (three times greater in the intensive management group than the conventional group).1,2

The trial indicated that an intensive management process (multiple injections, frequent monitoring, dosage adjustments, use of insulin pumps) with comparably intensive outcome goals (reduction in mean blood glucose and glycated hemoglobin levels) has overall benefit for type I patients. The fact that the youngest patients were 13 years of age at entry and adolescents represented only 14% of the study population has not for the most part deterred pediatricians from attempting to achieve the goals set forth in the trial.3 But if intensive management is to be effective and safe for children and teens, it must include strategies to reduce the risk of severe hypoglycemia, and it must provide for adequate support from a team of knowledgeable health-care professionals, including the primary care pediatrician.
Management principles: Blood glucose range
The management goal for infants, children, and teens with type I diabetes is to have blood glucose levels fall within a target range. This target range is age-specific and should take into account the cognitive abilities and resources of the patient and family. Overall, for children over 5 years of age, the target range for premeal glycemia is 70 to 150 mg/dL. Peak postprandial values for these children should be between 120 and 200 mg/dL. As illustrated in Table 2, these ranges are lower than the goal ranges for preschool children and children with cognitive problems, recurrent severe hypoglycemia, and lack of awareness of hypoglycemia. Such children require higher target levels to minimize low blood glucose and its consequences, which may be more pronounced in patients unable to detect the signs of impending severe hypoglycemia.

Determining target blood glucose ranges allows action to be taken when glycemia is not within the desired range. Immediate action to correct problems with the blood glucose level includes correcting low values with supplemental oral glucose and ameliorating hyperglycemia by giving supplemental insulin according to an insulin dosage correction algorithm, changing the composition of the next meal, or increasing activity. To correct an abnormal pattern that has developed over three to seven days or longer, the base dosage of insulin is changed using base dose insulin algorithms.
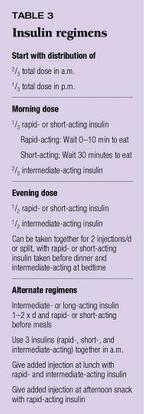
Insulin regimens
Almost all type I pediatric patients are on two or more insulin injections per day consisting of various combinations of rapid-acting lispro insulin (Humalog), short-acting (regular) insulin, intermediate-acting (NPH, lente) insulin, and long-acting (ultralente) insulin (Table 3). The initial dose of insulin for new-onset patients is based on the dosage required to treat ketoacidosis. The starting dose for children who begin treatment as outpatients is calculated on the basis of weight at approximately 0. 5 to 1.5 U/kg/d, depending on the degree of illness as indicated by blood glucose level and the presence of ketonuria or ketonemia. Two thirds of the total initial dosage is given in the morning and one third of the total in the evening. The initial distribution of the morning dose is one third short- or rapid-acting insulin and two thirds intermediate-acting insulin. The evening dose consists of 50% rapid- or short-acting insulin and 50% intermediate-acting insulin. The intermediate-acting insulin is given either with the rapid- or short-acting insulin before dinner, for a total of two injections per day, or separately before bedtime, for three injections per day.
Adjustments to the initial distribution and dosage of insulin are made daily over the phone by the diabetes specialist until most blood glucose levels fall within the target range and a base dose of insulin is established. This usually happens after one to three weeks in the new-onset patient and often coincides with the remission phase (honeymoon period) of diabetes, during which residual insulin secretion occurs in the remaining functional b cells.4 To prolong the remission period, which appears to be induced at least in part by administering enough insulin to nearly normalize the blood glucose pattern, a minimum of two insulin injections per day is continued as the base dose. This total dose, which is given in an attempt to avoid hypoglycemia, may be titrated as low as 0.2 to 0.3 U/kg/d. Phone contact between the parent or patient and the diabetes team is especially important at this time to prevent severe hypoglycemia.
The remission period usually ends within months, and blood glucose control becomes variable. Although, ideally, the diabetes team tells the patient at this time what dose of rapid-or short-acting insulin to take to correct high blood glucose values, the patient also may need to reestablish daily phone contact with the diabetes team so that adjustments of the base dose can be made. The team may tell the patient to adjust not only the amount of insulin taken but the timing of the injections and the type of insulin used. Numerous combinations and permutations of these elements may be necessary. To make multiple injections easier, some of our patients use an insulin pen. The pen can deliver 12 U increments of one type of insulin at a time, making it more likely that patients will accept taking a split dose of insulin at dinner and bedtime, or that they will take insulin at mealtimes.
Since the advent of rapid-acting lispro insulin, we have placed more children and teens of all ages on this insulin despite the fact that it has only recently been approved for use in children. Its quick onset of action (10 to 15 minutes), short duration of action (one to two hours), and efficacy when given immediately before a meal make it an ideal choice for children who are at risk for hypoglycemia and do not wait to eat after injections. For young children whose food intake is unpredictable or children who are sick, it can be given after a meal, reducing the risk of hypoglycemia.5
When a child takes lispro insulin with intermediate-acting insulin before breakfast, however, and no additional insulin between breakfast and dinner, the dinnertime blood glucose reading is often elevated. This has led us to add rapid-, short-, and intermediate-acting insulins together for the morning injection; to give an additional injection of rapid-acting or rapid- and intermediate-acting insulin before lunch; or to give rapid-acting insulin before the afternoon snack to meet individual needs.
Older children and teens occasionally prefer a regimen of intermediate- or long-acting (ultralente) insulin, usually as two injections per day, plus rapid-acting insulin with each meal to match carbohydrate intake. This allows them the freedom to skip or delay a meal, or to markedly alter the meal content. Over time, however, most of these patients have chosen to be placed on continuous subcutaneous insulin infusion (CSII) with an open-loop insulin pump (Figure 1).

Insulin pump therapy
Our center has found CSII, or insulin pump therapy, of benefit to appropriate children and youth. To use this innovative treatment successfully, patients and families must have sufficient knowledge and skills and appropriate attitudes to manage the technology.6 The insulin pump delivers insulin in two ways:
- continuously by basal infusion
- intermittently by bolus.
Children must have the developmental capability to learn how to program the pump and deliver insulin by both of these means. As Table 4 shows, the technical skills a child must have to use the pump independently while at school and away from parental supervision include being able to insert and protect the pump, deliver a dosage of insulin to correct an abnormal blood glucose level and "cover" a meal, and suspend or alter the delivery of basal insulin. These skills usually develop between 8 and 10 years of age. The cognitive skills needed to use CSII independently usually develop later, at or after 10 years of age. This has led our group to recommend CSII for children who are 10 years of age or older, unless the necessary skills and knowledge emerge at a younger age or the child is supervised by a parent or another responsible adult during school hours.

Finally, for CSII to be successful, the child or teen must be cared for by a diabetes team that is familiar with this therapy and able to teach pump management to the patient and family. The primary care pediatrician's involvement in deciding whether the patient and family are appropriate candidates and in co-managing the patient, especially during intercurrent illness, is also critical to success.
Since 1994, we have longitudinally followed patients on CSII to determine the short- and long-term outcomes of treatment.6,7 Presently, we treat 91 children and teens with CSII (approximately 10% of our total type I patient population). They have a mean age of 13.6 ± 3.9 years and a mean diabetes duration of 5.3 ± 3.2 years. They have been placed on CSII for a variety of reasons. We have found the insulin pump to benefit not only highly motivated patients wishing to achieve more life-style flexibility (42% of those using the pump), but also patients in the following groups:
- those with recurrent ketoacidosis, severe dawn phenomenon (elevated blood glucose levels in the morning resulting from the release of counterregulatory hormones, mainly cortisol and growth hormone, during sleep), extremes of glycemic excursion (fluctuations in blood glucose levels from the hypoglycemic to the hyperglycemic range), or poor diabetes control (37% of those on CSII)
- those with severe hypoglycemia (6%)
- a cohort of young children (7 to 10 years of age) who were initially unable to manage CSII independently (15%) but recently became able to do so. This group uses insulin pump therapy only at night when they are under parental supervision. Nighttime treatment has improved nocturnal and morning glycemia.
The patients on insulin pump treatment have shown a significant reduction in mean hemoglobin A1c (HbA1c), an important indicator of overall glycemic control, from 8.6 + 2.3% at initiation of CSII to 7.8 + 1.4% three months later (P = 0.006). (Mean HbA1c was 9.0% for the year preceding CSII, 8.2% during the first year of CSII [P = 0.05], and 8. 1% during the second year [P = 0.04].)7
Insulin adjustment algorithms
Our center uses two types of insulin dosage adjustment algorithms (Table 5). One is for immediate correction of an abnormal blood glucose value outside of the target range, and the other is to change the base dose of insulin after a pattern of abnormal glycemia has been established. The base dose is usually changed after three to seven days of abnormal blood glucose values.

For immediate correction of a blood glucose value outside the target range, incremental adjustments are made for every 50 mg/dL that the blood glucose level is elevated. If the rapid- or short-acting insulin dosage is less than 10 U, 0.5 U is added every 50 mg/dL. If the insulin dosage is greater than 10 and less than 20 U, 1.0 U is added every 50 mg/dL. If the dosage is greater than 20 U, 2 U are added incrementally. The additional dosage can be taken at the time of routine injections and at other times before meals (lunchtime or snacktime in midmorning, afternoon, and bedtime). If it is added as a bedtime injection, we tell families to cut the estimated dosage in half and check two to three hours later to ensure that the additional insulin has not caused hypoglycemia.
We give patients dosage adjustment information on a hand-held Insulin Dosage Guide that our center has developed (Figure 2).8 The patient sets a sliding bar in the middle of the guide at his or her blood glucose level, then reads the insulin dosage change and time to wait before eating in two windows on the lower part of the guide. In evaluations at our center, we have found that using the guide instead of the correction algorithm written on paper leads to a significant reduction of the HbA1c.

The base dose of insulin is adjusted after an abnormal pattern of glycemia has developed. We teach patients to adjust the base dose if the abnormal pattern has been present for either three days in a row or four of seven days. We instruct them to view the day as distinct time periods and tell them which dose of insulin affects the different time periods. For patients on three insulin injections per day, for example, the morning is affected by the nighttime intermediate- or long-acting insulin dosage, lunch by the morning rapid- or short-acting insulin, dinner by the morning intermediate- or long-acting insulin, and bedtime by the dinner rapid- or short-acting insulin. If an abnormal pattern develops during one of these periods, we teach patients how to adjust the insulin dosage that affects that time. The insulin dosage is usually increased or decreased by 0.5 to 1.0 U increments (10% of dosage). To help patients and families learn these principles, we give them a glucose logbook that includes the algorithm (Figure 3).9 Patients at our center who have used the log book for three to nine months have experienced a decrease in HbA1c.

Carbohydrate management
The recommended medical nutrition plan for patients with type I diabetes has changed dramatically since 1994, when carbohydrate management became the nutrition plan of choice.10 This approach emphasizes that the total amount of carbohydrate consumed is more important than the type of carbohydrate, such as simple vs. complex. The overall daily calorie count is evaluated annually by a registered dietician. It remains at 2,000 kcal/m2 or 1,000 kcal + 100/kcal/year of age. The dietician distributes carbohydrate consumption throughout the day based on family eating habits and preferences rather than by the traditional formula of 25% at breakfast, 25% at lunch, 30% at dinner, and 20% for snacks. Insulin doses are adjusted after the meal plan is established.
The recommendation that 25% to 30% of dietary calories come from fat (as much as possible unsaturated), 20% to 25% from protein, and the remaining 50% to 55% from carbohydrate consumption has not changed. Any type of carbohydrate can be consumed as long as it is counted. For this reason and because insulin is required mainly for carbohydrate ingestion, patients and families are taught how to count carbohydrate portions in order to keep their insulin dose in balance with food. Patients use a carbohydrate-to- insulin ratio and determine doses for each meal.
Patients and families who choose to do carbohydrate counting enjoy greater life-style flexibility. This nutrition plan works best for those wishing to lose or maintain weight, such as adolescent girls; for young children, who may be picky eaters; and for patients on multiple insulin injections or insulin pumps.
Sick-day management
Intercurrent illness in children and teens with diabetes can lead to diabetic ketoacidosis, hypoglycemia, dehydration, and deterioration of glycemic control. To avoid these problems, patients and families need to understand the importance of controlling the blood glucose level during illness, and to realize that insulin cannot be withdrawn completely, even in the face of vomiting and poor oral intake. Guidelines for days when the patient is sick should be written down, discussed in advance, and distributed not only to the patient's family but to other caregivers. They should be comprehensive, like the guidelines listed in Table 6, and include phone numbers for the diabetes team and the primary care pediatrician.

Sick-day management calls for frequent blood glucose monitoring, assessment for ketonuria, a marked alteration in insulin dosage, and evaluation of the seriousness of the illness. Families and other caregivers should monitor input and output, temperature, and overall mental status and have on hand oral glucose and electrolyte-containing solutions. The aim is to manage most illnesses at home, avoiding costly hospitalizations and emergency room visits. Making appropriate adjustments to the diabetes management regimen early in the illness is the best way to keep patients at home.
The health-care team should be available to the patient and family 24 hours a day during illnesses to advise them on adjusting insulin dosages and food and fluid intake. If the child is nauseated or vomiting, frequent small doses of rapid-acting insulin may be needed to avoid hypoglycemia. Rapid-acting analogues can be given in small doses as often as every two hours to diminish the risk of hypoglycemia. Similarly, if illness leads to hyperglycemia, frequent higher doses of rapid-acting insulin can be given until ketosis is reversed.
The diabetes team and the primary care pediatrician need to work together. The pediatrician should assess the cause of the illness, determine whether antibiotics or antiemetics are required, and assess hydration status, then relay the information to the diabetes specialist. This information, especially the presence or absence of dehydration, enables the diabetes specialist to give insulin and fluid more effectively to reverse the metabolic consequences of the illness. Finally, the patient needs follow-up by both the general pediatrician (most often during an office visit) and the specialist (most likely by phone for several days) to assess general health and glycemic control.
Preventing hypoglycemia
The diabetes team and primary care pediatrician must talk with each patient and family about that individual patient's risk and susceptibility to severe hypoglycemia. Teachers, school nurses, and other caregivers must also understand the risks. All these people should understand the signs, symptoms, and appropriate management of low blood glucose; the use of glucagon; and when to obtain help. Written instructions on managing hypoglycemia can be given to school personnel by the child's family, provided by the diabetes team, or provided by the school and approved or modified by the diabetes team. Glucose tablets, oral glucose-containing solutions, and glucagon for injection should be available in school, and the potentially hypoglycemic child should not be sent to the nurse's office without another person in attendance. The risk that hypoglycemia will occur during physical activity must be emphasized, and coaches and physical education teachers must allow the exercising child access to glucose when he or she needs it.
Although all episodes of severe hypoglycemia are of concern, nocturnal hypoglycemia is particularly worrisome to patients and their families.11 The incidence of low blood glucose on any given night has been reported to be between 14% and 47%.12,13 It is estimated that at least half the episodes of nocturnal hypoglycemia go entirely undetected.
While glycated hemoglobin levels and intensive management do not appear to be major risk factors for nocturnal hypoglycemia in children,11 certain other things are:
- a history of episodes of low blood glucose (more than two severe hypoglycemic events since diagnosis, more than 24 blood glucose levels below 50 mg/dL in the last two weeks)
- wide fluctuations in blood glucose levels
- going to bed with a glucose level less than 100 to 108 mg/dL
- age younger than 5 to 7 years
- higher daily insulin dosage (greater than 0.85 U/kg/d).
To decrease the risk of hypoglycemia, our center has initiated a hypoglycemia prevention program, particularly for patients who have already had at least one episode of severe low blood sugar. As described in Table 7, this program includes using lispro insulin, using insulin pumps, eating special nighttime snacks containing uncooked cornstarch,14 treating all low blood glucose correctly, particularly at night, and doing intermittent 3 a.m. blood glucose checks. On days when the child is very active, which can lead to late hypoglycemia, or when the insulin dosage or meal plan changes, extra nighttime precautions are in order.

Components of outpatient care
As noted previously, children and teens with diabetes should have access to an organized system of care that uses a multidisciplinary team to assure optimal physical and emotional health for the affected child and support and education for the family, caregivers, and school personnel. The team needs to provide the following components of diabetes care:
- diabetes-specific physical examinations
- 24-four hour access to knowledgeable health-care providers
- assessment and counseling in diabetes management and nutrition
- assessment of competence in diabetes self-care and education needs
- evaluation of social and family functioning and psychological issues
- school or day-care support.
Children and teens with diabetes should have routine health evaluations, ideally quarterly. Table 8 outlines what should be assessed during diabetes-related health care visits. The physical examination should include the following:
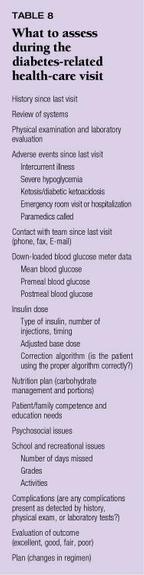
- head circumference until 3 years of age
- height and weight plotted on standard growth charts
- pubertal staging according to the Tanner criteria
- blood pressure compared to age-specific norms. Poor diabetes management has been associated with linear growth failure, abnormal weight-for-height ratio, failure to achieve normal pubertal progression, and early hypertension.15,16
Additional findings on physical examination that have been associated with poor diabetes control in children and adolescents include hepatic enlargement, limited joint mobility, and thickening of the skin.17,18 Thyroid gland size should be evaluated because of the high incidence of coexistent autoimmune-thyroid disease.19 A dilated retinal examination and evaluation for microalbuminuria should be done yearly in children beginning five years after diagnosis.20
Quarterly assessment of HbA1c is imperative. This measurement evaluates overall glycemic control by determining the amount of heme protein to which glucose has been nonenzymatically linked, which reflects the average blood glucose concentration over the preceding two to three months. For this reason, the HbA1c has been referred to as the "report card." The HbA1c should be less than 8% in children younger than 6 years of age, who may be at greater risk than older children for adverse consequences from hypoglycemia, and less than 7% to 7.5% in older children and teens. Values between 8% and 9.5% are considered suboptimal, while levels greater than 9.5% indicate poor glycemic control.
In our center, as in most centers that follow a large number of diabetes patients, we measure HbA1c with the DCA 2000 device (Miles Diagnostics, Tarrytown, NY), which provides results within seven to 10 minutes of testing. Knowing the result during the outpatient visit is especially helpful for patients with undesirable HBA1c values because appropriate changes can be made right away, without losing the impact of the face-to-face encounter. Likewise, if the level is within the desired range, the patient, family, and diabetes team can celebrate together a job well done. For patients with a higher-than-desired level despite having put forth maximal effort to manage their diabetes, more radical modifications of the diabetes regimen can be considered, and when all have been exhausted, mutual support and appreciation can be offered.
Sometime shortly after diagnosis, patients should be evaluated for islet-cell antibodies (ICA), to confirm the diagnosis of type I autoimmune diabetes.21 Commercial laboratories can now measure accurately antiglutamic acid decarboxylase antibodies, insulin autoantibodies, and ICA. Because of the increased risk of autoimmune thyroidititis, thyroid function tests and antithyroid antibodies should be obtained at diagnosis and periodically thereafter as indicated (yearly or more often in the thyroid gland is enlarged). Lipid profiles may be obtained in older children and teens, in patients with poor glycemic control, and in those with a family history of hyperlipidemia. Since children with diabetes are at increased risk of celiac disease, they should be assessed for that disorder if they have gastrointestinal symptoms or poor growth.
The collaborative care system
Active collaboration between the primary care pediatrician and the diabetes team is essential for optimal outcome. The pediatrician must be aware of the patient's specific regimen, findings on quarterly evaluations, HbA1c results, the plan for managing intercurrent illness, issues surrounding the family, the psychosocial adaptation of the patient, problems at school or during other activities, and adverse events. He or she gives routine pediatric care, sees that developmental and behavioral issues are addressed, makes sure that the child and family are adjusting to chronic illness, and offers age- and gender-appropriate anticipatory guidance.
The pediatrician can also help the patient obtain diabetes supplies and equipment, arrange subspecialty care visits, and consult with the patient and family about whether the patient should enter experimental protocols offered by the diabetes team or the broader diabetes research community. Finally, the pediatrician should serve as the patient's advocate with the parents, other caregivers, school personnel, coaches, and most important, the diabetes team.
Subspecialists are most qualified to determine what insulin regimens, adjustment algorithms, sick-day protocols, and medical nutrition plans patients should follow. They should communicate with the pediatrician about why they recommend certain treatment options and when and why they change insulin doses or other aspects of management. Because so many patients are now enrolled in managed care plans that use case-rate reimbursement for subspecialty care, primary care pediatricians are starting to do some quarterly examinations for patients at our center, following our diabetes-visit protocol. Information from these visits is tracked on our diabetes disease management computer data base.22 This development has enhanced the collaboration between our center and primary care pediatricians, thus benefiting patients and their families.
A complex undertaking
Caring for children and youth with type I diabetes is a complex, collaborative effort involving many health-care providers and many management decisions. Periodic health and psychosocial assessments and quarterly assessments of HbA1c are critical for optimal outcome. Of equal importance is a good working relationship between the diabetes team and the primary care pediatrician.
DR. KAUFMAN is Professor of Pediatrics at the University of California School of Medicine and Head, Division of Endocrinology and Metabolism
at Children's Hospital, Los Angeles. She is a consultant for MiniMed, Inc. and Integ Corporation, a stockholder in MiniMed, and holds a patent on the Extendbar (Clinical Products Limited). She also serves on the speaker's bureaus of Eli Lilly & Company and Novo Nordisk. She has received grants or research support from Bristol Myers Squibb, Genentech, Pharmacia & Upjohn, Eli Lilly & Company, Novo Nordisk, Pfizer, and MiniMed, Inc.
MS. HALVORSON is Director, Diabetes and Research, and Case Manager at Children's Hospital Los Angeles.
REFERENCES
1. Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the long-term development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977
2. Diabetes Control and Complications Trial Research Group: The effect of intensive treatment of diabetes on the development and progression of long-term complications in adolescents with insulin-dependent diabetes: The Diabetes Control and Complications Trial. J Pediatr 1994;125:177
3. Kaufman FR: Diabetes mellitus. Pediatr Rev 1997; 18:383
4. Wilson D: Diabetes mellitus in children and adolescents, in Behrman RE, Kliegman RM, Arvin AM (eds): Nelson's Textbook of Pediatrics, ed 15. Philadelphia, PA, WB Saunders, 1995, pp 112
5. Anderson JH Jr, Brunelle RL, Koivisto VA, et al, the Multicenter Insulin Lispro Study Group: Improved mealtime treatment of diabetes mellitus, using insulin analogue. Clin Ther 1997;19:62
6. Kaufman FR, Halvorson M, Miller D, et al: Insulin pump therapy in the type I pediatric patient: Indications and outcomes, in Laron Z, Pinelli L (eds): New perspectives in childhood diabetes and childhood obesity: 7th International ISPAD Course. Cosenza, Italy, Editoriale Bios sas, 1999, pp 111127
7. Kaufman FR, Halvorson M, Miller D, et al: Insulin pump therapy in type I pediatric patients: Now and into the year 2000. Diabetes Metabolism and Reviews (in press)
8. Kaufman FR, Halvorson M, Carpenter S: Use of a plastic insulin dosage guide to correct blood glucose levels out of the target range and for carbohydrate counting in children with type I diabetes (submitted)
9. Halvorson M, Carpenter S, Kaufman FR: Use of a logbook containing the base dosage adjustment algorithm in patients with type I diabetes. Diabetes 1997;46:37A
10. American Diabetes Association: Standards of medical care for patients with diabetes mellitus. Diabetes Care 1997;20 (suppl 1): S5
11. Kaufman FR: Diabetes in children and adolescents: Areas of controversy. Med Clin North Am 1998;82:721
12. Beregszaszi M, Tubiana-Rufii N, Benali K, et al: Nocturnal hypoglycemia in children and adolescents with insulin-dependent diabetes mellitus: Prevalence and risk factors. J Pediatr 1997;131:27
13. Porter PA, Keating B, Byrne G, et al: Incidence and predictive criteria of nocturnal hypoglycemia in young children with insulin-dependent diabetes mellitus.
J Pediatr 1997;130:366
14. Kaufman FR, Halvorson M, Kaufman ND: A randomized, blinded trial of uncooked cornstarch to diminish nocturnal hypoglycemia at diabetes camp. Diabetes Res Clin Pract 1995;30:205
15. Mauriac P: Hepatomegalies de l'enfants avecs troubles de la croissance et due metabolisme des glucide. Paris Med 1934;2:525
16. Lieberman LS, Rosenbloom AL: Changes in growth and body composition related to control in children with diabetes, in Borns J, Hauspie R, Sand A, et al (eds): Human Growth and Development. New York, Plenum, 1984
17. Rosenbloom AL, Silverstein JK, Lezotte DC, et al: Limited joint mobility in diabetes mellitus in childhood: Natural history and relationship to growth impairment. J Pediatr 1982;101:874
18. Buckingham BA, Uitto J, Sandborg C, et al: Scleroderma-like changes in insulin-dependent diabetes mellitus: Clinical and biochemical studies. Diabetes Care 1984;7(2):163
19. Riley WJ, Maclaren NK, Lezotte DC, et al: Thyroid autoimmunity in insulin-dependent diabetes mellitus: The case for routine screening. J Pediatr 1981;98:350
20. Santiago JV (ed): Medical Management of Insulin-Dependent Diabetes, ed 2. Alexandria, VA, American Diabetes Association, 1994
21. Mortensen BB, Hougaard P: Comparison of metabolic control in a cross-sectional study of 1,873 children and adolescents with IDDM from 18 countries. Diabetes Care 1997;20:714
22. Halvorson MJ, Barry TL, Kaufman FR: Advances made in pediatric diabetes care using an outcome research model: A five-year study. J Investigative Med 1999;47:13A

CONTINUING MEDICAL EDUCATION
ACCREDITATION
This activity has been planned and implemented in accordance with the Essentials and Standards of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Jefferson Medical College and Medical Economics, Inc.
Jefferson Medical College of Thomas Jefferson University, as a member of the Consortium for Academic Continuing Medical Education, is accredited by the Accreditation Council for Continuing Medical Education to sponsor continuing medical education for physicians. All faculty/authors participating in continuing medical education activities sponsored by Jefferson Medical College are expected to disclose to the activity audience any real or apparent conflict(s) of interest related to the content of their article(s). Full disclosure of these relationships, if any, appears with the author affiliations on page 1 of the article.
CONTINUING MEDICAL EDUCATION CREDIT
This CME activity is designed for practicing pediatricians and other health-care professionals as a review of the latest information in the field. Its goal is to increase participants' ability to prevent, diagnose, and treat important pediatric problems.
Jefferson Medical College designates this continuing medical educational activity for a maximum of one hour of Category 1 credit towards the Physician's Recognition Award (PRA) of the American Medical Association. Each physician should claim only those hours of credit that he/she actually spent in the educational activity.
This credit is available for the period of October 15, 1999, to October 15, 2000. Forms received after October 15, 2000, cannot be processed.
Although forms will be processed when received, certificates for CME credits will be issued every four months, in March, July, and November. Interim requests for certificates can be made by contacting the Jefferson Office of Continuing Medical Education at 215-955-6992.
HOW TO APPLY FOR CME CREDIT
1. Each CME article is prefaced by learning objectives for participants to use to determine if the article relates to their individual learning needs.
2. Read the article carefully, paying particular attention to the tables and other illustrative materials.
3. Complete the CME Registration and Evaluation Form below. Type or print your full name and address in the space provided, and provide an evaluation of the activity as requested. In order for the form to be processed, all information must be complete and legible.
4. Send the completed form, with $20 payment if required (see Payment, next page), to:
Office of Continuing Medical Education/JMC
Jefferson Alumni Hall
1020 Locust Street, Suite M32
Philadelphia, PA 19107-6799
5. Be sure to mail the Registration and Evaluation Form on or before October 15, 2000. After that date,
this article will no longer be designated for credit and forms cannot be processed.
FACULTY DISCLOSURES
Jefferson Medical College, in accordance with accreditation requirements, asks the authors of CME articles to disclose any affiliations or financial interests they may have in any organization that may have an interest in any part of their article. The following information was received from the authors of "New trends in managing type I diabetes."
Francine Ratner Kaufman, MD, is a consultant for MiniMed, Inc., and Integ Corp. She is a stockholder in MiniMed and holds a patent on the Extendbar (Clinical Products Limited). She serves on the speaker's bureaus of Eli Lilly & Co., Novo Nordisk, and has received grants or research support from Bristol Myers Squibb, Genentech, Pharmacia & Upjohn, Eli Lilly, Novo Nordisk, Pfizer, and MiniMed.
Mary Halvorson, RN, MSN, CDE, no information to disclose.
CME REGISTRATION AND EVALUATION FORM
Date of publication: October 1999
Title: "New trends in managing type I diabetes"
Author: Francine Ratner Kaufman, MD, and Mary Halvorson, RN, MSN, CDE
MP Code: CP1099
Registration
Name:
Degree:
Street address:
Institutional affiliation:
City: _________________________________________ State: ________ ZIP: ____________ Telephone ________________________
Specialty: [ ] Pediatrics [ ] Other __________________________________ Years in practice: ___________ Resident?__________
Time needed to complete this CME activity: [ ] <1 hr [ ] 1 hr [ ] 1.5 hr [ ] 2 hr
Certification: I attest to having completed this CME activity.
Signature (required)
Evaluation
1. Rate the overall effectiveness of this CME activity. 5 (very effective) 4 3 2 1 (not at all effective)
2. Circle "Yes" or "No"
Yes / No [A]. The learning objectives were useful to me in determining whether performing this CME activity would be a worthwhile educational experience for me.
Yes / No [B]. The objectives accurately described the content and potential learning value of this article.
Yes / No [C]. This activity will influence how I practice medicine.
Yes / No [D]. The activity was free from commercial bias.
Yes / No [E]. I learned something new that was important from the article.
3. Which of the following best describes a change you might consider making in your practice as a result of something you learned from this activity? (Please circle only one response.)
[A]. Slightly modify what I currently do.
[B]. Make a major change in what I currently do.
[C]. Follow a procedure, use a technique/technology that is completely new to me.
[D]. Follow a procedure, use a technique/technology that I currently use but for a different purpose.
[E]. None of the above, but some change.
[F]. Not considering any changes.
4. Please describe any change(s) you plan to make in your practice as a result of this activity:
5. How committed are you to making these changes? 5 (very committed) 4 3 2 1 (not at all committed)
6. Other comments
Payment
Circle A, B, or C, and enclose payment if required.
A. I am a paid subscriber to Contemporary Pediatrics, so no payment is due.
The expiration date above my name on the mailing label is: ___ ___ ___ ___ ___ (Example: D E C 9 9 ).
B. I have ordered a paid subscription, so no payment is due, but I do not have an expiration date yet.
C. I receive Contemporary Pediatrics without charge, so I must pay $20 to cover the cost of processing my CME application.
[ ] I am enclosing a check (payable to JMC/CME).
[ ] Please charge my Mastercard or Visa (circle type of card),
account number: ___ ___ ___ ______ ___ ___ ______ ___ ___ ______ ___ ___ ___ , expiration date: ___ ___ /___ ___
Signature (required)
Send the completed form to:
Office of Continuing Medical Education/JMC, Jefferson Alumni Hall, 1020 Locust Street, Suite M32, Philadelphia, PA 19107-6799.
Francine Kaufman,Mary Halvorson. New trends in type 1 diabetes management.
Contemporary Pediatrics
1999;10:112.