New weight-management algorithm
The long-awaited American Academy of Pediatrics (AAP) weight-management algorithm for obesity provides a comprehensive, evidence-based translation for real-world use.
The long-awaited American Academy of Pediatrics (AAP) weight-management algorithm for obesity provides a comprehensive, evidence-based translation for real-world use, said Ihuoma Eneli, MD, MS, FAAP, at the AAP’s 2016 National Conference. She discussed the guideline in her session "The new AAP algorithm: Finally! What the evidence says Is the best way to manage obesity."
Recommended: Are low-income kids at greater risk for obesity?
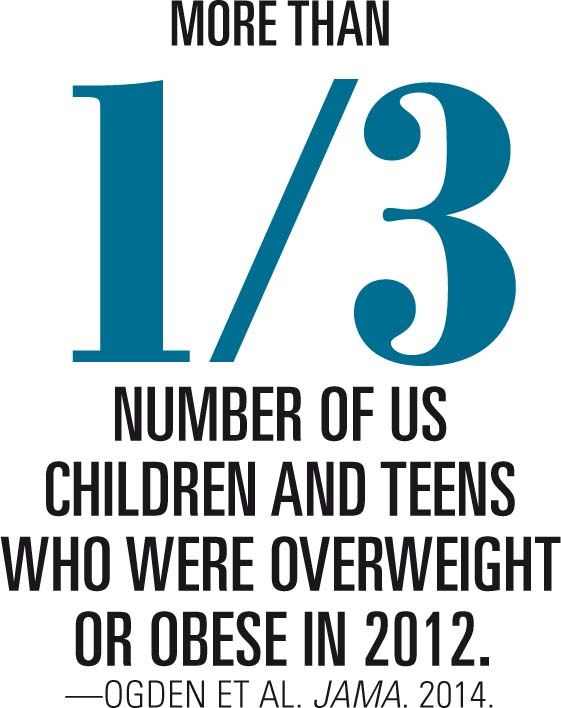
Until an Expert Committee convened by the American Medical Association Health Resources and Service Administration and the Centers for Disease Control and Prevention published obesity recommendations in 2007,1 pediatricians had no structured format to translate these guidelines into treatment for childhood obesity. The new AAP Algorithm for the Assessment and Management of Childhood Obesity in Patients 2 Years and Older2 incorporates these guidelines along with recent evidence and expert opinions.
Like the Expert Committee recommendations, the AAP algorithm links treatment recommendations to community resources, giving clinicians a coordinated approach by bringing all the evidence together to support specific suggestions in areas such as assessing the family situation, ordering laboratory tests, and setting treatment goals.
The algorithm divides obesity treatment into 4 stages, marked by increasing interventional intensity. Children should begin at the lowest stage appropriate for their body-mass index, age, and presence of comorbidities.
The first 2 stages, Prevention Plus and Structured Weight Management, occur in the primary care pediatrician's office. Stage 2 requires primary care pediatricians to provide counseling with assistance from an allied health professional such as a dietitian or health coach.
At every stage, the algorithm spotlights the importance of motivational interviewing, using tactics such as shared agenda setting and eliciting self-motivational statements from patients to boost compliance. To hone this skill, pediatricians may access the free Change Talk program developed by the AAP Institute for Healthy Childhood Weight via the interactive app available at Google Play and Apple iTunes. Through an online avatar, Change Talk walks users through common scenarios that occur in the primary care office.
REFERENCES
1. Barlow SE; Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(suppl 4):S164-S192.
2. American Academy of Pediatrics Institute for Healthy Childhood Weight. Algorithm for the assessment and management of childhood obesity in patients 2 years and older. Available at: https://ihcw.aap.org/Documents/Assessment and Management of Childhood Obesity Algorithm_FINAL.pdf. Updated August 2016. Accessed October 21, 2016.
NEXT: Commentary
COMMENTARY
The new AAP algorithm reformats information that has been available since 2007 in a clear, easy-to-understand format, spelling out in visual form what it takes as one moves through the different stages of obesity and interventions. It supports primary care doctors in determining how long to work with patients on each stage before increasing the intensity of the services they offer.
The algorithm specifies spending 3 to 6 months in each stage. Spending the recommended 3 to 6 months in each stage is challenging for families, especially at the intensity level required to treat children with severe obesity.

Most children between the 85th and 95th body-mass index (BMI) percentile respond to intervention in the primary care office. However, children with more severe obesity typically spend up to 6 months each with their primary care physician, then with primary care plus a dietitian, before being referred to a multidisciplinary clinic if needed. If this approach fails, Stage 4 treatment includes consideration of medical and surgical treatments. Usually, patients spend 2 years of hard work on making healthy changes, while also struggling against a chronic disease.
Patients and families get tired. That is why motivational interviewing is so important. Shaming, blaming, or berating families does not work. They already feel like failures because they are expending significant effort, in most cases, and are not seeing the desired weight changes.
As Dr Eneli pointed out, the key is making sure to help every family with healthy lifestyles and interventions as early-in age and stage-as possible. As compared with overweight or obesity below the 98th or 120th (of the 95th) percentile, depending on which approach one uses to characterize elevated BMI,1,2,3 we know that it is much more difficult to effectively address severe obesity.
REFERENCES
1. Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: a new growth chart. Pediatrics. 2012;130(6):1136-1140.
2. Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999-2014. Obesity (Silver Spring). 2016;24(5):1116-1123.
3. Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314-1320.
Mr Jesitus is a medical writer based in Colorado. He has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.