Oral and facial trauma
Mouth injuries are common in children, but pediatricians may not feel confident in handling them. These guidelines can help you identify the problems, make timely referrals, and educate patients and their families in prevention.
Athletes and other children frequently sustain mouth injuries while engaging in sports or at play, yet many pediatricians may feel unprepared to cope with mouth trauma and may not know what to look for or how to proceed in emergencies.
What to look for
When a child with oral or facial injuries is examined, trauma to the mouth is not your first concern. Priority is given to any central nervous system damage, hemorrhage, eye or ear injury, or cranial nerve damage-injuries that may require immediate attention.
After determining that the child does not have any of these injuries, you should check for oral pathology: discolorations, asymmetries, depressions, prominences, osseous step deformities, obvious broken bones, broken or missing teeth, or temporomandibular joint (TMJ) issues.
The intraoral examination should include an evaluation of malocclusions and abnormal mobility (lack of normal range or expected range of motion of the jaws). Examine the inside of the mouth for bleeding, swelling, and teeth that are displaced, broken, or missing.1
The injuries you may find can be divided into 4 categories: injuries to the soft tissues; injuries of the TMJ; jaw fractures and displacements; and injuries to the teeth.
Soft-tissue injuries
If you find lacerations of the soft tissues of the mouth, a determination should be made whether they require suturing. This depends on the size of the laceration; whether there are any vital structures involved such as major blood vessels, salivary ducts, muscles, or exposed bone; or whether muscle tension during function will retard healing.
If suturing is required and you feel comfortable working inside the mouth, you may elect to do the repair yourself (Figure 1). Alternately, you may choose to refer the patient to a dentist or oral surgeon.2

If a torn labial or lingual frenum is found, a dentist should evaluate these injuries, and if they are substantial, they will need to be treated immediately (Figure 2). However, many times they do not require immediate treatment and primary closure and may possibly be left to heal on their own.

Injuries to the gums that leave the periosteal bone exposed must be treated because unprotected bone is likely to become necrotic and delay healing (Figure 3).

Dislocated jaw
If a patient presents after a traumatic injury with the mouth propped open and complains of pain and the inability to close the mouth, first rule out a jaw fracture. If no jaw fracture is found, then suspect that the mandible has been subluxated.
In this case, the mandible has been forced open so far that the condylar head of the mandible has overrotated and translated forward so far that it is now positioned anterior to the articular eminence of the maxilla.
Here it is trapped in this forward position by the powerful masseter muscle, which pulls upward and backward, thereby preventing the mandible from repositioning itself back into the articular fossa.
This TMJ subluxation should be reduced as soon as possible before the muscles go into spasm. It is important to remember that when the repositioning maneuver succeeds, the mandible can snap back into place suddenly and with great force, posing a serious danger to the manipulator’s fingers (see, “Repositioning a TMJ Displacement”).
After the TMJ subluxation has been reduced, the child should be instructed not to open the mouth widely for at least 24 hours and to stick to a soft diet, with no gum chewing.3,4 The overstretched TMJ ligaments need time to shrink and heal or else the child may be prone to repeated episodes of TMJ subluxation.
Traumatic overstretching of the TMJ ligaments may occur after an injury without the mandible becoming trapped anteriorly. Here again a soft diet, rest, and possibly analgesics and anti-inflammatory medications may be beneficial to aid proper healing.
Repositioning a TMJ displacement
A recent TMJ displacement can usually be reduced by this simple maneuver. Remember that when you are successful, the jaws snap back into place quickly and with great force; don’t let your fingers get trapped. This is how it’s done.
1. Tape tongue depressors above and below your thumbs for protection.
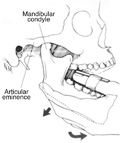
2. Press down on the lower molars with your thumbs and grasp the angle of the mandible with your fingers.
3. Give 1 quick, downward and forward rotation of the mandible. The jaw will snap back into the correct position. A day of soft food, no chewing gum, and rest helps heal the ligaments.

Broken bones in the mouth
Injuries to the mouth may produce jaw (maxilla or mandible) fractures or fractures of the tooth sockets. Even if the jaw is fractured, the injury may not be obvious.
Mandibular fractures are 8 times more likely to occur than maxillary fractures.5 Maxillary fractures, however, tend to be more dramatic because they can produce considerably more swelling and bruising.6-9 A trained eye can identify jaw fractures in many routine radiographic images (Figure 4).

A panoramic radiograph, however, is the image of choice to identify mandibular jaw fractures (Figure 5).1,7 Both the maxilla and the mandible have favored places where fractures tend to occur.10,11 In children, most mandibular fractures are found in the subcondylar area or adjacent to the mandibular symphysis.12
Knowing the direction and nature of the impact to the mandible can help one find where the fractures may have occurred.12 So, for example, with impacts to the right side of the jaw, look for possible fractures adjacent to the impact site but also in the left subcondylar area.

With blows directly to the chin, suspect fractures on either side of the mandibular symphysis. In the case of impact under the chin, check for fractures in both right and left subcondylar areas.
Your patient may suffer an impact to the face and come in complaining of extreme pain in the area of the upper anterior teeth. The teeth may be firm, the bite may appear normal, and no obvious sign of a jaw fracture may be present. You may, however, notice a very profound bruising in the maxillary anterior labial vestibule.
The patient should be referred to a dentist to confirm that there are no root fractures.13 However, this patient has probably fractured the anterior nasal spine of the maxilla. Although quite painful, these injuries usually heal by themselves, and only palliative care is indicated (Figure 6).

Fractures of the jaw may or may not be displaced.7 Displacement is influenced by many factors: the direction of the fracture line; the angle of the bevel of the fracture line; the direction of the adjacent muscle pull; whether teeth are present on the jaw fragment; the extent of the soft tissue wound, if any; and the direction and intensity of the traumatic force.
If you suspect that a jaw fracture may have occurred, the child should be referred to an oral surgeon. Prompt treatment makes immediate reduction of the fracture possible. A rigid splint is placed on the maxillary and mandibular teeth, and the teeth are brought into occlusion and stabilized.
Some initial healing may have taken place if more than 24 hours have passed. In these cases, the fractured segments may not be easily manipulated, and so a progressive reduction of the fracture may be necessary. Rigid splints are placed on the intact maxillary and mandibular components, then the displaced fractured segments are slowly brought into occlusion using rubber bands that are added sequentially over time.5
Tooth injuries
Young children slowly learn the protective reflex of putting their hands out in front of them to brace themselves in a fall, so quite often these young patients will sustain injuries to the front teeth and bony sockets.14,15 The teeth may be displaced as the supporting bone is fragmented. The teeth may be partially or completely avulsed. They may also be displaced lingually far enough that they now interfere with the arcing closure path of the mandible. Here, the patient is left unable to close the mouth without hitting the displaced front teeth (Figure 7).

A helpful question to ask the patient is to try and close the mouth with the molars touching. If the child cannot do this, he or she should be referred to a dentist so that the displaced front tooth or teeth can be repositioned and splinted.1,6,11,16
Until the displaced tooth or teeth are repositioned to eliminate the interference, the patient will be quite uncomfortable and unable to close the mouth.
Emergency intervention is indicated when a child presents with a history of an avulsed tooth. If the tooth, or the fragments of a fractured tooth, cannot be located, a chest x-ray may be necessary to rule out the possibility that the tooth was aspirated.
This is especially true if the patient is experiencing any breathing abnormality. Avulsed primary teeth are usually not reimplanted (Figure 8).

Occasionally, especially with toddlers, the child can come in after sustaining trauma to the mouth with the incisor tooth (usually upper) avulsed, but it cannot not be found. No breathing issues are noted.
One possibility is that the incisor was swallowed. However, another possibility is that the incisor may have been impacted up into the alveolus by the trauma, and if a radiograph is taken (a dentist can do this), it can be seen there.11
A dentist should be consulted as soon as is reasonably possible to rule out this possibility. The dentist will then need to decide in the case of an impaction injury if the tooth can be left to re-erupt on its own, which it may do, or if the tooth needs to be actively repositioned down and splinted.
Partially avulsed permanent teeth should be repositioned and splinted as soon as possible (Figure 9).11 The child should be referred to a dentist immediately so that the most favorable outcome can be achieved.6,7,16

Completely avulsed permanent teeth should be reimplanted immediately or as soon as possible.11 The longer the tooth is out of the mouth, the poorer the chance for a successful outcome. The technique is simple and can be taught to parents and school health personnel.17
• Make sure that the tooth socket is clean and free of any foreign material or blood clot by gently wiping or lightly irrigating the site.
• Anesthesia is usually not needed to reimplant an avulsed tooth.
• Try not to handle the root of the tooth because the surface can be easily damaged.
• If there is debris on the root, gently rinse it with warm water but do not try to scrape it clean.
• Fit the tooth back into the socket as best as you can, even if that means placing it backward or at an angle.
• The child should bite on some gauze to stabilize the tooth and prevent aspiration until being seen by the dentist to splint the tooth for stabilization.
• If it is determined that the child is unable to reliably stabilize the reimplanted tooth in the mouth during transport, to avoid the risk of aspirating the tooth, reimplantation should be delayed until a dentist can be consulted and a stabilizing splint placed.
• In this case, the tooth should be stored in some liquid medium during transport to the dentist, but try to avoid dry transport. A desiccated tooth has very poor chances for survival.
The patient should see a dentist as soon as possible because the tooth will need to be stabilized with a splint (Figure 10). Of course, any associated medical needs should be addressed, and a determination should be made of the need for immunizations.

If whoever is with the child at the time of the accident is unable to reimplant the tooth or the child is too young or too upset to be trusted with a loose reimplanted tooth in the mouth while traveling to the dentist for splinting, then the avulsed tooth must be protected from desiccation while outside the mouth and being transported to the dentist. The tooth can be transported in milk, isotonic saline, Gatorade, contact lens solution, or water. Transporting the tooth dry is the least favorable option.
Another option is to use a commercially available, emergency transporting system called Save-a-Tooth.7,16 The product contains Hanks Balanced Salt Solution (HBSS) as the transporting liquid (Figure 11).
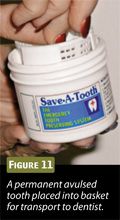
This will keep the tooth hydrated and supply supportive nutrients as well. The system is easy to use and has a reasonable shelf life so that it can be easily maintained in an emergency kit at any sporting event, doctor’s office, or home medicine cabinet.
Broken teeth
Children often fracture their teeth or lose them entirely. Unfortunately, such injuries are often permanent and may affect not only the injured teeth but the remaining teeth as well. Pediatricians who see such injuries are in a position to minimize the damage by providing emergency treatment themselves or by referring the patients for care by a dentist.
If after a traumatic injury the child complains that the teeth “do not fit correctly,” suspect a mandibular displacement. After ruling out a jaw fracture, check for fractured or lost molars (Figure 12).16

The molars establish the vertical height of the jaw and support the weight of the bite. If a molar is fractured or lost, several things can happen. The jaws normally come together in a wedge pattern, with the molars in the back and the incisors in the front. Also, the mandible closes in an arcing fashion.
With the loss or damage to a molar, the vertical height support will be affected and the mandible will tend to over rotate and over close (Figure 13). The teeth will now meet differently, and more weight will be transferred to the teeth anterior to the affected molar. Prompt referral to a dentist is indicated.

There is one last possibility to consider when a mandibular displacement is noted after a traumatic injury. If both a jaw fracture and damaged or missing molars are ruled out, suspect soft tissue trauma to the TMJ and supporting muscles, which can influence the jaw position. Here analgesics, anti-inflammatory medications, moist heat, rest, and a soft diet are appropriate.
Anterior teeth are frequently injured. Superficial (enamel only, or enamel and dentin) fractures, although uncomfortable, are not acute emergencies (Figure 14).11 The patient should be referred to a dentist to cover or repair the fractures at the earliest convenience.

If the fracture is deeper and exposes the pulp tissue (blood evident on the fracture face), the patient must be seen by a dentist immediately (Figure 15) to cover the exposed pulp because the vitality of the tooth is in jeopardy, and the length of time that the pulp remains exposed is a critical factor.1

Fractures of the root of the tooth may occur with or without obvious mobility; some root fractures may only be identified on x-ray. A dentist should be consulted as soon as possible. The possibility of preserving the tooth depends on the position, direction, and extent of root fracture. The alternative, in which the entire crown is lost, is a much more serious problem and requires immediate attention by a dentist.
Prevention
Pediatricians can play a primary role in preventing oral or facial injuries by educating young athletes, their parents, and their coaches about the need for using proper protective devices. Head and face protectors (helmets with or without face shields) are available for many sports, and their use should be encouraged.
The use of mouth protectors for all contact sports is highly recommended by the American Dental Association.7,11 This includes but is not limited to football, hockey, lacrosse, basketball, baseball, volleyball, and soccer, to name a few.
Generic mouthguards are available over the counter at sports shops and are designed to be do-it-yourself. By softening the mouthguard material in boiling water and then fitting it to the child’s mouth, the mouthguard can be fabricated by the patient at home. The cost is minimal, although the fit is usually poor, and these mouthguards may cause breathing problems and speech difficulties.
Poorly fitted generic mouthguards provide little if any protection. Also, if the athlete is rendered unconscious, the danger of the mouthguard displacing and lodging in the throat exists. For athletes who are wearing orthodontic appliances, orthodontic versions are available.
The alternative is a custom-fitted mouthguard. This is custom made by a dentist, and so there is additional cost and time involved. However, the fit and comfort are superior, they cause less disruption of speech and breathing, and they usually outlast the generic mouthguards.
In all cases, athletes should be discouraged from wearing removable orthodontic appliances, such as retainers, while engaging in contact sports to minimize the risk of the appliances breaking or becoming dislodged and going down the throat.
Pediatricians who serve as coaches or team doctors should become familiar with the unique risk factors and specific preventive measures required in each specific sport.
Consider, for example, the popular sport of basketball. Many young athletes eagerly try to emulate their professional basketball idols and duplicate the exciting slam-dunk maneuver. This explains the popularity of adjustable-height slam-dunk basketball sets, which allow the athletes to lower the hoops to a height where shorter athletes can now more easily reach them.
Unfortunately, many children annually lose their front teeth on this equipment (Figure 16).
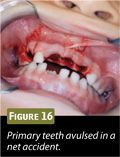
This happens with inexperienced young athletes with poorer dexterity trying to perform a complex maneuver. Mix in a smaller stature, with shorter arms, bringing the children and their faces closer to the net. Now add prominent front teeth, and when the children with open mouths hit the net, the teeth get caught in the net. As the children drop and the spring-loaded hoops recoil, the front teeth are extracted.
One way to avoid these accidents is to use plastic breakaway clips that attach to the basketball hoops. The net is then attached to these clips and not the hoop directly (Figure 17), so that if a child gets entangled in the net, the net is designed to separate from the hoop, thereby minimizing the injury to the child. Of course, one should also take care to wrap the vertical support pole (if any) with a cushioned pad to reduce injuries.

This is just 1 example of the type of recommendations that pediatricians can make to athletes, parents, and coaches for safety with a particular sport. Experience with the individual sports and the particular safety issues of each sport can assist pediatricians in their roles as coaches, team doctors, and team advisors.
Pediatricians who coordinate their efforts with dentists by making timely referrals and who educate young athletes, their families, and coaches about the use of protective aids can do a great deal to help reduce the incidence of sports-related oral or facial injuries.
For more information, go to www.iadt-dentaltrauma.org and dentaltraumaguide.org.
REFERENCES
1. Ellis E III. Soft tissue and dentoalveolar injuries. In: Hupp JR, Ellis E III, Tucker MR. Contemporary Oral and Maxillofacial Surgery. 5th ed. St. Louis, MO: Mosby; 2008:469-492.
2. Flores M, Malmgren B, Andersson L, et al; International Association of Dental Traumatology. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dent Traumatol. 2007;23(4):196-202.
3. Tucker MR, Farrell BB, Farrell BC. Management of temporomandibular disorders. In: Hupp JR, Ellis E III, Tucker MR. Contemporary Oral and Maxillofacial Surgery. 5th ed. St. Louis, MO: Mosby; 2008:629-650.
4. Davies SD, Chung W. Functional disorders of the temporomandibular joint. In: Fonseca RJ, Turvey TA, Marciani RD. Oral and Maxillofacial Surgery. Volume II: Trauma, Surgical Pathology, Temporomandibular Disorders. 2nd ed. St. Louis, MO: Saunders; 2008:898-911.
5. Coletti D, Caccamese Jr. JF. Diagnosis and management of mandible fractures. In: Fonseca RJ, Turvey T, Marciani RD. Oral and Maxillofacial Surgery. Volume II: Trauma, Surgical Pathology, Temporomandibular Disorders. 2nd ed. St. Louis, MO: Saunders Elsevier; 2008:139-161.
6. Ochs MW, Tucker MR. Management of facial fractures. In: Hupp JR, Ellis E III, Tucker MR. Contemporary Oral and Maxillofacial Surgery. 5th ed. St. Louis, MO: Mosby; 2008:493-518.
7. Edward Ellis III. Advances in maxillofacial trauma surgery. In: Fonseca RJ, Walker RV, Betts NJ. Oral and Maxillofacial Trauma. 3rd ed. St. Louis, MO: Elsevier Saunders; 2004:329-376.
8. Manson PN, Forrest CR, Hammer B, et al. Craniofacial fractures. In: Prein J, ed. Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group. Berlin: Springer; 1997:95-154.
9. Posnick JC, Costello BJ, Tiwana PS. Pediatric craniomaxillofacial fracture management. In: Miloro M, Ghali GE, Larsen PE, Waite P. Peterson’s Principles of Oral and Maxillofacial Surgery. 2nd ed. Hamilton: Decker; 2004:527-547.
10. Salin MB, Smith BM. Diagnosis and treatment of midface fractures. In: Fonseca RJ, Walker RV, Betts NJ. Oral and Maxillofacial Trauma. 3rd ed. St Louis, MO: Elsevier Saunders; 2004:643-687.
11. Hutson RK, Christian BA. Diagnostic imaging of facial injuries. In: Fonseca RJ, Turvey TA, Marciani RD. Oral and Maxillofacial Surgery. Volume II: Trauma, Surgical Pathology, Temporomandibular Disorders. 2nd ed. St. Louis, MO: Sanders Elsevier, 2008:91-103.
12. Barber HD, Bahram R, Woodbury SC, Silverstein KE, Fonseca RJ. Mandibular fractures. In: Fonseca RJ, Walker RV, Betts NJ. Oral and Maxillofacial Trauma. 3rd ed. St Louis, MO: Elsevier Saunders; 2004:479-522.
13. Turvey TA, Ruiz RL, Blakey GH III, Biron RT, Levin LM. Management of facial fractures in the growing patient. In: Fonseca RJ, Walker RV, Betts NJ. Oral and Maxillofacial Trauma. 3rd ed. St Louis, MO: Elsevier Saunders; 2004:967-1000.
14. Powers MP, Quereshy FA, Ramsey CA. Diagnosis and management of dentoalveolar injuries. In: Fonseca RJ, Walker RV, Betts NJ. Oral and Maxillofacial Trauma. 3rd ed. St Louis, MO: Elsevier Saunders; 2004:427-478.
15. Tiwana PS, Kushner GM, Alpert B. Cranio-maxillofacial injuries in children. In: Fonseca RJ, Turvey TA, Marciani R. Oral and Maxillofacial Surgery. Volume II: Trauma, Surgical Pathology, Temporomandibular Disorders. 2nd ed. St Louis, MO: Sanders Elsevier, 2008:352-373.
16. Andreasen JO, Bakland LK, Flores MT, Andreasen FM, Andersson L. Traumatic Dental Injuries. A Manual. 3rd ed. Copenhagen: Wiley-Blackwell; 2011.
17. Choi D, Badner VM, Yeroshalmi F, Margulis KS, Dougherty NJ, Kreiner-Litt G. Dental trauma management by New York City school nurses. J Dent Child (Chic). 2012;79(2):74-78.