Overcoming ALTEphobia: A rational approach to "spells" in infants
The baby who suffers a "spell" marked by apnea, choking, or color changes presents a frightening dilemma: Is it an apparent life-threatening event (ALTE) or something less serious? The author offers detailed advice on how to evaluate spells and follow up if necessary. First of two parts.
Cover story
Overcoming ALTEphobia: A rational approach to "spells" ininfants
By Sean Palfrey, MD
The baby who suffers a "spell" marked by apnea,choking, or color changes presents a frightening dilemma: Is it an apparentlife-threatening event (ALTE) or something less serious? The author offersdetailed advice on how to evaluate spells and follow up if necessary. Firstof two parts.
Trying to figure out whether or not a "spell" reported by thefrightened parents of an infant was really life-threatening is one of thehardest, most anxiety-provoking diagnostic dilemmas that a primary carepediatrician faces. Deciding what to do about a worrisome event is almostas difficult. Both parents and pediatricians generally overreact to chokingspells, apnea, and transient color changes that occur in normal babies--aphenomenon that I call ALTEphobia, fear of apparent life-threatening events.
Sudden infant death syndrome (SIDS) is the specter that everyone fears.By definition, it refers to the sudden, unexpected death of an infant, thecause of which remains unknown even after full death-site and postmortemevaluations. Of the fewer than one in 1,000 infants who die of SIDS in thiscountry, only a very small number have "warning" spells of anykind. Yet spells are common.
Almost none of the children who have spells ever go on to die, and sincewe do not understand the causes of SIDS, we have no tests that can identifythe tiny subset of children who do. Moreover, no statistical evidence existsto suggest that any of our interventions, including home monitoring, havechanged the incidence of SIDS deaths. All we have is the feeling that ifsomeone had not been alerted to certain events, and intervened quickly,particular infants might have died.
Thus, our tasks when faced with spells are much the same as when we encounterany other worrisome sign or symptom: first, to identify any pathologic elementsand second, to decide if treatment is warranted. Obviously, seizures, chokingspells, prolonged apnea, and bradycardia can have serious consequences,and we need to evaluate and treat them carefully. But these events are almostnever precursors to SIDS, and it is very important to be clear with ourselvesand with parents about this fact.
My purpose here is to offer a balanced approach to evaluating, managing,and following up various types of spells that infants may have in the firstyear of life. It is presented in two parts. This article discusses the natureof certain spells, guidelines for rational assessment, criteria for undertakingfurther work-up, and studies that could be performed. The second part willdiscuss interpretation of study results and management of infants who havehad spells.
What are "spells"?
Parents and other untrained observers may become very upset by variationsin breathing patterns, color, and muscle tone of babies in their care. Fewspells in infancy are truly ALTEs, however. Our first step, when faced witha concerned caretaker, is to dissect out of the story the few key elementsthat are medically meaningful and to reassure the family about the rest.
Successful cardiorespiratory control results from a sequence of finelytuned feedback mechanisms, both peripheral and central. These control loopsincorporate a great deal of physiologic redundancy and wide safety margins.Almost anything can happen to most children, and they will still be ableto overcome the problem. It is our task to differentiate truly worrisomeevents from commonplace ones.
We need to follow up children who have had events involving prolongedapnea, cyanosis, and changes in alertness and tone, but the stories we hearare often vague or confusing. On the phone or in the office, several initialquestions provide clues to the type of event: Was the baby asleep or awake?Trying to breathe or not? Normal color or red, pale, or blue? Able to recoverfully right after the event or not?
We should attempt to establish the duration of the event and whetherthe infant actually needed the stimulation given, but these are often difficultto gauge accurately. If the baby appeared to be choking, we need to documentthe spell's temporal relationship to feeding or vomiting. Based on theseelements of history, and our knowledge of normal and abnormal patterns ofbreathing, heart rate, and circulation, we can usually gain, even from themost sketchy of stories, some sense of whether or not a baby was in realdanger.
Central apnea spells
All babies have some central apnea, and parents are often frightenedbecause even short spells seem to last so long. In general, however, weare less concerned about the duration or frequency of apnea than we areabout associated signs of physiologic distress such as bradycardia or desaturation.
Duration of central apnea. We consider most "short" apnea,lasting up to 15 seconds, to be within normal limits. "Prolonged"central apnea is defined in relation to age. Normal infants youngerthan6 to 9 months occasionally have apnea longer than 15 seconds, but it isnot uncommon for older children to have central apnea spells lasting 25seconds or more without any apparent physiologic distress.
Babies who have mildly prolonged central apnea for age, yet tolerateit without difficulty, may be perfectly healthy. Those who have apnea lastingmore than 10 seconds longer than expected, or who have significant bradycardiaor cyanosis during central apnea of any duration, should be considered abnormaland possibly at risk for a serious hypoxic event. The brains of certainchildren do not always generate the appropriate signals to inspire, andserious events can result from otherwise minor stresses, such as viral infectionsand choking spells. These babies may not be able to respond adequately tohypoxia, hypercarbia, acidosis, or even stressful changes in body position.
Frequency. Some babies have lots of short central apnea. This usuallyreflects immature central respiratory control or an ongoing viral infection.Babies mature out of this pattern, and it should be considered of littlephysiologic concern unless associated with bradycardia or desaturation.Certain babies are at special risk, however, including those with bronchopulmonarydysplasia (BPD), congenital heart disease, or spina bifida. They must bewatched carefully for apnea, especially during respiratory illnesses, becausethey are at much greater risk of serious problems during these periods.
Periodic breathing. Short central apnea can occur in a rhythmic, repetitivepattern called "periodic breathing." This pattern almost alwaysoccurs during sleep, unless the baby has a central nervous system abnormalityor infection, and consists of bursts of a few normal breaths separated byperiods of short central apnea usually lasting six to 12 seconds. Periodicbreathing may go on for two or three of these cycles or for many minutes.
Periodic breathing, like short central apnea, reflects immature centralrespiratory control. Preemies may spend 10% to 15% of sleep time breathingthis way. Most term babies spend 1% to 4% of sleep time breathing this way,and the pattern tends to disappear over the first one to four months oflife. Viral and other CNS infections transiently increase the percentageof periodic breathing just as they increase the frequency and duration ofshort central apnea. Periodic breathing is rarely of concern unless thebaby becomes progressively more desaturated as the pattern continues. Ifthis happens, the cause of the prolonged runs of periodic breathing andthe reason the baby desaturates so easily should be investigated.
Obstructive apnea spells
Obstructive apnea represents a normal defense mechanism and occurs wheneveranyone tries to breathe against an obstruction. Air movement may be blockedby extraneous material, the baby's own soft tissues, or reflex laryngospasm.
During obstructive apnea, the baby actively tries to breathe but is transientlyunsuccessful. Usually, you can see the respiratory effort, but sometimesthe baby appears to be caught in inspiration, unable to move air. If theobstruction is significant, the baby will be awake and may appear scared,with eyes open and body tense.
As with central apnea, the incidence of obstructive apnea is relatedin various ways to age and development. Infants are obligate nose breathersfor their first several months, for example, with small, floppy airwaysand immature muscle tone. Relatively small amounts of material in the wrongplaces can produce noisy, momentary obstruction, even in normal babies,and these can be scary events. Soft tissues in the nose, around the softpalate, and at the back of the tongue intermittently narrow the airways,causing much of the "rattley" breathing heard in infants.
Premature infants, who have poor tone and relatively weak muscles, canexperience serious airway obstruction when slumped in a semi-upright position,as in a car seat. For this reason, many nurseries place such infants inthe car seats they are to go home in for a couple of hours before departureto make sure that they can maintain good saturations in the semi-uprightposition. Children with hypotonia or macroglossia also may be at increasedrisk for obstructive apnea and should be carefully checked.
Gastroesophageal (GE) reflux is one of several common, normal eventsoften blamed for choking spells. It can cause spells by two different mechanisms:direct obstruction of the airway by refluxed stomach contents and reflexlaryngospasm.
Reflex laryngospasm is really a protective mechanism, and in some instancesis referred to as the "diver's reflex." Fluids such as stomachcontents, formula, and even water can stimulate receptors widely distributedin the oropharynx, trachea, larynx, and esophagus. This neurologic reflexcauses the larynx to close, preventing foreign material from getting intothe lungs. A child who has chronic reflux may also develop esophagitis.When this happens, the esophageal receptors become sensitized, or "twitchy,"and the infant may have laryngospasm without obvious reflux.
Obstructive apnea may be normal and benign, as when it is associatedwith colds, mild laryngomalacia, or minor choking spells. In two situations,however, it is cause for real concern. First, if a baby has very frequentchoking spells, we should ask why they are happening so often. Does he havean anatomic obstruction, hypotonia, recurrent GE reflux, excessive reflexlaryngospasm caused by esophagitis, or seizures?These circumstances rarelythreaten the baby's life but, for his general well-being, they should beinvestigated and the underlying causesaddressed.
Much more serious is the rare situation in which a baby either cannotsense or respond to hypoxia or hypercarbia or truly cannot overcome theobstruction by himself. In these cases, we need to search extensively forthe etiology of the problem. Causes may include dysfunction of central orperipheral O2, CO2, or pH sensory reflexes, serioushypotonia, a poor gag reflex, dysfunctional swallowing, or decreased abilityto clear secretions. These conditions must be taken very seriously and treatedto whatever degree possible.
Mixed apnea spells
Mixed apnea spells contain periods of both central and obstructive apneaand occur commonly. Usually both components are short, and the baby toleratesthe event without difficulty.
Occasionally, the combination can lead to desaturation and bradycardia.If significant cyanosis results, or the baby requires active stimulation,we should investigate both the central and obstructive components and attemptto determine why the baby is unable to sustain good saturations and heartrate.
The colors of spells
Spells can be accompanied by reassuring color changes, such as rednessor flushing, or worrisome color changes, such as pallor or cyanosis.
Transient redness is reassuring because it usually reflects effort andperfusion with well-oxygenated blood. Obvious exceptions include high feversor exposure to carbon monoxide.
Transient pallor is less easy to interpret. In the first few months oflife, it may reflect generalized hypoxia, and the cause should be investigated.After that age, pallor usually suggests anemia or local hypoperfusion causedby cold or volume depletion.
Transient cyanosis suggests that the baby is oxygenating the cyanoticpart of the body poorly, either because of local vasoconstriction or perfusionwith poorly oxygenated blood. Peripheral cyanosis, like obstructive apnea,may be a protective mechanism, caused by cold or dehydration, for example.Central cyanosis probably reflects cardiovascular or pulmonary disease,and suggests shunting. Recurrent or prolonged cyanosis should be evaluatedand the causes treated if possible.
Spells with abnormal tone
Changes in muscle tone during a spell may point to a variety of problemsdepending on whether the baby becomes hypotonic or hypertonic.
Hypotonia of relatively acute onset can reflect many problems. Theseinclude sepsis, dehydration, drug exposure, seizure or postictal states,and neurologic devastation caused by hypoxia.
Hypertonia of relatively acute onset may reflect muscular effort, suchas that required to overcome obstruction, or a change in overall tone causedby seizures, meningitis, encephalopathy, or even the esophagitis of Sandifer'ssyndrome. Almost all of these serious conditions are associated with persistenceof abnormal tone, yet most of the babies we examine minutes after a spellappear normal. A seizure is usually the most difficult event to rule outas the cause of a transient episode of altered tone. Outside the immediateneonatal period, however, when subtle changes in respiratory pattern ortone may be the only manifestations of a seizure, seizures usually includetypical motor, tone, and mental status changes--patterns that parents oftencan describe.
Spells with abnormal motor activity
Babies often shake, and most forms of shaking are benign. A baby whois choking may stiffen and make repetitive arching or gasping motions. Ababy who is hungry and a little hypoglycemic, or simply irritable, may showfine shaking motions of the arms or legs.
Myoclonus can be either benign or seizure-related. If the baby's movementsare rhythmic and jerky, they may represent seizure activity.
Evaluating a "spell"
Evaluating spells requires answering three fundamental questions: Wasit an ALTE or not? If yes, why did it happen, and can we prevent it fromhappening again? If no, do we need to do anything at all? Since very few"spells" are truly life-threatening, yet many appear frighteningto parents and caretakers, the physician's first task is to assess the infant'scurrent clinical status, either over the phone or directly in the officeor emergency department.
In the process of establishing the patency of the airway, adequacy ofbreathing, heart rate (if possible), skin color, alertness, tone, and movement,we can calm and reassure the family and ourselves that the baby's basicfunctions are stable at the moment. Then, depending on the answers to severalquestions about the spell, the baby, and the state of the parents, we candetermine where, when, and even if we want to see the baby.
A pertinent, appropriately detailed history is the centerpiece of theevaluation of spells and often supplies most of the information we needto judge the etiology and severity of the event. It is important to remaincalm, disciplined, and focused at every step. Otherwise the work-up willspiral out of control, becoming prolonged and needlessly worrisome for parents.
First, we must attempt to establish the elements of the spell, theirseverity, and duration. In order to do this, we need to ask a series ofspecific questions and help the caretakers clarify their own memories ofwhat happened. Based on this information and our clinical judgment, we thenhave to decide whether the event was life-threatening and if not, whethersimilar events are likely to be. This determination will drive our investigationinto possible etiologies.
History of the acute event
A history of the spell itself should include the following questions:
Why did you check the baby at the moment of the spell? Did the baby cryout or make an unusual sound? Was she vomiting or thrashing? Was she unusuallyquiet? Was she simply being fed? The answers to these questions can provideclues that may help define what was happening before the caretakers observedthe baby having the spell.
Was the baby asleep or awake? This question helps to differentiate centralfrom obstructive apnea and suggests causes. Most significant central apneaoccurs during sleep, and almost never wakes the baby, unless the child hasmeningitis, sepsis, seizures, or an uncommon combination of factors (suchas a child with spina bifida who has respiratory syncytial virus). Mostserious episodes of obstructive apnea wake the infant.
Was the baby trying to breathe? During most central apnea episodes, norespiratory effort is seen. During serious obstructive apnea, the baby usuallyappears to be at least trying to breathe, seems scared, and has increasedmuscle tone.
Where was baby when the episode occurred? The baby's body position andplace in a crib, infant seat, or the parent's arms as well as the descriptionof objects around the baby--such as pillows, quilts, bean bags, and stuffedanimals--may suggest or argue against obstructive apnea.
Was the baby dusky, pale, red, or normal in color, and could he be seenwell enough to tell? The baby's color offers many important clues, but itis essential to establish that there was enough light to see it accurately.We must also find out what parts of the baby could actually be seen, sincelocalized cyanosis may have very different causes from full, central cyanosis.
Did the baby come out of the spell by herself, need stimulation, or needvigorous resuscitation? The importance of this question is self-evident,but the answer may take a great deal of skill to interpret. If the babydid not need stimulation, how long did it take her to return to a completelynormal state, and what were the steps in that process (was she sleepy, limp,pale, wheezy)? If the baby was stimulated, would the physician have feltthe need to stimulate her given what the parents described as her condition,and what does the doctor believe were the truly necessary actions? (Wasmouth to mouth resuscitation needed, for example?)
Were there unusual elements to the spell? Questions such as, "Wasthe baby lying in an odd position? Moving in a weird way? 'Awake' but unresponsive?"can offer clues to conditions such as altered neurologic status or seizures.
After the spell, did the baby appear completely normal? This is a criticalquestion, because if the answer is Yes, it makes serious acute illnesses,metabolic disorders, CNS trauma, even seizures unlikely and narrows thedifferential diagnosis considerably. It is important, however, that thereturn to normalcy be fairly rapid. Otherwise, factors such as significant,though transient, hypoxia caused by the spell could remain undiscovered.
Do witnesses have differing stories about important elements? Does thestory add up? Discrepancies in the history may be important and may suggestchild abuse. Minor discrepancies in an otherwise simple story, however,may be caused by poor lighting, anxiety, or limitations of the reporter,and certain clinical scenarios may indeed be difficult to figure out.
How upset are the parents? The answer to this question has implicationsboth for the interpretation of the history the parents give and the careand support we need to offer them during their child's evaluation.
Medical history
Most babies who present with a spell have been healthy and have veryshort past medical histories, but basic questions relating to pregnancy,birth, and specific organ system functions should be asked because theycan provide explanations for benign as well as serious spells. This is thefirst pass, and we are looking for common conditions that could explainor predispose infants to acute and transient episodes of apnea, bradycardia,desaturation, choking, seizures, or changes in muscle tone. Later, if wecannot find an explanation for life-threatening events, we will have toundertake more detailed questioning. Appropriate initial questions include:
- Did the baby's mother have any known infections (rubella, cytomegalovirus, toxoplasmosis), metabolic diseases (thyroid disease or diabetes), or neurologic problems such as seizures during her pregnancy? Was she taking any medications?
- Was the baby born prematurely? Did he have any deformities, such as a meningomyelocele? Did he have immature lungs, require assisted ventilation, need oxygen, have bronchopulmonary dysplasia? Did he have apnea, bradycardia, frequent desaturations? Did he have seizures or an intraventricular bleed?
- GI: Is the baby very spitty? Does he choke when he vomits? Has he been diagnosed as having GE reflux, constipation, or formula intolerance?
- Cardiac: Does the baby have a heart murmur or any known heart problem?
- Pulmonary: Has the baby had a chronic cough or bouts of pneumonia or bronchiolitis? Is he coming down with a cold?
- Neurologic: Has he had meningitis or seizures? Does he have significant developmental delays, hyper- or hypotonia?
- Has the baby grown normally? Does he have problems with immunity? Is he a difficult baby to take care of--is he "bad"?
If these questions turn up a medical diagnosis that explains the spell,we should be concerned not about SIDS but about the known illness and respondaccordingly.
Family history
The family history should focus on genetic and environmental entitiesthat increase the chances of spell-like events in infants. These includeepilepsy or certain forms of chronic neurologic or neuromuscular diseasesand syncope (possibly caused by prolonged QT syndrome) or sudden cardiacdeath (possibly resulting from a genetic predisposition to heart disease).Cigarette smoking and illicit drug use increase the risk of SIDS slightly,but we cannot predict which children are at particular risk. A family historyof serious child abuse or removal of children from the parents for unknownreasons alerts us to psychosocial problems as possible causes of spellsand also difficulties with treatment compliance.
It is obviously important to ask if children in the immediate familyhave died suddenly without explanation. Although it is very unusual formore than one child in the same family to die of SIDS, the specter causesmassive anxiety, so that pediatricians often hear about every color changeand choking spell. Since the chance a second child will die of SIDS is actuallylittle greater than that in the general population, we must keep our medicaltasks in focus, but we must also work with particular care and sensitivitywith such a family in addressing any episode they find scary.
Discovering that several first degree relatives have died inexplicablyin infancy, or even suddenly at an older age of unknown causes, greatlyincreases the chance that a potentially fatal familial disorder exists orthat homicide has occurred. Such situations require much more detailed,far-reaching investigations and often the input of geneticists, immunologists,and social workers.
Questions relating to family history and recurrent SIDS often increaseparents' anxiety and guilt. We need to point out that the absence of eachcondition we discuss is reassuring and that we know the risks familial diseasespose and can address them. It is only multiple unexplained deaths in a familythat place a child at truly high risk.
The physical examination
The physical examination should focus on finding anatomic or physiologicexplanations for the spell. Pay special attention to the neurologic examination,including altered responsiveness, increased or decreased tone and strength,and difficulties in swallowing or handling secretions. Examine the noseand oropharynx carefully for possible causes of obstruction. Check the heartand lungs for evidence of lung disease or previously undetected cardiacdisease. Look for signs of acute infection, such as a fever and evidenceof pneumonia, meningitis, Shigella, and other infections.
If the physical exam turns up abnormalities that might explain the spell,they should obviously be evaluated in depth. Most of the time, however,infants appear well by the time we see them, and we have to proceed on thebasis of our degree of clinical concern about the spell and clues we haveturned up in the history.
Planning the workup after the initial evaluation
We must first decide whether or not the event was truly life-threatening.Did it require vigorous intervention to reverse, or is there any evidence,based on history and clinical judgment, of an ongoing life-threatening process?Episodes of choking, apnea, or dusky color that resolve by themselves orafter minor stimulation are, by definition, not life-threatening or associatedwith an increased risk for SIDS. Serious systemic diseases may produce worrisomeevents, but they are almost always accompanied by persisting abnormalitiesor clues in the history or physical exam.
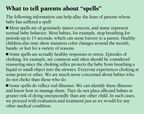
If, in our judgment, the baby does not have a life-threatening conditionand looks clinically well, he can be sent home to be followed and workedup as needed on an outpatient basis. It is very important, however, to informand educate the infant's parents about what we think happened. Some needlittle reassurance while others need a great deal. It depends on their levelof anxiety and the nature of the event. The information found in the box,"What to tell parents about 'spells'" may be helpful. The informationfound in the box, "What to tell parents about SIDS" may help parentswho are especially concerned about SIDS.

If we feel that the event had worrisome features that warrant evaluationand might be preventable, we have to decide whether the baby can be workedup quickly and safely as an outpatient (as in the case of a baby with refluxand significant choking) or requires admission for monitoring during thework-up (as in the case of an infant with possible seizures). Table 1 listsguidelines for deciding which tests to perform.

If we feel that the event reported was life-threatening or might reflecta life-threatening condition, we admit the baby for observation, monitoring,and possibly antimicrobial therapy pending culture results.
Evaluating specific abnormalities
If the baby was not completely normal before the episode and did notreturn to a completely normal state afterwards or was febrile or lethargic,he should obviously be worked up for sepsis, meningitis, encephalitis, headtrauma, metabolic disease (such as hypoglycemia), or whatever else seemsmedically appropriate.
If the baby had a truly serious event, which probably included apnea,bradycardia, or desaturation, yet looks well after the spell, consider theapproach outlined in Table 2.

The multichannel study
A multichannel study--sometimes called a sleep study, pneumogram, orpolysomnogram--monitors respiratory effort, heart rate, and one or moreof the following physiologic functions: airflow at the nose, oxygen saturation,and esophageal pH. In sleep centers, simultaneous electroencephalogram (EEG)and electromyelogram recordings may be performed, but I will not discussthem in detail.
Multichannel studies are usually run for 12 hours, but if the baby hashad episodes at least once a day, the test can be run until an episode occurs.Typically, the study is done overnight, especially if you are looking forcentral apnea, which usually happens during sleep. If you are trying todocument obstructive apnea or reflux, however, the child should be studiedwhen the episodes seem most likely to happen.
All channels must be recorded and printed simultaneously. Accurate timemarkers should be included so that whenever an event is noted clinically,the corresponding patterns can be identified precisely on the recordings.
Choose the channels carefully. We always want to know heart rate andrespiratory effort, but alone--without saturation data, for instance--thesetwo channels offer too little information. For this reason, there are essentiallyno indications for ordering a two-channel "pneumogram" (respiratoryeffort and heart rate only).
Multichannel studies are expensive. Don't do one if you intend to ignorethe results or have decided to manage the infant in a specific way regardlessof result. Some insurance companies require a two-channel pneumogram beforethey will pay for home monitoring. Some even require that the study takeplace in a hospital. These are very illogical approaches. It is importantthat we all try to educate insurance companies and advocate that they incorporatemedical reasoning into their regulations.
Make sure that you find an expert whose clinical judgment you trust todiscuss cases with you, read your studies, and interpret them using theclinical data you have assembled. My own recommendations are almost alwaysbased more on the information I gain from discussing the case with the infant'sphysician than on data I find on studies.
What typical channels can and cannot tell you
Therespiratory effort tracing is usually recorded by an impedance method,which measures chest wall (and occasionally abdominal) motion. The primaryproblem with this method is that babies sometimes breathe very shallowly,especially during deep sleep. Very shallow breathing is sometimes difficultto distinguish, clinically as well as on paper, from central apnea. If thebaby's simultaneous heart rate and saturations remain normal, however, heis probably moving O2 and CO2 well, just as we hopeoccurs when we administer high-frequency ventilation.
Problems also arise when vigorous body motion obscures respiratory patterns,making it difficult to tell whether obstructed breaths are hidden underthe movement artifacts. Other deflections, such as heart beats, occasionallyshow up on impedance tracings, but by analyzing the rate of these waves,one can usually tell cardiac coincidence, as it is called, from rapid, shallowbreaths.
Theheart rate tracing is created by recording a simple ECG, calculatinga rate from each R-R interval, and printing it as a continuous tracing.The primary problems with this "channel" are lead placement andmotion artifact, which can distort the ECG so much that the calculated heartrates look like tachycardia or bradycardia. It is usually easy to guessthat the extremes are artifactual but often difficult to tell if there isa real heart rate drop during movement artifact.
Theoximetry tracing is the usual method of measuring oxygenation in thiscountry. Its advantages are that it is very easy to perform, noninvasive,and usually reflects systemic O2 saturation. Its primary disadvantagesare that any kind of motion, even that seen in choking, can cause uninterpretableartifact. Similarly, poor peripheral circulation, caused by vasoconstrictionor dehydration, will cause the tracing to register lower than core saturations.This channel, however, can be very useful in determining how well a babyis able to maintain saturation during central apnea, hypoventilation, bradycardia,and various potentially stressful conditions.
The oximetry reading is paired with a simultaneous pulse rate tracing(hence "pulse oximetry"). When the oximeter registers a heartrate identical to that of the ECG, the saturation reading is usually accurate.When it does not, the reading is almost always so wrong that it is uninterpretable.
Transcutaneous pO2 measurements are often used in neonatalintensive care units and are not affected by motion. Because they heat theskin up in order to work, however, their position has to be changed everyfour to eight hours. Also, they become less sensitive as skin thicknessincreases. For these reasons, they are rarely used in this country for 12-or 24-hour sleep studies.
Thenasal air flow tracing is the method most commonly used to reflectupper airway air movement, thus allowing us to tell if a child is tryingto breathe but not moving any air (obstructed). It relies on nasal thermistry,the temperature of the air moving in and out of the nose, to show air movement.
Infants in the first few months of life are obligate nose breathers,and if the baby allows the sensor to stay in place, nasal thermistry givesa good indication of air flow. Whenever the baby breathes through his mouth,however, the tracing looks like obstructive apnea (lots of respiratory effortin the impedance channel and no air movement in the airflow channel) whenin fact the baby is breathing very effectively. Also, nasal thermistersare annoying and rather easily dislodged, so unless someone is watchingthe probe position, it can move and generate useless or misleading tracings.
A much more informative method of studying upper airway movement, end-tidalCO2 measurement, is more expensive, a little more invasive, andnot readily available in many parts of the country. It provides a breath-to-breathreflection of CO2 exchange, indicating the sufficiency of airmovement. Although this method does not quantify airflow, when combinedwith oximetry it provides important physiologic information about the baby'scondition at the moment. It should be universally available for use whenthe adequacy of an infant's ability to move air is in serious question.
A note on motion artifact: Whenever there is lots of body movement, asduring an obstructive event, none of the channels discussed so far is reliable.It is important for clinicians to understand that events may be missed underthese conditions.
Theesophageal pH tracing relies on accurate placement of the pH probe.It should be in the mid-esophagus, not so low that it dips into the stomachinadvertently, high enough that it reflects reflux partway up the esophagus,and not so high that the baby can dislodge it with little effort.
The pH channel tells us how many times a baby refluxes to the level ofthe probe and how long the refluxed acid remains in the esophagus beforebeing swallowed. Combined with simultaneous heart rate, saturation, andrespiratory tracings, a pH probe study will demonstrate any temporal relationshipbetween episodes of reflux and obstructive apnea, bradycardia, or desaturation.
The accuracy of pH tracings depends on several things. A pH of 4 or lessis considered to reflect the presence of stomach acid in the esophagus,but this is correct only if the baby has acid material in the stomach. Newbornsmay not have very acidic stomach contents for days or even weeks after birth,so reflux events are often missed at this age. Food neutralizes stomachacid, so pH probes may not document reflux events during feedings. It hasbeen estimated that less than half of reflux events in babies are associatedwith drops in esophageal pH to below 4, so the interpreting physician mustconsider the importance of even subtle pH changes if obstructive apnea spellsaretemporally related.
Esophageal pH probes may also miss episodes of vomiting because theseepisodes happen so quickly and clear the esophagus of material so effectivelythat there will be little or no deflection in the pH tracing. Finally, pHprobes require accurate calibration. They must be checked at the start ofevery study and remain in calibration throughout the 12 hours of the study,or else pH 4 becomes worthless as a benchmark.
It is surprising that reflux is so rarely "caught" producingobstructive apnea, even when there are many episodes of each. In fact, weoften see what looks like coughing or choking before reflux, presumablybecause the changes in relative pressures between the abdomen and chestassociated with choking more often cause reflux than the reverse. This factunderscores the importance of recording pH probe studies on the same equipmentas the other channels so that exact temporal relationships can be analyzed.
Blood, urine, and spinal fluid studies
Blood studies should be performed only if there are specific indications.If the baby has returned to a completely normal state after the event, asmost do, blood studies are unlikely to be helpful. If the history or physicalexam suggests infection, sepsis, or meningitis, these should obviously beinvestigated with a complete blood count and appropriate cultures. Sometimes,if a spell has been truly stressful, the white blood cell count is elevatedwith demarginated polys, but there is no source of infection. A significantincrease in bands would be unusual, however, and should be followed up.
Infants, particularly premature infants, who are seriously anemic aremore likely to have central apnea than those with normal hemoglobins. Ifyou believe that the baby has symptoms or signs of anemia or known riskfactors, perform a hemoglobin (or CBC). If the baby has a history of spellsafter fasting or appears listless or jittery, a blood sugar should be done.Occasionally occult infections, such as urinary tract infections or earlyviral infections, can cause apnea, but these should not be pursued unlesssuspicions arise from the history or physical exam. If serious spells runin the family, a much more involved work-up may be needed.
The ECG
In the absence of an abnormal cardiac exam or resting desaturation, itis unlikely that a congenital heart defect is the cause of a transient cyanoticor apneic episode. Tachyarrhythmias, such as supraventricular tachycardia,can cause congestive heart failure, but this usually develops graduallyin infants, and cyanosis from this cause does not appear and disappear abruptlyin association with the tachycardia.
Prolonged QT syndrome can cause sudden and serious dysrhythmias. It israre, runs in families, and is unlikely to be associated with central orobstructive apnea. If we have a clear reason to suspect prolonged QT syndrome,however, it can be evaluated with a standard ECG.
Premature infants sometimes have bradycardic spells associated with transientduskiness, especially during swallowing or apnea. These are rarely "caught"on standard ECGs and are much more commonly found, and better evaluated,by 12-hour sleep studies.
If we hear an irregular heart beat or see little repetitive deflectionson the heart-rate channel of a sleep study, these findings can reflect prematurebeats. Transient "spells" related to them are rare, but they shouldbe evaluated with a standard ECG.
The EEG
Apnea or tone and color changes may be the only obvious manifestationsof seizures, especially during the first month or so of life. After twoor three months of age, some motor activity is usually present as well.If you seriously suspect seizure activity, perform an EEG. If significantapnea or cyanosis occurred during the motor or tone changes, an EEG shouldbe performed in a sleep lab where the other channels discussed above canbe recorded simultaneously.
A postictal period is common after a seizure, but infants who have hadserious nonseizure spells sometimes appear sleepy immediately afterwardsas well. These babies usually have normal EEGs or nonspecific slowing andgo on to be completely normal, but they warrant neurologic evaluation andan EEG.
Barium swallow and chest X-ray
GE reflux is a common concern when a baby has a serious obstructive episode,but a barium swallow is not as informative as a pH probe study, unless youthink that the baby might have an obstruction, an anomaly, or abnormal esophagealmotility. In these cases, be sure to specify an upper GI series or a swallowingstudy (fluoroscopy), to assure that you get the information you need.
Even in the presence of GE reflux, aspiration pneumonia is rare, andif it is present, the baby
should have some pulmonary symptoms when examined after the episode. Mostcauses of right to left shunting resulting from cardiac or vascular anomaliesare more effectively documented by an echocardiogram than by chest X-rays.
Looking ahead
If the initial evaluation of an infant who has had a "spell"suggests issues of serious concern, we must proceed with a thoughtful, stepwisework-up. The second part of this article will discuss how to interpret theresults of the work-up and make subsequent management decisions.
THE AUTHOR is Clinical Professor of Pediatrics at Boston UniversitySchool of Medicine and Attending Pediatrician at Boston Medical Center,Boston.
The author gratefully acknowledges the support of Judith S. Palfrey,MD, without whose urging this article would never have been written, andthe
advice and counsel of Michael J. Corwin, MD.
SUGGESTED READING
Filiano JJ, Kinney HC: Sudden infant death syndrome and brainstem research.Pediatr Ann 1995;24:379
Freed GE, Steinschneider A, Glassman M, et al: Sudden infant death syndromeprevention and an understanding of selected clinical issues. Pediatr ClinNorth Am 1994;41(5):967
Garg M, Kurzner SI, Bautista DB, et al: Clinically unsuspected hypoxiaduring sleep and feeding in bronchopulmonary dysplasia. Pediatrics 1988;81:635
Gibson E, Spinner S, Cullen JA, et al: (1996) Documented home apnea monitoring:Effect on compliance, duration of monitoring, and validation of alarm reporting.Clin Pediatr 1996;35(10):505
Hunt CE, Beckerman RC, Brouillette RT, (eds): Respiratory Control Disordersin Infants and Children. Baltimore, Williams & Wilkins, 1992
Hunt CE, Hufford DR, Bourguignon C, et al: Home documented monitoringof cardiorespiratory pattern and oxygen saturation in healthy infants. PediatrRes 1996;39(2):216
Keens TG, Ward SL: Apnea spells, sudden death, and the role of the apneamonitor. Pediatr Clin North Am 1993;40(5):897
Meny RG, Carroll JL, Carbone MT, et al: Cardiorespiratory recordingsfrom infants dying suddenly and unexpectedly at home. Pediatrics 1994;93(1):44
National Institutes of Health Consensus Development Conference on InfantileApnea and Home Monitoring: Consensus statement. Pediatrics 1987;79(2):292
Schwartz PJ, Southall DP, Valdes-Dapena M: The sudden infant death syndrome:Cardiac and respiratory mechanisms and interventions. Ann NY Acad Sci 1986;533:1
Southall DP, Plunkett MC, Banks MW, et al: Covert video recordings oflife-threatening child abuse: Lessons for child protection. Pediatrics 1997;1OO(5):735
Southall DP, Richards JM, Rhoden KJ, et al: Prolonged apnea and cardiacarrhythmias in infants discharged from neonatal intensive care units: Failureto predict an increased risk for sudden infant death. Pediatrics 1982;70:844
Artificial intelligence improves congenital heart defect detection on prenatal ultrasounds
January 31st 2025AI-assisted software improves clinicians' detection of congenital heart defects in prenatal ultrasounds, enhancing accuracy, confidence, and speed, according to a study presented at SMFM's Annual Pregnancy Meeting.