Pediatric nonalcoholic fatty liver disease
Nonalcoholic fatty liver disease (NAFLD) in children is increasing, with studies showing it to be the most common liver abnormality in children aged 2 to 19 years.
Reviewed by Gary L Freed, MD, MPH
Nonalcoholic fatty liver disease (NAFLD) in children is increasing, with studies showing it to be the most common liver abnormality in children aged 2 to 19 years.1 Prevalence of the disease in children and adolescents is difficult to determine given that a definitive diagnosis requires a liver biopsy and the lack of screening guidelines for pediatric NAFLD. However, a landmark study that examined the incidence of disease in 742 autopsy specimens of children who had died of an accident found that 17.3% of the children aged 15 to 19 years had the disease.2,3 This same study showed that NAFLD was more common in boys than girls and in children of Asian descent (10.2%) and Hispanic (mostly Mexican) descent (11.8%), with the lowest rate in African Americans (1.5%), findings that have been confirmed in other studies.
The growing obesity epidemic is believed to be a main driver in the increase of pediatric NAFLD, with studies indicating that about half of obese children may have fatty liver.1 Additional data show that overweight and obese adolescents have 4.14 and 5.98 times, respectively, the risk of NAFLD compared with adolescents of normal weight.
The need for improved diagnosis and treatment of NAFLD in children is highlighted by the multiple complications these children are at high risk of developing, including atherosclerosis and other cardiovascular complications and increased carotid intima media thickness.4 Although prospective data are scarce on the long-term consequences of NAFLD in children, a retrospective study of 66 children with NAFLD followed for 20 years showed that 4 developed type 2 diabetes, 2 underwent liver transplantation, and 2 died of cirrhosis.
Primary care physicians and other health care professionals on the front lines of care can play an important role in identifying children and adolescents with or at risk for developing NAFLD. This review article offers a brief primer on what is currently known about pediatric NAFLD, and provides information on the current understanding of its unique pathophysiology compared with adult NAFLD and current diagnostic and treatment approaches.
Natural history
Nonalcoholic fatty liver disease is defined as the presence of macrovesicular steatosis in greater than 5% of hepatocytes in the absence of significant consumption of alcohol, drugs, or other recognized disorders that may result in fatty liver.2 It includes diseases that range in severity from simple steatosis to nonalcoholic stateohepatitis (NASH). Compared with NASH, simple steatosis has a benign prognosis and is characterized by the accumulation of liver fat without apparent inflammation. In contrast, NASH involves inflammation of the liver and hepatocellular damage that can progress to cirrhosis.2,4
Two types of NASH have been described, 1 associated with adults and the other with pediatrics.4 Type 1 (adult) NASH is characterized by steatosis, hepatocyte ballooning, Mallory hyaline, and pericellular/sinusoidal fibrosis, most with distinct centrilobular distribution. Type 2 (pediatric) NASH is characterized by portal-based fibrosis sometimes associated with portal inflammation and without centrilobular distribution, and more strongly linked to Hispanic and Asian backgrounds and male sex. Studies have shown that 32% to 83% of children have features of both types.4-6
Pathogenesis
Although the pathogenesis of fatty liver in children and adolescents is not fully understood, overnutrition and a sedentary lifestyle are believed to be key contributors. Increasing attention has been given to the type of diet contributing to overnutrition and the epidemic of obesity among children, with data showing an increased intake of fructose, primarily from soft drinks, as a strong contributor.2 Data indicate that between 1977 and 2001 the consumption of soft drinks in children and adolescents aged 2 to 19 years increased from 3.0% to 6.9%.2 Although the effect of fructose consumption in children on NAFLD has yet to be established, studies in adults have shown that consumption of soft drinks is a risk factor for the development of NAFLD.
In particular, visceral adiposity is associated with pediatric NAFLD; data show that for every 5-cm increase in waist circumference in obese children or adolescents there is an odds ratio of 1.4 for predicting ultrasound-detected liver steatosis.7 The central role of overnutrition and obesity, and in particular visceral adiposity, in the development of NAFLD is associated with a cascade of mechanisms associated with disease development, including insulin resistance, metabolic syndrome, change in lipogenesis, and obstructive sleep apnea.1 Other processes suggested in the pathogenesis of disease involve mitochondrial dysfunction, which is seen as playing a key role in NASH independent of insulin resistance and its consequences, as well as the possibility of a genetic predisposition. Increasing evidence is also pointing to an association between cytokines and adipokines and the mechanism involved with liver damage and repair in fatty liver. Plasma cytokeratin-18 (CK-18), which is a marker of increased hepatocyte apoptosis, has become particularly interesting as a cytokine that may be useful as a biomarker for NASH in children.8
A “2-hit” model or theory has been proposed to describe the pathogenesis of NAFLD based on the recognition that steatosis can be a reversible process and that whether a patient progresses to irreversible liver damage and fibrosis is determined by whether or not they develop steatohepatitis.9,10 In this model, the first hit in the development of NAFLD is an excessive hepatocyte triglyceride accumulation resulting from insulin resistance and the second hit involves an inflammatory injury to the liver possibly by oxidative stress, associated lipid peroxidation, and cytokines (primarily tumor necrosis factor-alpha or endotoxin).10-12
Diagnosis
Children with NAFLD are often asymptomatic or present with mild symptoms such as fatigue, malaise, and vague abdominal pain.1,7 On physical presentation, some children with NAFLD may present with mild-to-moderate hepatomegaly with right upper-quadrant tenderness. Most children with NAFLD will present as overweight or obese, particularly with visceral adiposity, making liver palpation challenging.4 In addition to obesity and being overweight, many children will present with acanthosis nigricans that suggests the presence of insulin resistance. Studies show that up to half of all children with NASH present with acanthosis nigricans.1
Currently there are no screening guidelines to help health care providers diagnose NAFLD in children. Liver biopsy remains the gold standard for making the definitive diagnosis of NASH, but it is not well suited for screening or monitoring children because of its invasive nature, cost, and complications.4 As such, primary care physicians and other health care providers need alternative tools to help make the differential diagnosis in children, including biochemical tests and imaging studies. A number of noninvasive biomarkers of disease are also being studied for their predictive potential. Following is a brief description of these diagnostic tools.
Biochemical tests. Several biochemical tests have been evaluated to help provide information on the potential presence and severity of NAFLD in children, including liver function tests and insulin resistance tests.1,4,7 The most common finding on laboratory studies is a mild-to-moderate elevation of serum alanine aminotransferase (ALT).4 The use of ALT is not considered a good diagnostic marker for NAFLD, however, given its low sensitivity.7,13 Similarly, mildly elevated levels of alkaline phosphates or gamma glutamyl transpeptidase (GGT) have been associated with NAFLD, but these do not indicate the severity of steatosis or hepatic fibrosis.13
Insulin resistance tests may provide information to identify children and adolescents with NAFLD, with some data suggesting that hyperinsulinemia may represent the first pathogenic hit of NAFLD.7 As a single predictor of NAFLD, however, hyperinsulinemia is insufficient given its low specificity. Hypertriglyceridemia, atherogenic lipid profile, and uric acid all have been reported as potential biochemical markers of disease. More studies are needed to identify the best criteria for insulin resistance among the tests available and to determine the exact cutoff measures needed for standard reference.1
Imaging. The primary imaging tools used to diagnose NAFLD in children and adolescents are ultrasound and magnetic resonance imaging (MRI).4 Ultrasound is used in clinical practice as well as in research studies, and shows echogenicity and frequently shows enlargement of the liver. Studies suggest that visceral fat measured by ultrasound may provide a way to predict the risk for NAFLD in obese adolescents, with some data showing ultrasound-detected liver involvement as frequently as 42% among prepubertal children.1
Magnetic resonance imaging is used primarily in research studies because of its expense and has been shown in some studies to accurately quantify fat content in the liver.4 Computed tomography is not recommended because of the need to avoid radiation exposure in children. Although routine testing with ultrasound and MRI can detect advanced disease by signs of portal hypertension, these imaging tools are limited by the lack of sensitivity to detecting fibrosis. Other more novel imaging tools have shown accuracy in detecting liver fibrosis but are currently limited by cost (magnetic resonance spectroscopy), inability to be used in obese patients or those with ascites (transient elastography), and too little clinical data (magnetic resonance elastography).1,4
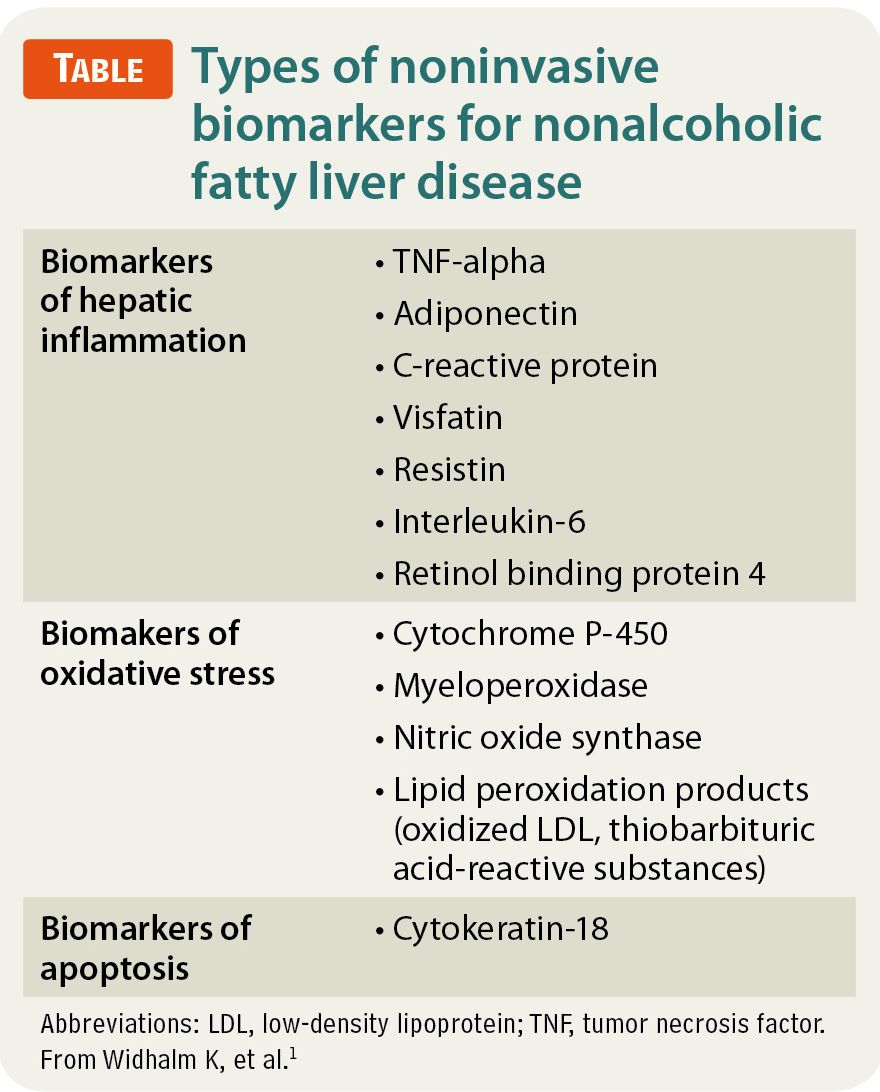
Noninvasive biomarkers. Three groups of noninvasive biomarkers can be used to indicate NAFLD (Table).1 Data suggest that these biomarkers can identify NAFLD and its likely progression. Among these biomarkers, CK-18 is regarded as the most promising biomarker of NASH.13 Data from a recent study of 201 children with biopsy-proven NAFLD showed that serum CK-18 levels were significantly higher in 140 children who had NASH compared with the other children with hepatic steatosis.8 The study highlighted the excellent predictive value of CK-18 for diagnosing NASH, and established several cutoff values to maximize sensitivity and specificity for the prediction of NASH on biopsy. Currently these biomarkers are used to diagnose NAFLD for research purposes, but it is hoped that their future role will include staging and monitoring of disease.4
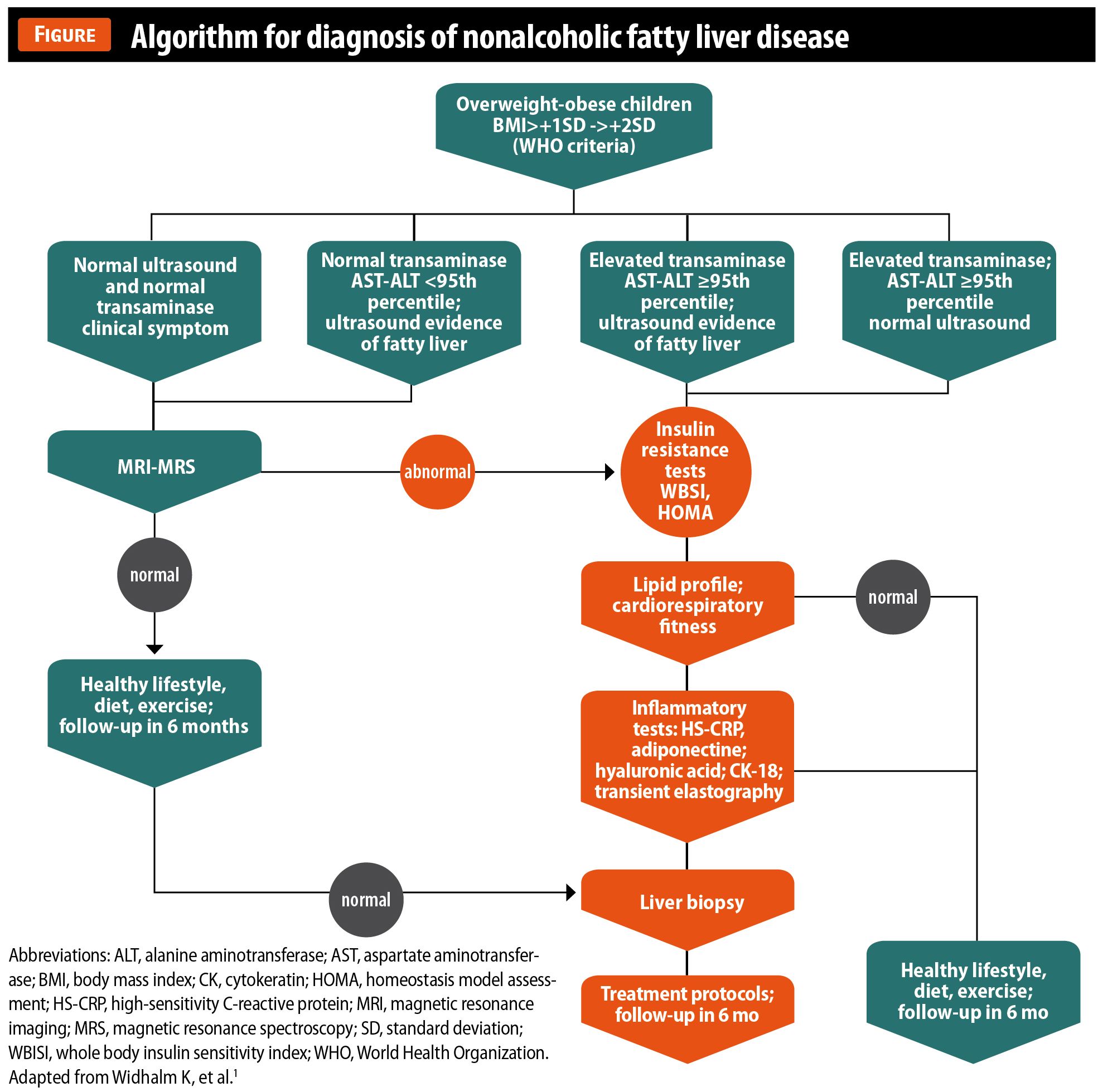
The Figure provides an algorithm that may be useful as a guide for diagnosing NAFLD in children.1 The algorithm recommends routine biochemical testing (liver transaminases) as well as imaging (liver ultrasound) in all children who are overweight or obese as defined by World Health Organization (WHO) criteria. If any of these tests suggest fatty liver, further testing is done to check the presence of insulin resistance. If insulin resistance is found, further testing for inflammatory markers is undertaken to determine the presence of fibrosis. In patients with a high suspicion of NASH, a liver biopsy is recommended.
Treatments
The first line of treatment and prevention of NAFLD focuses on lifestyle interventions.1,2 Studies show that even very modest changes in diet and physical activity that may or may not lead to weight reduction can improve liver function tests, cytokines, and histology of NASH.1 One study found significant improvements in markers of insulin resistance, aminotransferases, and hepatic lipid content in 68% of 84 pediatric patients with biopsy-proven NAFLD followed for 1 year in a lifestyle-intervention study.2 Another study suggests that improvements can occur within weeks of changes to diet and physical activity.
Although there seems to be a clear benefit from modifications to diet and physical activity on obesity and associated disease mechanisms of NAFLD, getting children and adolescents to undergo and maintain these lifestyle changes remains challenging, and there are currently no standards for lifestyle changes that offer the most benefit.1,2 Some experts recommend that children and adolescents be encouraged to follow a low-fat, low-glycemic-index diet that includes eating a minimum of 5 servings of vegetables and fruits daily, engaging in physical activity for at least 1 hour daily, and minimizing television/computer time to 2 hours daily.2
Other treatment approaches given the difficulty of compliance with lifestyle changes include medical therapies for NAFLD that target the metabolic syndrome (thiazolidinediones, metformin) or the hepatoprotective response (statins, vitamin E).1,2 Two randomized clinical trials support the use of vitamin E in addition to lifestyle interventions for the treatment of NASH.4 In the PIVENS (Pioglitazone or Vitamin E for NASH Study) 96-week study that compared pioglitazone or vitamin E with placebo in 247 adult patients with biopsy-proven NASH, significant improvements in steatosis and lobular infiltration (but not in fibrosis scores) were found in the patients in the vitamin E group compared with the placebo group. The TONIC (Treatment of NAFLD in Children) trial of 173 children with biopsy-proven NAFLD that compared vitamin E with metformin or placebo for 2 years found that neither high-dose vitamin E nor metformin significantly improved ALT versus placebo. Significant improvement in histologic findings, however, was found in the children taking vitamin E. In a subset of children with established NASH at initial biopsy, 58% receiving vitamin E showed significant histologic resolution after 96 weeks of treatment with no adverse effects noted.
Conclusion
With the increase in pediatric NAFLD, primary care physicians and other health care providers can play an important role in recognizing the signs and symptoms of early disease and intervene before the disease progresses.
REFERENCES
1. Widhalm K, Ghods E. Nonalcoholic fatty liver disease: a challenge for pediatricians. Int J Obes (Lond). 2010;34(10):1451-1467.
2. Mencin AA, Lavine JE. Advances in pediatric nonalcoholic fatty liver disease. Pediatr Clin North Am. 2011;58(6):1375-1392.
3. Schwimmer JB, Deutsch R, Kahen T, Lavine JE, Stanley C, Behling C. Prevalence of fatty liver in children and adolescents. Pediatrics. 2006;118(4):1388-1393.
4. Ovchinsky N, Lavine JE. A critical appraisal of advances in pediatric nonalcoholic fatty liver disease. Semin Liver Dis. 2012;32(4):317-324.
5. Schwimmer JB, Behling C, Newbury R, et al. Histopathology of pediatric nonalcoholic fatty liver disease. Hepatology. 2005;42(3):641-649.
6. Carter-Kent C, Yerian LM, Brunt EM, et al. Nonalcoholic steatohepatitis in children: a multicenter clinicopathological study. Hepatology. 2009;50(4):1113-1120.
7. Vajro P, Lenta S, Socha P, et al. Diagnosis of nonalcoholic fatty liver disease in children and adolescents: position paper of the ESPGHAN Hepatology Committee. J Pediatr Gastroenterol Nutr. 2012;54(5):700-713.
8. Feldstein AE, Alkhouri N, De Vito R, Alisi A, Lopez R, Nobili V. Serum cytokeratin-18 fragment levels are useful biomarkers for nonalcoholic steatohepatitis in children. Am J Gastroenterol. 2013. Epub ahead of print.
9. Lalor PF, Faint J, Aarbodem Y, Hubscher SG, Adams DH. The role of cytokines and chemokines in the development of steatohepatitis. Semin Liver Dis. 2007;27(2):173-193.
10. Carter-Kent C, Zein NN, Feldstein AE. Cytokines in the pathogenesis of fatty liver and disease progression to steatohepatitis: implications for treatment. Am J Gastroenterol. 2008;103(4):1036-1042.
11. Cortez-Pinto H, de Moura MC, Day CP. Non-alcoholic steatohepatitis: from cell biology to clinical practice. J Hepatol. 2006;44(1):197-208.
12. Nagata K, Suzuki H, Sakaguchi S. Common pathogenic mechanism in development progression of liver injury caused by non-alcoholic or alcoholic steatohepatitis. J Toxicol Sci. 2007;32(5):453-468.
13. Yang HR. Noninvasive diagnosis of pediatric nonalcoholic fatty liver disease. Korean J Pediatr. 2013;56(2):45-51.
MS NIERENGARTEN, a medical writer in St. Paul, Minnesota, has over 25 years of medical writing experience, coauthoring articles for Lancet Oncology, Lancet Neurology, Lancet Infectious Diseases, and Medscape. DR FREED is an editorial board member for Contemporary Pediatrics. The author and the reviewer have nothing to disclose in regard to affiliations with or financial interests in any organization that may have an interest in any part of this article.
Subscribe to Contemporary Pediatrics to get monthly clinical advice for today's pediatrician.