Putting sleep disturbances to rest
Sleep problems are common in children and adolescents. Understanding sleep physiology and educating parents about sleep hygiene and other interventions can turn an unhealthy situation around.
Cover article
Putting sleep disturbances to rest
By Charles A. Pohl, MD, and Amy Renwick, MD
Sleep problems such as frequent awakenings, sleep terrors, and sleepwalking are common in children and adolescents. Understanding sleep physiology and educating parents about sleep hygiene and other interventions can turn an unhealthy situation around.
On several occasions during the last month, a 22-month-old boy has been found thrashing and screaming two hours after falling asleep. The child is difficult to fully awaken during these episodes, yet appears normal the following day. The concerned mother wants to know if the child is traumatized by his weekly visits with her estranged husband.
***
After returning from a family vacation at the beach, a 3-year-old begins to awaken three times a night for a glass of water. The parents ask if this behavior reflects a medical condition, such as diabetes or a bladder infection. If it doesn't, can they give the child a cold medicine to help her sleep?
Teddy bears. Lullabies. Sweet dreams. We like to think of bedtime as a peaceful period and sleep as a refreshing rest. In reality, bedtime for many children and their parents is a stressful occasion, and a good night's sleep merely a sweet dream.
A third or more of children and adolescents experience sleep problems, like those described in the two opening scenarios.13 Common complaints include bedtime refusal, frequent awakenings, daytime sleepiness, nightmares, and sleepwalking. These disturbances result in parental anxiety, frustration, and sleeplessness. Affected children may be irritable, less successful in school,1,4,5 and more prone to injury.6 Sleep disturbances can thus have a far-reaching effect on the entire family. Parental interventions may unintentionally exacerbate the problem.
To establish and preserve healthy sleep patterns, it is important for families and pediatricians to understand normal sleep physiology and common causes of disruptions. This article reviews developmentally appropriate sleep patterns in children and discusses common sleep disturbances, emphasizing a practical approach to management.
Physiology of normal sleep
The sleep-wake cycle and the physiologic patterns of sleep undergo developmental changes from infancy to adulthood. Newborns spend about 70% of their time sleeping; adults, only 25% to 30%. Infants require about 14 to 16 hours of sleep daily (Figure 1 in the print edition: Figure 1, from Ferber R, Kryger M: Principles and Practice of Sleep Medicine in the Child. Philadelphia, WB Saunders Company, 1995, Used with permission from Elsevier Science).7 Daily sleep time decreases to about 13 hours by 2 years of age, 11 hours by 5 years, 10 hours by 10 years, and eight to nine hours during adolescence.
Term newborns typically have four to six evenly distributed sleep-wake periods daily. Consolidation of daily sleep into the nighttime period usually begins by 6 weeks of age. Many infants start to sleep through the night by 4 to 6 months of age. Daytime sleep usually diminishes to three naps per day by 6 months, two naps per day between 6 and 12 months, one nap per day between 12 and 24 months, and no naps by 3 to 5 years. Including this information in routine health maintenance visits can promote good sleep routines as well as alleviate many parental anxieties.
Two distinctive sleep states have been identified: non-rapid eye movement (NREM) and rapid eye movement (REM). These states, present in virtually all mammals and birds, are separated from one another by unique behavioral characteristics and by physiologic patterns on polysomnography.
During NREM, brain activity slows, while muscle movement and thermoregulation are preserved. NREM sleep cycles predominate during the first third to half of nighttime sleep and are divided into four stages. Early sleep progresses through NREM stages 1 to 4 (Figure 2 in the print edition, from: Sheldon, SH, Spire J-P, Levy HB: Pediatric Sleep Medicine. Philadelphia, WB Saunders Company, 1992, Used with permission from Elsevier Science). In stage 1, the sleeper is drowsy and still somewhat responsive. By stages 3 and 4 (also called slow-wave sleep, delta-wave sleep, and deep sleep), it is very difficult to arouse the sleeper, who is quite confused if awakened. This physiologic pattern helps explain why sleep problems that take place during NREM stages 3 and 4, such as sleep terrors and sleepwalking, occur early in the night and are characterized by dramatic body movements with no awareness of the environment.
REM, or active, sleep cycles predominate in the latter half to third of the night. The portion of total sleep that is REM sleep decreases with agefrom about 50% to 80% in infancy to 20% to 25% in adulthood.8 During the REM stage, muscle tone is inhibited in all but the ocular and respiratory systems, and thermoregulation is lost. The sleeper has episodic bursts of rapid eye movement (eyelids usually closed), irregular pulse, and tachypnea, while extremity muscles are usually motionless. Muscle twitches are occasionally observed during this sleep phase. Dreams are common.
Partial awakenings, which are times when the sleeper enters a light sleep from a deeper sleep, are common in both children and adults. The sleeper may open his eyes but resumes a deeper sleep once he recognizes a familiar environment. These awakenings are especially common in children 6 to 12 months of age. To help keep sleep problems from developing, children should be encouraged to fall asleep in the familiar surroundings of their own crib or bed, and parents should be encouraged not to disturb their infant during partial awakenings.
Children younger than 3 months of age experience three, rather than two, distinct stages of sleep: NREM, REM, and indeterminant sleep. This last phase is defined by physiologic changes on the sleep study inconsistent with the other two stages. Unlike the sleep composition of older children and adults, the sleep composition of infants predominantly consists of REM. At this age, sucking movements, facial twitches or grimaces, vocalizations, and stretching during REM sleep are common. Minimal body movement is noted during this stage.
In addition to the makeup of a person's sleep architecture (awake-NREM-REM cycles), timing and structure of sleep depend on circadian rhythm over a 24-hour period. The biologic clock affects not only sleep but also hormonal secretion, core body temperature, and kidney function. Social and environmental cues are required to maintain a 24-hour sleep-wake cycle. In the absence of external input, the cycle is between 24.5 and 25 hours. Infants can become entrained to a 24-hour cycle by 2 months of age.9
Light's effect on the suprachiasmatic nucleus (SCN) of the hypothalamus appears to be the most important factor regulating or pacing the circadian system (Figure 3). Retinal photoreceptors relay information to the SCN when exposed to light. Studies have shown that light is capable of shifting the cycle by as long as two hours a day: Light exposure before sleep can delay sleep onset; light exposure toward the end of sleep can hasten awakening. Melatonin, normally secreted by the pineal gland at night, has an opposite effect.10 [Editors' note: For information on melatonin, see "
Core body temperature fluctuates in a typical pattern during the sleep-wake cycle and appears to be important in regulating sleep (Figure 4, from: Richardson GS, Carskadon MA, Orav EJ: Circadian variation of sleep tendency in elderly and young subjects. Sleep 1982;5(Suppl 2):S82, and Kryger MH, Roth T, Dement WC: Principles and Practice of Sleep Medicine). Philadelphia, WB Saunders Company, 1994.11 The temperature is lower during sleep periods such as nighttime and mid afternoon and higher during wakeful hours. Declining body temperature appears to facilitate sleep. If a person attempts to fall asleep during the "wrong" part of the cyclein the evening, for example, when body temperature is risingsleep is less likely to occur and, if it does, is more likely to be disrupted.
Although the need for a good night's sleep is obvious, the biologic function of sleep is unknown. Studies suggest, however, that NREM sleep plays a role in restoration of somatic tissue. REM sleep, on the other hand, appears to be important in learning and memory processing as well as central nervous system restoration. Sleep also is thought to be important to the immune system. In adults, sleep is associated with changes in levels of circulating catecholamines and cytokines such as interleukin-6 and interleukin-2.12
Evaluating sleep problems
In most cases, a careful history and physical examination can elicit the underlying sleep problem. Subsequent evaluation and management can be tailored to specific patient issues, based on the findings of the initial assessment.
Obtain a detailed sleep history, in addition to a history of the patient's presenting complaint; the medical, developmental, and psychological history; and the family and social history. Questions should identify the patient's sleep-wake schedule, current sleep patterns, and associated nighttime and daytime symptoms. It also is important to ask about the child's sleep environment. A list of useful questions appears in Table 1.
TABLE 1
Questions for a sleep history
How much time does the child spend in bed? How much of that time is she asleep?
What time does the child go to bed?
What does she do in the hour before bedtime? Is there a consistent bedtime routine?
If the child has nighttime feedings, how many ounces does she consume?
What is the sleep environment like? (Ask about co-sleeping, noise, temperature.)
Does the child snore?
When does the problem occur relative to bedtime and relative to the time of actually falling asleep?
What does the child do? (Elicit a detailed description of the problem.)
Does she seem aware of what is happening?
How does the parent respond?
How often does the problem occur?
When does the child wake up in the morning? Is she difficult to awaken?
Is the child sleepy during the day? Is school performance affected?
Are there any other daytime symptoms?
How much caffeine does the child consume (in coffee, tea, soda, chocolate)?
Is the child taking medications?
A diary of the child's sleep pattern and complaints can be a useful evaluation tool. It can give the pediatrician a better idea of the real extent of the problem, especially in families where the parents remember only two evenings: the child's worst night and the one just preceding the office visit. Videotaping any unusual events (such as abnormal breathing patterns or movements during sleep) also may be helpful during the initial evaluation.
A general physical examination should be performed, but it is rarely helpful in patients whose history does not provide clues to organic or functional disease. Special attention should be paid to the airway and the nervous system. Observation of the child's behavior and parent-child interaction also is useful.
In most cases, no additional investigation of the child's problem is necessary once a detailed history has been obtained and a physical examination performed. In cases where further investigation is warranted, studies and tests should be tailored to the child's clinical presentation. Polysomnography, which includes an electroencephalogram (EEG), electromyogram (EMG), and electro-oculogram (EOG) and sometimes additional monitors, is useful if a disorder such as nocturnal seizures, obstructive sleep apnea,13 or narcolepsy is suspected.
Other studies to consider are a multichannel sleep study with a pH monitor, airway or pulmonary evaluation, neurologic tests, psychological testing, head imaging studies, toxicology screens, and cardiac studies. Any child being awakened by pain requires a thorough evaluation to rule out malignancy or serious systemic illness.
Managing sleep-time disturbances
Sleep interruption is common in the pediatric population and can impair quality of sleep for the child and parents alike. These disruptions, in turn, can affect the health, development, and quality of life of the child and parents. Sometimes, irregular sleep patterns result in potentially dangerous situations. The remainder of this article discusses specific causes of sleep disruptions (Table 2) and management strategies.
TABLE 2
Causes of nighttime sleep disruptions in children
Arousal disorders (sleep terrors and sleepwalking)
Nightmares
Inappropriate sleep schedule
Unreasonable parental expectations
Sleep-onset association disorder
Excessive nighttime feeding
Limit-setting sleep disorder
Social stresses
Psychiatric conditions
Medical and neurologic disorders
Pharmacologic therapies
Nocturnal seizures
REM behavior disorder
Environment-induced sleep disorder
Remember that cultural practices regarding sleep vary. If the child, parents, and family schedule are not disturbed by an unusual sleeping practice, there is little point in trying to adjust sleep habits.
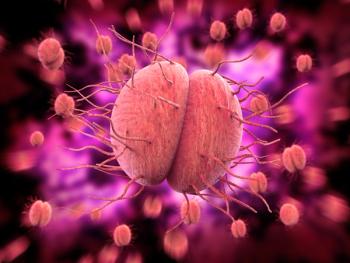
Arousal disorders. About 25% of children suffer from an arousal disorder, such as sleepwalking or sleep terrors.14 Arousal disorders occur during NREM stages 3 and 4 (slow-wave or deep sleep); as expected, parents report that the events occur in the first third to half of the child's sleep. These disorders can have dramatic symptoms (significant muscle movement, tachycardia, tachypnea, diaphoresis) and are characterized by, in addition to significant muscle movement, unresponsiveness to the environment and lack of remembrance of the episode upon awakening. Episodes are exacerbated by inadequate or disruptive sleep. Children with these disorders do not have daytime symptoms (such as daytime sleepiness) or polysomnographic abnormalities.
Sleepwalking (somnambulism) is perhaps the most dangerous sleep disorder, with the potential for causing severe injury, even death. Risks include walking through glass, falling down stairs, and wandering into traffic or extreme weather. Sleepwalking begins in the preschool or school years. Episodes last up to 10 minutes, during which the sleepwalker may perform complicated tasks or urinate in inappropriate places without conscious awareness.
A sleeping child who suddenly screams and is found thrashing about and sweaty with dilated pupils is probably having sleep terrors, or pavor nocturnus. Attempts to comfort the child are unsuccessful, but after 10 minutes or so he (or she) returns to a calm sleep state. Sleep terrors usually begin after the age of 18 months. Although the child appears terrified, he will not recall a particular scary dream or even the episode itself.
Arousal disorders may be distressing to witness, but they do not indicate any underlying psychopathology and rarely require any significant intervention other than parental education. These disorders begin to resolve as the child reaches adolescence. There is no need to try to awaken the child during an episode. Sleepwalkers can be led back to their beds. Parents should ensure the child's safety by preventing access to stairways and streets. In extreme situations, and if the sleep terrors or sleepwalking occur at a predictable time each night, parents can attempt to put an end to the sleep disturbance by waking the child 15 to 30 minutes before an event and then allowing him to resume sleep after several minutes.15,16 Improved sleep hygiene (Table 3), stress reduction, or a brief afternoon nap (an hour or less) may also help.17 Medications and psychotherapy are rarely indicated.
TABLE 3
Establishing basic sleep hygiene habits
General
Follow a consistent schedule for bedtime and wakening
Never use bed as a place of punishment
Daytime
Discourage daytime play in the bed
Limit caffeine, especially after lunchtime
Schedule naps, if needed, early in the day (before 2 p.m.)
Nighttime
Turn the television off at least 30 minutes before bedtime
Avoid meals, exercise, or stimulating television shows near bedtime
Have the child empty his bladder just before going to bed
Establish a calming bedtime routine
Make the sleeping environment quiet, dark, and not too hot or cold
Put the child in bed while he is still awake
Put infants to sleep on their backs
Don't reward the child for leaving bed
Nightmares. Parents frequently confuse sleep terrors with nightmares. Table 4 lists the distinguishing features of these two problems. Unlike the child experiencing sleep terrors, the child having a nightmare may awaken spontaneously and will usually remember having had a frightening dream. Nightmares occur during REM sleep ("REM-ember"), in the latter half of the sleep period. There is little movement during the episodes. Once the child is awake, she is consolable, although possibly too scared to fall back to sleep readily.
TABLE 4
Distinguishing sleep terrors from nightmares
Anxiety or disturbing daytime events may trigger nightmares. Propose that parents discuss nightmares during the day and reassure children that they are safe. Television shows, movies, video games, and books should be screened for material that may be too frightening. Television sets should not be left on near a sleeping child.
Nightmares that recur frequently or cause severe sleep disruption can signal an underlying problem such as abuse or posttraumatic stress disorder. Referral for mental health evaluation may be indicated.
Nocturnal seizures are rare in children. Unlike sleep terrors, nocturnal seizures do not occur consistently in the early part of sleep, and the child usually has daytime symptoms (such as developmental delay, behavior changes, excessive sleepiness, or a tic disorder). Also suspect nocturnal seizures if symptom onset is after 9 years of age or if there is a prolonged recurrence.18 Polysomnography can distinguish this disorder from sleep terrors. Nocturnal seizures usually require antiepileptic medication.
REM behavior disorder. As with nocturnal seizures, REM behavior disorder is rare in children and can be distinguished from sleep terrors by polysomnography. REM behavior disorder is caused by the return of muscle tone during REM sleep. Patients act out their dreams, sometimes violently. They usually respond to clonazepam therapy.
Inappropriate sleep schedule or parental expectations. A child may develop nighttime awakenings if the length of time he is expected to sleep exceeds his total sleep requirement. In other words, if a child requires 10 hours of sleep, he is likely to have sleep refusal, nighttime arousal, or early awakening if he is expected to be in bed for 12 hours each night. A problem also can develop if a child takes extra naps in a stroller or the car. Therefore, it is important for the pediatrician to not only calculate the appropriate sleep requirement for a child's age and development but also to elicit a complete sleep history for each 24-hour period.
Sleep-onset association disorder. Some children relate the onset of sleep to tactile stimulation with an object such as a pacifier. Others associate onset of sleep with an activity such as rocking, breastfeeding or bottle-feeding, or watching television. If that transitional object or activity is not present when the child awakens during the night, he is unable to resume sleep on his own. A pediatrician can be confident that sleep-onset association disorder is the problem if sleep quickly resumes once the child receives the "security blanket" (pacifier, rocking, television). Encourage parents to condition a new sleep-association habit by putting the child to bed while he is still awake.
Excessive nighttime feeding. Infants may have frequent nighttime awakenings secondary to excessive nighttime feeding. The awakenings may be the result of discomfort from urination, sleep-onset association, a disruption in the circadian rhythm (resultingin sporadic hunger pain), or a learned habit. Clues that suggest this problem include significant nocturnal intake, saturated diapers, and sleep onset after a feeding. The nocturnal feedings should be gradually eliminated, and the child needs to learn to initiate sleep on his own.
Limit-setting sleep disorder. Many toddlers are reluctant to go to bed. They may feel they will miss exciting events, or simply prefer not to be left alone, and leaving bed is an opportunity for them to demonstrate their new autonomy. Some are confused by inconsistent bedtime rules. These factors may result not only in bedtime refusal ("curtain calls") but also nighttime awakenings. Unlike sleep-onset association disorder, the unwanted behavior persists regardless of the presence of a transitional object or when it is time to go to sleep.
A consistent parental response is key to curbing this behavior. A predictable, nonstimulating, nonnegotiable bedtime routine must be implemented. Parents should be counseled to make bedtime a pleasant time and to never make going to bed a punishment. If a child gets out of bed, he should be calmly and immediately led back. Allowing him to join in activities, watch television, or just stay up a little longer will reinforce the unwanted behavior. Stickers or other rewards given for staying in bed may be useful.
Most infants are able to sleep through the night by the age of 4 to 6 months. Having said that, children under 2 years of age are often plagued by frequent nighttime awakenings. Most of these events could have been avoided had the caregiver initiated good bedtime habits earlier (Table 3). Parents should be encouraged to establish a calming bedtime routine, to put the child in bed while he is still awake, and to not disturb babies during episodes of partial awakening. They also must be educated about developmentally appropriate sleep patterns. (See the "
Children usually resume restful sleep once the principles of basic sleep hygiene are implemented. After bedtime, the interaction between the child and the parent should be minimal and nonstimulating, and periods between contacts should be gradually lengthened.
Social stresses and psychiatric conditions. Nighttime disturbances often occur when children experience fear or anxiety. Unlike children who have a limit-setting sleep problem, those who have trouble sleeping because they are scared or anxious usually have daytime symptoms (for example, alterations in eating patterns, social altercations or isolation) and remain upset despite parental comforting. In such cases, the inciting fear-factor must be removed and the child needs to be nurtured. The child's sleep location and sleep schedule should be flexible until the child is less fearful or anxious. Behavioral modifications such as the gradual withdrawal of the parent's presence at night may be necessary. Parents may need to initially sit near the bed until the child falls asleep, and then on successive nights move farther away, eventually moving out of the room. Interaction should be restricted to brief, calm reassurances. Lengthy discussion about the fears is betterheld in the daytime.7 Occasionally, pharmacologic interventions such as benzodiazepines are necessary.
The use of antihistamines such as Benadryl or other over-the-counter formulations as sleep aids in children is not recommended. These medicines, which may cause adverse reactions, can occasionally mask the sleep disturbance and prevent the underlying problem from being identified.
Sleep disturbances may be prominent features of the presentation of psychiatric conditions such as schizophrenia and depression. A referral to a pediatric psychiatrist is usually necessary in such cases.
Medical and neurologic disorders and pharmacotherapeutics. Many medical conditions can influence sleep patterns and behavior. In such cases, the child is usually fully awake and cannot be calmed in a parent's bed. Associated symptoms, such as fever and pain, are typically present, enabling the pediatrician to identify the problem and provide appropriate care. Any child with snoring or abnormal breathing during sleep, for example, should be evaluated for obstructive sleep apnea syndrome (OSAS), which can disturb the quality of sleep in addition to causing potentially fatal complications such as cor pulmonale. A full discussion of OSAS is beyond the scope of this article; the reader is referred to the recent American Academy of Pediatrics practice guideline for more information.13 Asthma, colic, otitis media, and gastroesophageal reflux disease are other common medical problems associated with sleep disruption. Any medication should be considered a possible culprit in nighttime awakenings. After addressing any identified underlying factors, parents should give children ample opportunity to return to sleep on their own, allowing older children to engage in quiet, safe activities (such as singing or reading) in bed if necessary.
Environment-induced sleep disorder. Children appear to be more distracted by environmental disruptions than are adults. Chaotic or noisy settings such as motel rooms and airports, violent television shows, or urban travel can result in nighttime awakening.
Turning stressful to restful
Sleep disturbances are common in children and adolescents and can have a significant effect on them and their families. A careful history often identifies the underlying cause of the problem. Improved sleep hygiene is the mainstay of treatment.
REFERENCES
1. Wolfson AR, Carskadon MA: Sleep schedules and daytime functioning in adolescents. Child Development 1998;69:875
2. Stores G: Practitioner review: Assessment and treatment of sleep disorders in children and adolescents. J Child Psychol Psychiatry 1996;37:907
3. Morrison DN, McGee R, Stanton WR: Sleep problems in adolescence. J Am Acad Child Adolesc Psychiatry 1992;31:94
4. Randazzo AC, Muehlbach MJ, Schweitzer PK, et al: Cognitive function following acute sleep restriction in children ages 1014. Sleep 1998;21:861
5. Meijer AM, Habekothe HT, Van Den Wittenboer GL: Time in bed, quality of sleep and school functioning of children. J Sleep Res 2000;9:145
6. Valent F, Brusaferro S, Barbone F: A case-crossover study of sleep and childhood injury. Pediatrics 2001; 107:e23
7. Ferber R, Kryger M: Principles and Practice of Sleep Medicine in the Child. Philadelphia, WB Saunders Company, 1995
8. Sheldon SH, Spire J-P, Levy HB: Pediatric Sleep Medicine. Philadelphia, WB Saunders Company, 1992
9. McGraw K, Hoffmann R, Harker C, et al: The development of circadian rhythms in a human infant. Sleep 1999;22:303
10. Comella CL, Walters AS, Hening WA: Sleep and wakefulness. Textbook of Clinical Neurology, ed 1. Philadelphia, WB Saunders, 1999
11. Kryger MH, Roth T, Dement WC: Principles and Practice of Sleep Medicine. Philadelphia, WB Saunders Company, 1994
12. Redwine L, Hauger RL, Gillin JC, et al: Effects of sleep and sleep deprivation on interleukin-6, growth hormone, cortisol, and melatonin levels in humans. J Clin Endocrinol Metab 2000;85:3597
13. American Academy of Pediatrics: Clinical practice guideline: Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2002;109:704
14. Archbold KH, Pituch KJ, Panahi P, et al: Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatrics 2002;140:97
15. Frank NC, Spirito A, Stark L, et al: The use of scheduled awakenings to eliminate childhood sleepwalking. J Pediatr Psychol 1997;22:345
16. Lask B: Novel and non-toxic treatment for night terrors. BMJ 1988;297:592
17. Anders TF, Eiben LA: Pediatric sleep disorders: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry 1997;36:9
18. Zucconi M, Ferini-Strambi L: NREM parasomnias: Arousal disorders and differentiation from nocturnal frontal lobe epilepsy. Clin Neurophysiol 2000;111(Suppl 2): S129
DR. POHL is director, Network of Apnea and Pediatric Sleep Center, and clinical associate professor, department of pediatrics, Jefferson Medical College of Thomas Jefferson University, Philadelphia, Pa.
DR. RENWICK is chief resident, department of pediatrics, Thomas Jefferson University and Alfred I. duPont Hospital for Children, Philadelphia, Pa.
Revisiting our two patients
Case 1. The 22-month-old boy is most likely experiencing sleep terrors. Unlike children who have nightmares or anxiety problems, children with sleep terrors do not awaken from the events and their symptoms usually resolve spontaneously within minutes. They also do not experience symptoms during the day, such as daytime sleepiness. The parent should be reassured that sleep terrors are common and do not require any interventions or medications. The caregiver should be encouraged to avoid erratic sleep schedules and to call if symptoms change or become worse.
Case 2.Changes in sleep patterns are common when a child's sleep schedule is disrupted. Normal sleep should resume if the family returns to the regular bedtime routine that was practiced before the vacation. Suspect a medical condition if this new behavior does not subside in the course of one or two weeks, is observed during the daytime, or is associated with other symptoms. Over-the-counter medications, such as the common cold formulation that the family is proposing, are not an effective means to promote a proper sleep pattern.
The parent guide on how to help your child get a good night's sleep may be photocopied and distributed to families in your practice without permission of the publisher.
Helping your child sleep well
A good night's sleep can make a big difference in your child's day (and yours). Sleep is thought to be important for learning, growth, healing, and proper function of the immune system. Children who don't sleep well may be irritable, less successful in school, and more likely to have an accident. And if one person in the family isn't sleeping, the rest of the family may be kept awake by the problem. Fortunately, certain simple things you can do are the keys to good sleep.
What to expect
Newborns sleep 14 to 16 hours a day, spread evenly through the day and night. After about six weeks, babies begin to sleep more during the night than the day. While they sleep, you may see sucking movements, facial twitches, or stretching. By age 4 to 6 months, many infants sleep through the night.
From 6 months to adulthood, sleepers occasionally have partial awakenings during the nightthey may stir, open their eyes, and even cry. They will fall asleep again if they recognize a familiar environment and are not disturbed.
Toddlers generally need 11 to 13 hours of sleep a day, including a daily nap until they are 3 to 5 years old. School-age children should get 10 to 11 hours of daily sleep. Adolescents need eight to nine hours of sleep; they frequently get less than this amount.
Basic tips for improving sleep
Follow a consistent schedule for bedtime and awakening.
Never use your child's bed as a place of punishment.
Discourage daytime play in the bed.
Schedule naps, if needed, early in the day (before 2 p.m.).
Limit caffeine, especially after noon.
Turn the television off at least 30 minutes before bedtime.
Avoid meals and exercise near bedtime.
Have your child empty his (or her) bladder just before going to bed.
Establish a calming bedtime routine; bedtime stories are perfect.
Make sure the sleeping environment is quiet, dark, and not too hot or cold.
Put infants to sleep on their backs.
Put your child in bed while he is still awake, so he gets used to falling asleep there.
Don't reward your child for leaving bedTV, play, and long conversations with you should not be allowed.
If your child gets out of bed, calmly and immediately lead him back to bed.
Stickers or other rewards given for staying in bed may be useful if your child keeps getting out of bed.
Common problems
Nightmares usually occur late in the night, and they may awaken the child. He will remember having had a frightening dream. Reassure him that he is safe and can continue to sleep in his bed. Nightmares can be triggered by daytime events and fears. Television shows, movies, video games, and books should be screened by you for material that may be too frightening for your child.
Sleep terrorsoccur earlier in the night than nightmares do. Children may scream, open their eyes, sit up, or thrash about in bedbut they are not truly awake. They are unable to be comforted, but after 10 minutes or so they return to a calm sleep. They do not remember having a scary dream or even that anything happened. These episodes resolve on their own as the child reaches adolescence.
Sleepwalkingcan be dangerous, because sleepwalkers are able to do complicated tasks without any conscious awareness. Risks of sleepwalking include walking through glass, falling down stairs, and wandering into traffic or bad weather. You don't need to try to awaken a sleepwalker; just lead him back to bed. Most importantly, make sure he cannot get to stairways, streets, or other hazardous areas.
Resources
If you want to know more about sleep in children, here are a few books:
Solve Your Child's Sleep Problems, by Richard Ferber
Sleeping Through the Night: How Infants, Toddlers, and Their Parents Can Get a Good Night's Sleep, by Jodi A. Mindell
American Academy of Pediatrics Guide to Your Child's Sleep: Birth Through Adolescence, edited by George J. Cohen
This guide may be photocopied and distributed without permission to give to the parents of your patients. Reproduction for any other purpose requires express permission of the publisher.
Newsletter
Access practical, evidence-based guidance to support better care for our youngest patients. Join our email list for the latest clinical updates.