Renovating your medical home
In 2007, a joint statement issued by the American Academy of Pediatrics (AAP), the American Academy of Family Physicians, the American College of Physicians, and the American Osteopathic Association endorsed the patient-centered medical home (PCMH) concept and described how the PCMH can optimize care for patients.
In 2007, a joint statement issued by the American Academy of Pediatrics (AAP), the American Academy of Family Physicians, the American College of Physicians, and the American Osteopathic Association endorsed the patient-centered medical home (PCMH) concept and described how the PCMH can optimize care for patients.1 In addition to identifying the primary care practitioner as the leader of a team whose role is to provide and coordinate patient care, the joint statement further noted that physicians should adhere to evidence-based guidelines, advance the use of information technologies to improve care, and implement practices that improve the quality of care provided to patients.
The medical home is at the very center of the many controversies now surrounding healthcare in this country. There appear to be 2 contrasting views of healthcare in the United States. From the public health perspective, too many patients receive inadequate healthcare because they don’t have ready access to a “medical home” where they receive compassionate care from a medical practice that coordinates necessary medical services. Meanwhile, primary care pediatricians practicing in the “trenches” try to provide the best medical home we can, while recognizing that our patients have individual needs. In this installment of Peds V2.0, we’ll take look at how to identify and rectify practice problems (that is, improving the medical home you provide for patients) and provide some insights regarding the small- and big-picture aspects of healthcare.
Institute of Medicine: Healthcare is broken!
The Institute of Medicine (IOM) presented a negative critique of healthcare in the United States in its 2001 report Crossing the Quality Chasm: A New Healthcare System for the 21st Century.2 It described a healthcare system that is too expensive, too complicated, and with too many patients obtaining fragmented care from too many providers. The consequence of healthcare deterioration is that patients often suffer poor health outcomes. To remedy the situation, the IOM listed several goals for change:
- Improve the safety of the healthcare system;
- Make healthcare more effective via implementation of evidence-based medicine;
- Provide patient-centered care that is respectful and involves patients in decision making;
- Provide timely services that avoid unnecessary delays; and
- Provide care that is equitable and that does not vary in quality because of socioeconomic status, gender, or ethnicity.
Because of the IOM recommendations developed well over a decade ago, we now have a healthcare system that is trying to embrace the above values, with the government seeking radical changes through the implementation of the Affordable Care Act (ACA) and medical insurance companies seeking ways to incentivize physicians to improve the quality of care while containing costs. To support a medical home information technology infrastructure, some pediatric practices with substantial numbers of Medicaid patients have received modest payments to implement electronic health records (EHRs) that facilitate data collection. Payments also are in place to encourage practices to use EHRs to achieve medical home certification and to demonstrate “meaningful achievement” of government-defined outcomes.
Currently several clinical quality measures are associated with “optimal pediatric care” as outlined by the Centers for Medicaid and Medicare Services (CMS) and the National Committee for Quality Assurance (NCQA).3 Pediatricians may be eligible for enhanced reimbursements by providing data documenting the achievement of good patient outcomes, and may eventually be subject to reduced payments if we score poorly!
These benchmarks include:
- Optimizing immunization rates;
- Screening children for obesity;
- Avoiding prescribing antibiotics for children with upper respiratory infections;
- Obtaining rapid strep tests on patients before antibiotics are prescribed;
- Using recommended medications for management of patients with asthma;
- Seeing patients on medications for attention-deficit/hyperactivity disorder quarterly;
- Developmental screening in the first 3 years of life;
- Regular well-child checks; and
- Chlamydia screening for sexually active young women aged 16 years and older.
A home divided
From the public health perspective, all pediatric patients would benefit from having a medical home. Of course, the main flaw in the “big picture” of healthcare is that patients are not just data points in a spreadsheet. Each patient requires individualized care. As discussed in a previous Peds V2.0 article (Contemp Pediatr. 2014;30[5]:30-35), the most cost-effective remedy to the “medical homeless” situation is to raise Medicaid insurance compensation to levels commensurate with those of private payers, thereby enabling pediatricians to provide care to these previously underserved patients.
Unfortunately, the ACA has had unforeseen consequences that discourage utilization of the medical home. In my experience, the high deductibles associated with Obamacare are making parents reluctant to seek care when children are ill, and when they do seek care they wish to minimize the cost of the office visit and associated services.
In my view, it is also inappropriate merely to equate quality care with scores achieved on a short list of benchmarks. Some patients cannot be convinced to immunize their children despite pediatricians’ best efforts. Most pediatricians would empirically treat the symptomatic sibling of a child with a rapid strep test without testing, and according to the above, pediatricians would not be given credit for what is, in reality, cost-effective healthcare. We also cannot control when patients refuse care or fail to make appointments, or do not use healthcare portals as required by stage 2 of the “meaningful use” requirements of the ACA.
How does your practice measure up?
Both at state and federal levels, data have been collected to monitor the quality of healthcare provided to our nation’s children. The CMS publishes yearly reports from the Secretary of Health and Human Services. In 2012, it published an interesting comparison of the percentage of children meeting certain core healthcare measures who were enrolled in either Medicaid or the Children’s Health Insurance Program and compared these to the percentage receiving services who had commercial insurance (Table 1).4 Not unexpectedly, children with commercial insurance tended to be more up-to-date with well visits and immunizations. Adolescents tended to be poorly immunized no matter what type of insurance they had. Interestingly, adolescent teenagers were more likely to be screened for chlamydia if they had Medicaid compared with commercial insurance.
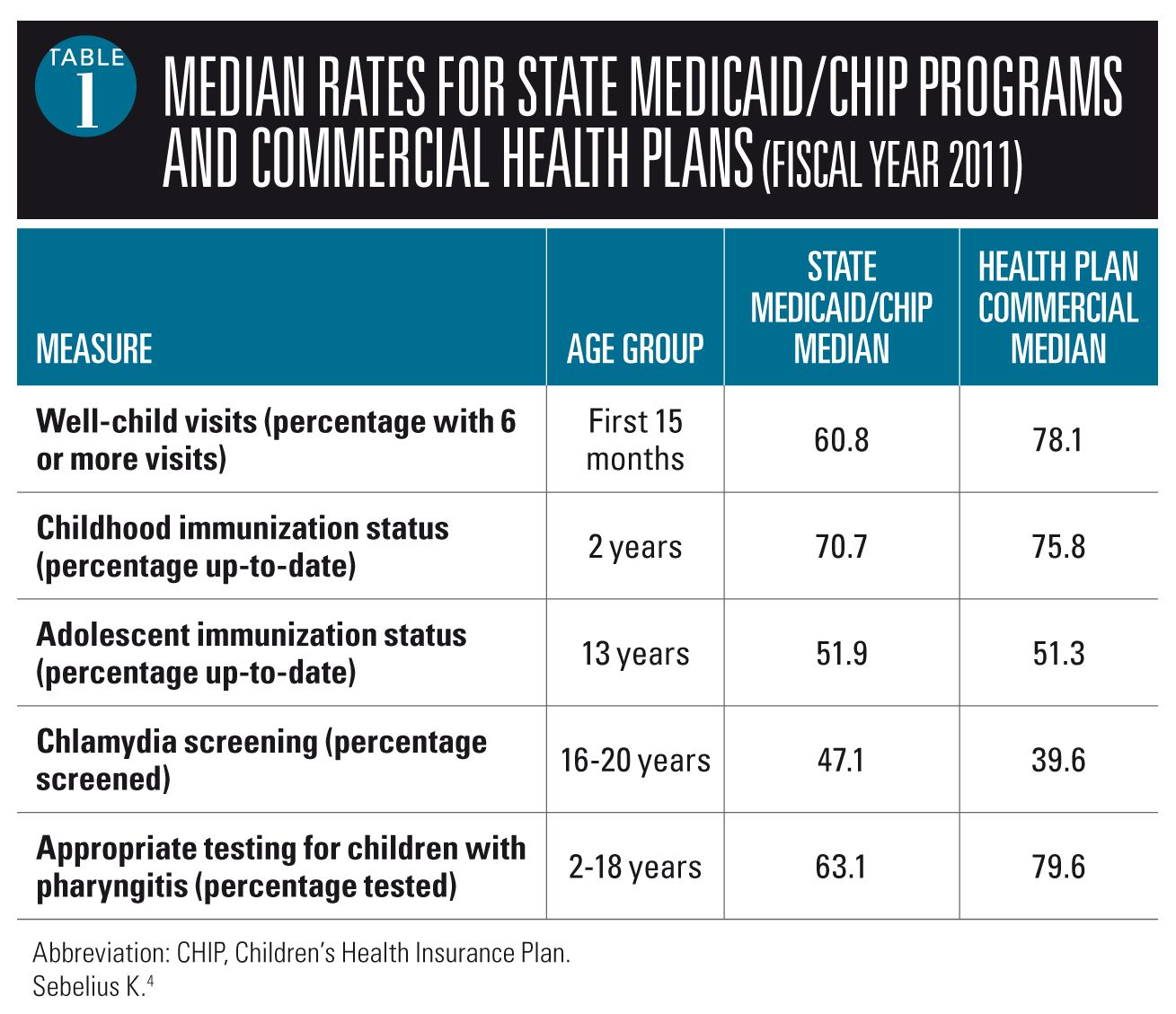
Table 2 shows median (50th) percentile and 90th percentile data from NCQA Healthcare Effectiveness Data and Information (HEDIS) measures.5 These are the performance measures on which your practice will be graded if you apply for NCQA certification, and they also are the numbers that many insurance companies utilize to determine if you are eligible for quality incentive reimbursements.
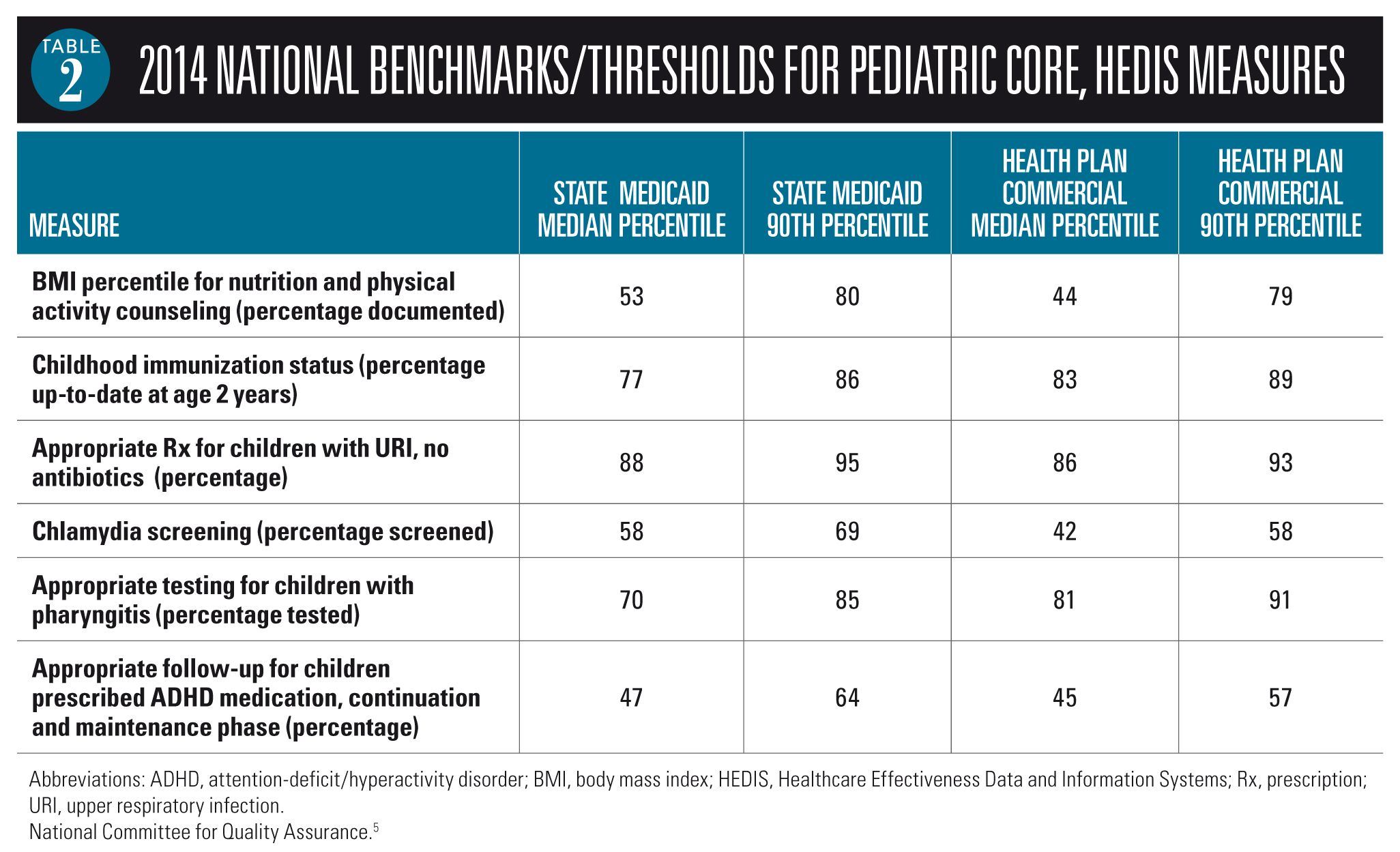
It would be useful to use your EHR to determine where your practice falls regarding these benchmarks. If your numbers look good, you can feel confident your practice should perform well when you apply for medical home certification or participate in insurance plans that are beginning to compensate physicians for quality of care. If you underperform, you would be well advised to work toward improving your practice performance. Also note that surveys of parents figure in the marks you receive from NCQA and insurance companies. Sample surveys can be obtained from www.cahps.ahrq.gov/surveys-guidance/cg/pcmh/index.html.
Start renovating: Identify flaws
Despite our best efforts, there is no such thing as a “perfect pediatric practice” and we can always find ways to improve the services we provide patients. If you have an EHR (and even if you don’t), it would be a good idea to collect data regarding how your practice is performing with the core pediatric performance metrics noted above and consider surveying your patients to determine how their parents’ perceive the care their children receive from you and your staff. You can mail surveys to patients or use an online survey tool such as Survey Monkey (www.surveymonkey.com) to accomplish this. Survey Monkey is an outstanding resource that facilitates designing surveys and e-mailing these to patients. The data analytics collected by the service provide meaningful results that can prove helpful in identifying aspects of your practice wanting improvement. A suggestion box is another time-tested way for patients to provide feedback.
Often it is obvious when workflow in your office needs improvement. This can result from your own observations or from your staff, or from recommendations made by your patients. This is why regular weekly staff meetings, in which everyone is encouraged to speak freely to describe issues and recommend improvements to existing problems, are important. Sometimes, you may be blind to obvious problems with the practice. It is often helpful to walk through the process of a visit in your office from check-in to exit to see how your workflow can be improved or streamlined.
Make the repairs
Once problems with your medical home have been identified, you need to make the necessary fixes. One time-proven approach used to solve problems in industry as well as in healthcare is the plan-do-study-act (PDSA) method. This PDSA methodology is well described at www.aafp.org/practice-management/pcmh/quality-care.html. An excellent worksheet is available at www.aafp.org/dam/AAFP/documents/practice_management/pcmh/qualitycare/PDSA.pdf.
Simply described, the PDSA process involves listing and prioritizing the problems you wish to address. You then assemble a team to study the problems. The team identifies improvements that can be implemented and formulates ways to measure the impact of the changes you are considering. You can run a pilot test to see if your solution does indeed resolve the problem. If things look promising, you collect data before the change; implement the change; and collect postimplementation data to prove that your remedy has indeed been effective. Going forward, you continue to monitor the situation to see if further modifications are indicated.
Keep your eyes on the prize
Pediatricians who have been taking care of children for a long time are confident that we provide quality care to patients. Could we do a little better? Possibly, but not if we have to purchase expensive and cumbersome EHRs that slow us down, just to generate numbers proving our worth. To a large extent, less regulation and more choice would go a long way toward improving pediatric healthcare. Many pediatricians remain unconvinced that our healthcare system is as “broken” as our bureaucrats would lead the public to believe. As mentioned above, pediatricians treat 1 patient at a time, and the outcomes we achieve cannot be measured.
I wonder how bureaucrats would fare if we devised a benchmark system to measure their performance.
REFERENCES
1. American Academy of Family Physicians (AAFP), American Academy of Pediatrics (IAAP), American College of Physicians (ACP), American Osteopathic Association (AOA). Joint principles of the patient-centered medical home. National Center for Medical Home Implementation website. http://www.medicalhomeinfo.org/downloads/pdfs/JointStatement.pdf. Published March 2007. Accessed June 17, 2014.
2. Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC; National Academies Press; 2001.
3. Centers for Medicare and Medicaid Services. Core Set of Children’s Health Care Quality Measures for Medicaid and CHIP (Child Core Set): Technical Specifications and Resource Manual for Federal Fiscal Year 2013 Reporting. Available at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/Medicaid-and-CHIP-Child-Core-Set-Manual.pdf. Updated May 2013. Accessed June 17, 2014.
4. Sebelius K. The Department of Health and Human Services: 2012 Annual Report on the Quality of Care for Children in Medicaid and CHIP. Available at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/2012-Ann-Sec-Rept.pdf. Published December 2012. Accessed June 17, 2014.
5. National Committee for Quality Assurance. 2014 Accreditation Benchmarks and Thresholds. Available at: https://www.ncqa.org/Portals/0/PolicyUpdates/Trending and Benchmarks/2014_BENCHMARKSANDTHRESHOLDS.pdf. Published January 30, 2014. Accessed June 17, 2014.
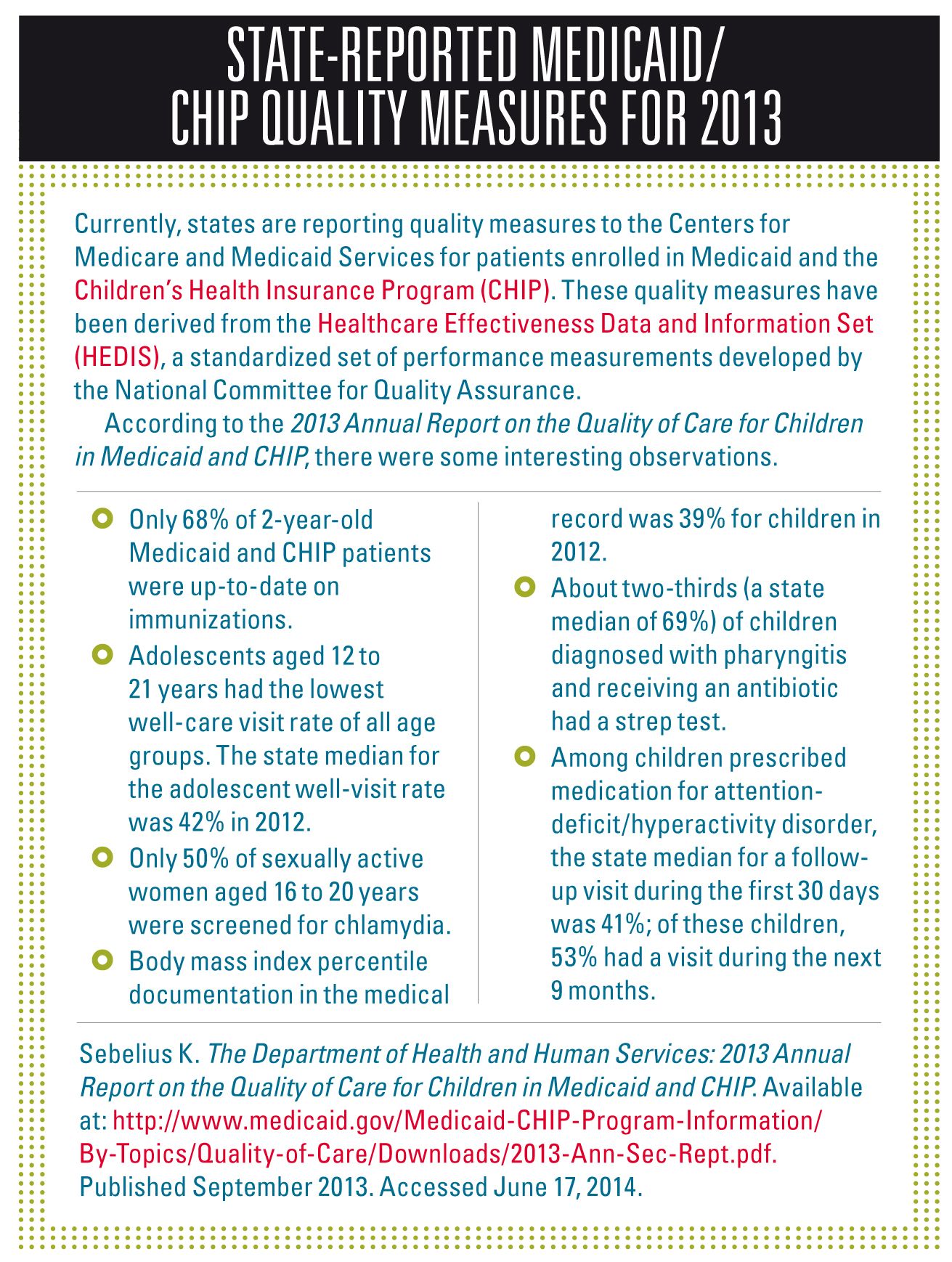
State-reported Medicaid/CHIP quality measures for 2013
Currently, states are reporting quality measures to the Centers for Medicare and Medicaid Services for patients enrolled in Medicaid and the Children’s Health Insurance Program (CHIP). These quality measures have been derived from the Healthcare Effectiveness Data and Information Set (HEDIS), a standardized set of performance measurements developed by the National Committee for Quality Assurance.
According to the 2013 Annual Report on the Quality of Care for Children in Medicaid and CHIP, there were some interesting observations.
- Only 68% of 2-year-old Medicaid and CHIP patients were up-to-date on immunizations.
- Adolescents aged 12 to 21 years had the lowest well-care visit rate of all age groups. The state median for the adolescent well-visit rate was 42% in 2012.
- Only 50% of sexually active women aged 16 to 20 years were screened for chlamydia.
- Body mass index percentile documentation in the medical record was 39% for children in 2012.
- About two-thirds (a state median of 69%) of children diagnosed with pharyngitis and receiving an antibiotic had a strep test.
- Among children prescribed medication for attention-deficit/hyperactivity disorder, the state median for a follow-up visit during the first 30 days was 41%; of these children, 53% had a visit during the next 9 months.
Sebelius K. The Department of Health and Human Services: 2013 Annual Report on the Quality of Care for Children in Medicaid and CHIP. Available at: http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Quality-of-Care/Downloads/2013-Ann-Sec-Rept.pdf. Published September 2013. Accessed June 17, 2014.
Dr Schuman, section editor for Peds V2.0, is adjunct assistant professor of pediatrics, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire. He has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.