Rheumatic fever: No cause for complacence
Resurgences of this dangerous disease during the past two decades make it clear that we cant afford to relax our vigilance. This update reviews the latest thinking about diagnosis, treatment, and prevention.
Cover story
Rheumatic fever: No cause for complacence
By Carl N. Steeg, MD, Christine A. Walsh, MD, and Julie S. Glickstein,MD
Resurgences of this dangerous disease during the pasttwo decades make it clear that we can't afford to relax our vigilance. Here'sthe latest thinking about diagnosis, treatment, and prevention.
Rheumatic fever is the most common acquired heart disease in childrenand young adults and the principal cause of death from heart disease duringthe first 50 years of life. In the pre-antibiotic era it was widespread,filling hospital wards with children suffering from its cardiac sequelae.While it continues to be widespread in some parts of the world, especiallyAsia and Africa, rheumatic fever declined in the US after the introductionof antibiotics. It was considered a rarity until the early 1980s when aresurgence began.1,2 Although it is still not common in thiscountry, rheumatic fever remains a significant clinical problem for pediatriciansand an important reason to treat upper respiratory tract infections causedby group A b-hemolytic streptococci (GABHS) with antibiotics for a full10 days. Appropriate antibiotic therapy effectively prevents rheumatic fevereven though we still have much to learn about its molecular and geneticetiology. In light of the disease's recent resurgence and serious sequelae,pediatricians cannot afford to be complacent about its prevention, diagnosis,and treatment.
A complex epidemiology
Since no definitive diagnostic test for rheumatic fever exists, the preciseincidence is uncertain. Once regarded as a disease of temperate climates,rheumatic fever is now more common in the tropics, especially in developingcountries. Certain ethnic groups, such as the Maoris in New Zealand, seempredisposed to rheumatic fever at all socioeconomic levels. Most other racialor ethnic differences in incidence are attributed to socioeconomic statusand environmental factors such as overcrowding and poor housing. It hasbeen known for over 100 years that certain families are prone to rheumaticfever regardless of socioeconomic circumstances, suggesting that heredityplays a role.3,4 In 30% to 50% of families with an index case,another member was subsequently affected.5,6
The epidemiology of rheumatic fever is linked to the epidemiology ofstreptococcal pharyngitis. Rheumatic fever occurs most often during thespring, following the peak period of strep pharyngitis.
The advent of antibiotics and improving environmental conditions andsocioeconomic status are chiefly responsible for the decline in incidenceand death rate from rheumatic fever in the US. The outbreaks since the 1980s,mostly among children of middle or high income families, are probably relatedto a change in virulence of the streptococcus organism.
Pathogenesis: Still something of a mystery
Despite years of intensive investigation, the exact pathogenesis of rheumaticfever and rheumatic heart disease remains unknown. Rheumatic fever is generallyconsidered to be an inflammatory disorder of connective tissue--an autoimmuneresponse to untreated GABHS pharyngitis in a genetically predisposed host.
Streptococcal characteristics. Streptococci are classifiedaccording to the type of hemolysis produced by growth on sheep blood cellagar. b-hemolytic streptococci produce a clear zone around colonies. Serogroupsof b-hemolytic streptococci are based on carbohydrate moieties in the cellwall. Of the 20 serogroups (A to T), only group A causes rheumatic fever.
The group A b-hemolytic streptococcus is composed of cytoplasm coveredby a cell membrane consisting predominantly of lipoproteins. The cell wallsurrounding the cell membrane has three layers. The outer layer containsthree proteins--M, R, and T. The M protein primarily determines virulencebecause it inhibits phagocytosis. More than 80 forms of M protein exist,allowing antigenic differentiation by M serotypes. Specific serotypes areconsidered rheumatogenic because of their association with outbreaks ofrheumatic fever. Types 1, 3, 5 , 6, 18, 19, and 24 are the strains mostresponsible for rheumatic fever in the US, whereas others seem to be theculprits in other areas of the world. Rheumatogenic strains adhere to oraland pharyngeal cells of patients with rheumatic fever.
Some strains are surrounded by a mucoid capsule, which enhances virulenceby resisting phagocytosis. Strains recovered during past outbreaks of clinicallysevere rheumatic fever were heavily encapsulated in this way.
Group A streptococci also produce extracellular enzymes, of which streptolysinO is the best known. Antibodies to this enzyme are the basis for one ofthe most important diagnostic tests for recent streptococcal infection,the antistreptolysin-O (ASLO) titer.
Host characteristics. Acute rheumatic fever occurs at thesame rate in boys and girls between 6 and 15 years of age. It is rare inchildren younger than 5 years of age. In families prone to the disorder,it is difficult to distinguish the effects of lifestyle factors such asovercrowding and poor medical care from those of heredity.
Data obtained from a military population during an epidemic suggestedthat only 2% to 3% of untreated cases of streptococcal pharyngitis resultedin first cases of rheumatic fever.7 A 1961 study reported a significantlylower attack rate (0.4%) in children, and the rate may be even lower thanthat in the US today.8 The incidence rises to 50% in individualswith a history of a previous attack.
Antibody titers to group A carbohydrate are significantly higher andmore persistent in patients who develop rheumatic heart disease than inthose who do not.9 This finding may well have a genetic basis.A large proportion of B lymphocyte cells with a specific alloantigen hasbeen found in 99% of patients with rheumatic fever as opposed to only 14%of controls.10 A high incidence of class II human leukocyte antigens(HLA) also has been found in rheumatic fever patients, but variability ofdominant HLA types in different populations makes a definite associationquestionable.
Disease mechanism. Although the genetic pattern of rheumaticfever has not been fully established, it is generally accepted that an immunologicmechanism, either humoral or cellular, is responsible for the injury. Duringa one- to three-week period after apparent recovery from streptococcal phayngitis,antibodies to breakdown products from the bacteria cross-react with molecularlysimilar host tissue in the heart, joints, and central nervous system.11,12The cross-reactive antibodies return to a normal level only after severalmonths to years.
Macrophages, mononuclear cells, and fibroblasts are found in rheumaticheart valves. T-cell subpopulations have been identified in valve tissueremoved from patients. T cells react predominantly to valve tissue ratherthan myocardium, which corresponds to the clinical course of rheumatic heartdisease. One theory proposes that the cellular response causes the cardiaceffects of the disease, while the humoral response accounts for the otherclinical manifestations.
Diagnostic criteria and clinical characteristics
Acute rheumatic fever is a self-limited, multisystem disease that canaffect the heart, joints, brain, and cutaneous and subcutaneous tissues.Cardiac damage is the only potentially chronic debilitating effect. Theclinical presentation varies greatly from patient to patient. Diagnosisrests on the Jones criteria first published in 1944.13 To promoteuniformity in diagnosis, Jones proposed a set of criteria based on whathe termed the major and minor clinical and laboratory manifestations ofrheumatic fever. The criteria were revised in 1992 by the American HeartAssociation's Committee on Rheumatic Fever and Bacterial Endocarditis andKawasaki Disease of the Council on Cardiovascular Disease in the Young (Table1).14 In the absence of a specific diagnostic test for rheumaticfever, the revised criteria serve as guidelines for making the diagnosis.

The presence of two major criteria, or one major and two minor criteria,is considered highly indicative of the diagnosis if clearly supported byevidence of a recent streptococcal infection (increased or rising ASLO titer,recent scarlet fever, or a positive GABHS throat culture). Arthralgia cannotbe considered a criterion in patients with true arthritis.
Since a positive throat culture or rapid streptococcal antigen test mayreflect colonization rather than recent or current infection, these criteriafor streptococcal involvement are less adequate than rising antibody titers.If the ASLO titers are not suggestive, antibodies to deoxyribonuclease B,hyaluronidase, or streptokinase may be used.
Clinical manifestations usually show up one to three weeks after theonset of pharyngitis. Their severity can vary greatly, depending on thesystems affected.
Arthritis. Migratory polyarthritis is the most common,but least specific, of the major criteria, occurring in approximately 70%of patients. To make the diagnosis of arthritis, active joint inflammationmust be present. A "hot joint" is characterized by pain, swelling,tenderness, erythema, and heat. Large joints--knees, elbows, ankles, wrists--areoften the ones involved, with affected areas "migrating" fromjoint to joint. Rapid relief with salicylate therapy (usually within 48hours) is very characteristic of the arthritis and is often considered diagnosticof a rheumatic joint. Rheumatic fever never causes permanent joint damage,and the persistence of arthritis or arthralgia beyond the acute phase castsdoubt on the diagnosis.
Carditis occurs in about 50% of cases, although it hasbeen reported in as many as 75%. It is the major contributor to the overallmorbidity and mortality of rheumatic fever and varies widely in severity.Endocardial (mitral and aortic valves), myocardial, and pericardial involvementmay occur. Endocardial involvement with auscultatory evidence of mitralor aortic valve insufficiency is required for diagnosis. Isolated myocardialor pericardial involvement should not be considered rheumatic.
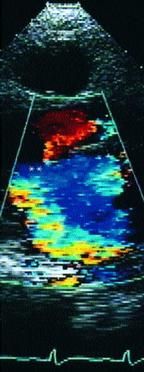
Mitral insufficiency is characterized by a high-frequency blowing apicalholosystolic murmur. An associated low-pitched mid-diastolic apical murmurmay be noted, representing increased mitral valve flow in diastole resultingfrom significant regurgitation. A high-frequency decrescendo diastolic murmurat the right base and left sternal border is the sign of aortic insufficiency.Aortic valve involvement almost never occurs without mitral valve involvement.
Although the Jones criteria specify clinical auscultatory evidence forthe diagnosis of mitral and aortic insufficiency, more and more reportsdiscuss subclinical carditis, in which mitral insufficiency is noticeableonly on echocardiogram. Several investigators have concluded that two-dimensionalechocardiography using color and pulsed Doppler imaging are useful in identifyingsubclinical lesions and offer a valuable addition to current diagnosticcriteria (Figures 1 and 2). It has been suggested that such evidence beadded to the list of minor criteria, but at present, the use of echocardiographyto diagnose carditis remains controversial.1517 It doesnot appear that echocardiographic findings signify an increase in the incidenceof rheumatic fever, but rather an improvement in detection of subclinicalcarditis.


Chorea. Sydenham's chorea occurs in about 10% of casesof acute rheumatic fever. It may be a late manifestation, developing somethree months after the initial illness. Sydenham's chorea must be differentiatedfrom other hyperkinetic movement disorders such as essential tremors, hereditarychorea, or drug-induced and toxic forms.
Chorea is characterized by purposeless, involuntary movements of facialand skeletal muscles as well as generalized weakness and emotional lability.Other features include "milkmaid's grip," "spooning,"and "hung-up reflexes." Chorea most often subsides in five to15 weeks but may recur for as long as two years. Because it is often a latefinding, the acute phase reactants may not be elevated.
Sydenham's chorea may be the sole manifestation of rheumatic fever. Insuch cases, echocardiographic evidence of mitral or aortic insufficiencymay help make the diagnosis.
Erythema marginatum is rare, occurring in only 4% of cases.The rash, which appears on the trunk and proximal extremities, is red withserpiginous margins and central clearing and spreads centrifugally. It isneither raised nor pruritic. A warm bath or contact with hot towels characteristicallyaccentuates it. It is difficult to detect in dark-skinned patients.
Subcutaneous nodules. Subcutaneous nodules also occur rarely,in fewer than 5% of cases. They appear as small nontender, firm, movablemasses, usually palpable over the extensor surfaces of the elbows, wrists,and knees. They also may be found along the spine and in the suboccipitalarea. They almost always appear in association with severe forms of carditis.
Minor criteria. The minor Jones criteria-arthralgia, fever,elevated acute phase reactants, and prolonged PR interval-are not at allspecific for rheumatic fever. They provide additional clinical and laboratoryevidence of the diagnosis and are used only in conjunction with the majorcriteria.
Previous streptococcal infection. In addition to the majorand minor Jones criteria, conclusive evidence of a preceding streptococcalinfection must be present to confirm the diagnosis of rheumatic fever. Apositive throat culture does not distinguish between true infection andthe carrier state. Rapid antigen tests, while highly specific for the presenceof the streptococcus, also cannot distinguish the carrier state. A risein antistreptococcal antibodies is a far more reliable indicator of a recentinfection.
Single ASLO titers of 320 Todd units in children are generally acceptedas a true indication of recent streptococcal infection. A low titer necessitatesevaluation of other streptococcal antibody titers-antideoxyribonuclease,antistreptokinase, or antihyaluronidase. Slide agglutination tests, suchas the Streptozyme test, are not considered definitive and should not beused to confirm a previous streptococcal infection.
Treating rheumatic fever
Figure 3 presents an overview of the management of acute rheumatic fever.Once the diagnosis has been confirmed, treatment to eradicate the streptococcus,even when throat cultures are negative, is indicated. An intramuscular injectionof 1.2 million U of long acting benzathine penicillin G should be administeredto children over 27 kg (60 lb). (Children under 27 kg should receive 600,000U.)

Aspirin remains the anti-inflammatory agent of choice and should be startedas soon as the diagnosis is suspected, while waiting for the laboratorytest results. It often relieves pain dramatically, even after only a doseor two. The usual therapeutic dose is 75 to 100 mg/kg/day every four tosix hours. Serum salicylate levels should be between 15 and 25 mg/100 mL.Once a good clinical response occurs, the dose can be reduced by about 50%over the course of a week. Treatment continues for three to four weeks andmay be discontinued when the sedimentation rate starts to decrease. Whencarditis is present, six to eight weeks of treatment may be required. Althoughother nonsteroidal anti-inflammatory agents have been substituted for aspirinin some cases, no data support their use specifically for rheumatic fever.
Corticosteroids are recommended only in special situations--primarilywhen severe carditis with congestive heart failure (CHF) occurs. Steroidscan quickly relieve these symptoms and control heart failure unless it resultsfrom severe mechanical dysfunction of the mitral or aortic valve, in whichcase surgical repair of the valve may be the only recourse. A two- to four-weekcourse of prednisone (2 mg/kg/day) is recommended. In cases of severe CHF,digitalis, diuretics, and afterload reducing agents should be added to theregimen. Steroids also may be given in the rare case of profoundly symptomaticarthritis unresponsive to conventional aspirin therapy. Aspirin should begiven while tapering steroids to prevent clinical rebound.
Although anti-inflammatory treatment may alleviate the clinical symptoms,shorten the course, and improve the outcome and prognosis of acute rheumaticcarditis, it has not proved at all useful in preventing or mitigating theresidual long-term cardiac sequelae. Cardiac sequelae are related to theseverity of cardiac involvement during the acute attack.
Patients with Sydenham's chorea require a quiet room and may need sedation.Haloperidol is often used to control the abnormal movement. Patients withconcurrent acute inflammation should also take aspirin.
Preventing recurrences
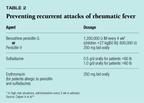
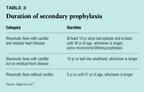
Rheumatic fever may recur with subsequent streptococcal infections. Patientswho have already had recurrences are at greater risk than those who havesustained only a single attack, for whom the risk for recurrence generallydecreases with time. In 1995 the Council on Cardiovascular Disease in theYoung of the American Heart Association offered recommendations for preventingrecurrent attacks of rheumatic fever (Tables 2 and 3).18 Penicillin,given IM or orally, is the agent of choice, with sulfadiazine and erythromycinas substitutes when penicillin cannot be used. Oral penicillin is recommendedonly for patients at low risk for recurrence who are known to comply withmedication schedules.
Confusion has arisen over prophylaxis for rheumatic fever and bacterialendocarditis. Patients with cardiac valve damage from rheumatic fever requireendocarditis prophylaxis for specific procedures in addition to ongoingrheumatic fever prophylaxis.
Sequelae: The heart of the matter
The heart is the only organ subject to major long-term damage from rheumaticfever, and the primary aim of efforts to prevent recurrences of the diseaseis to eliminate cardiac sequelae. Mild mitral insufficiency occurring asthe sole cardiac manifestation during the acute attack will often disappear.Only 30% of patients with mild mitral valve disease have clinical evidenceof the problem one year later. Aortic insufficiency occurring during theacute attack, however, leads to permanent disease in 90% of patients. Ineffect, all patients who develop severe congestive failure will continueto have long-term cardiac problems.
Vigilance, the price of prevention
Documented outbreaks of rheumatic fever continue to be reported, andwe cannot afford to relax our preventive efforts. Physicians must remaincompulsive in treating GABHS upper respiratory infections with appropriateantibiotics. Because prevention is not always possible, especially wheninfection is subclinical or patients with symptoms of an upper respiratorytract infection do not seek medical care, pediatricians also must maintaintheir skills in diagnosing and treating rheumatic fever.
DR. STEEG is Director, Division of Pediatric Cardiology, Albert EinsteinCollege of Medicine and Children's Medical Center at Montefiore, Bronx,NY.
DR. WALSH is Professor of Clinical Pediatrics, Division of PediatricCardiology, Albert Einstein College of Medicine and Children's Medical Centerat Montefiore.
DR. GLICKSTEIN is Associate Professor of Clinical Pediatrics, Divisionof Pediatric Cardiology, Albert Einstein College of Medicine and Children'sMedical Center at Montefiore.
REFERENCES
1. Veasy LG, Tani LY, Hill HR: Persistence of acute rheumatic feverin the intermountain area of the United States. J Pediatr 1994;124:9
2. Hosier DK, Craenen JM, Teske DW, et al: Resurgence of acute rheumaticfever. Am J Dis Child 1987;141:730
3. Wilson MG, Schweitzer MD: Rheumatic fever as a familial disease.Environment,communicability and heredity in their relation to the observedfamilial incidence of the disease. J Clin Invest 1937;16:555
4. Guilhorne L, Weidebach W, Kiss MH, et al: Association of humanleukocyte class H antigens with rheumatic fever or rheumatic heart diseasein a Brazilian population. Circulation 1991;83:1995
5. St. Lawrence W: The family association of cardiac disease, acuterheumatic fever, and chorea. JAMA 1922; 79:2051
6. Faulkner JK, White PD: The incidence of rheumatic fever, chorea,and rheumatic heart disease. JAMA 1924;83:425
7. Rammelkamp CH, Denny FW, Wannamaker LW: Studies in the epidemiologyof rheumatic fever in the armed services, in Thomas L (ed): RheumaticFever. Minneapolis, University of Minnesota Press, 1952, p 72
8. Siegel AC, Johnson, EE, Stollerman GH: Controlled studies of streptococcalpharyngitis in a pediatric population: 1. Factors related to the attackrate of rheumatic fever. N Engl J Med 1961;265:559
9. Dudding BA, Ayoub EM: Persistence of group A antibody in patientswith rheumatic valvular disease. J Exp Med 1968;128:1081
10. Khanna AK, Buskirk DR, Williams RC Jr, et al: Presence of a nonHLAB cell antigen in rheumatic fever patients and their families as definedby a monoclonal antibody. J Clin Invest 1989;83:1710
11. Bronze MS, Dale JB: The re-emergence of serious group A streptococcalinfections and acute rheumatic fever. Am J Med Sci 1996;311:41
12. Husby G, Van de Rijn I, Zabriskie JB, et al: Antibodies reactingwith cytoplasm of the subthalamic and caudate nuclei neurons in chorea andacute rheumatic fever. J Exp Med 1976;144:1904
13. Jones TD: Diagnosis of rheumatic fever. JAMA 1944;126:481
14. Special Writing Group of the Committee on Rheumatic Fever, Endocarditis,and Kawasaki Disease of the Council on Cardiovascular Disease in the Young,American Heart Association: Guidelines for the diagnosis of rheumatic fever:Jones criteria, updated 1992. Circulation 1992;87:302
15. Folger GM Jr, Hajar R: Doppler echocardiographic findings of mitraland aortic valvular regurgitation in children manifesting only rheumaticarthritis. Am J Cardiol 1989;63:1278
16. Folger GK, Hajar R, Robida A, et al: Occurrence of valvular heartdisease in acute rheumatic fever without evident clinical carditis: Colorflow Doppler identification. Br Heart J 1992;67:434
17. Vasan RS, Shrivastava S, Vijayakumar K, et al: Echocardiographicevaluation of patients with acute rheumatic fever and rheumatic carditis.Circulation 1994;1:73
18. Dajani A, Taubert K, Ferrieri P, et al: Treatment of acute streptococcalpharyngitis and prevention of rheumatic fever. A statement for health professionals.Pediatrics 1995;96:758
Carl Steeg, Christine Walsh, Julia Glickstein. Rheumatic fever: No cause for complacence. Contemporary Pediatrics 2000;1:128.