Screening adolescents for depression
Pediatric primary care providers who screen, identify, and treat adolescents for depression and its comorbidities can make a positive difference in their patients’ long-term health, social functioning, and interpersonal relationships.
Depressed adolescents experience emotional suffering, problems in daily living and functioning such as impairment in social and interpersonal relationships.1 Many parents ask their pediatrician about their adolescent’s moodiness as well as potential misuse of substances. Because depressed adolescents often present with physical complaints, providers are in an important position to help screen and identify depression so that adolescents receive proper assessment and appropriate care. In addition, because adolescents with chronic diseases are at increased risk for developing depressive disorders when compared with the general population, it is particularly important that providers be well informed and use appropriate screening tools for depression.
It has been reported that as many as 50% of cases of major depression are missed because of the absence of screening by family physicians.2 In recognition of the fact that depression goes undetected in many adolescents, organizations such as the American Academy of Pediatrics and the US Preventive Services Task Force (USPSTF) recommend routine screening for depression in adolescents and having a system in place to handle positive screenings.
This article reviews the criteria for adolescent depressive disorders, provides information on depression screening tools that can be used in everyday practice, and concludes with practical considerations in the implementation of screening.
Differential diagnosis
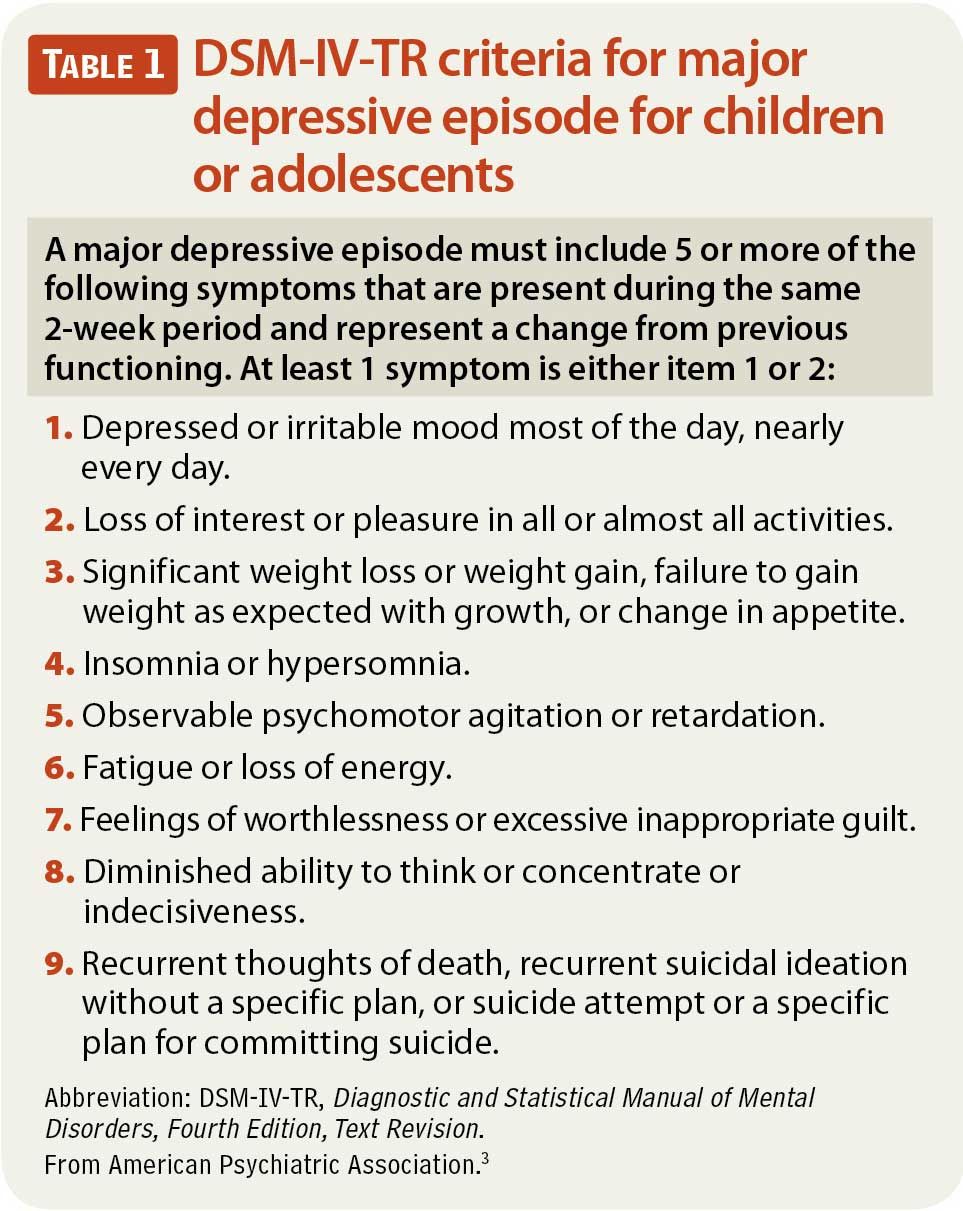
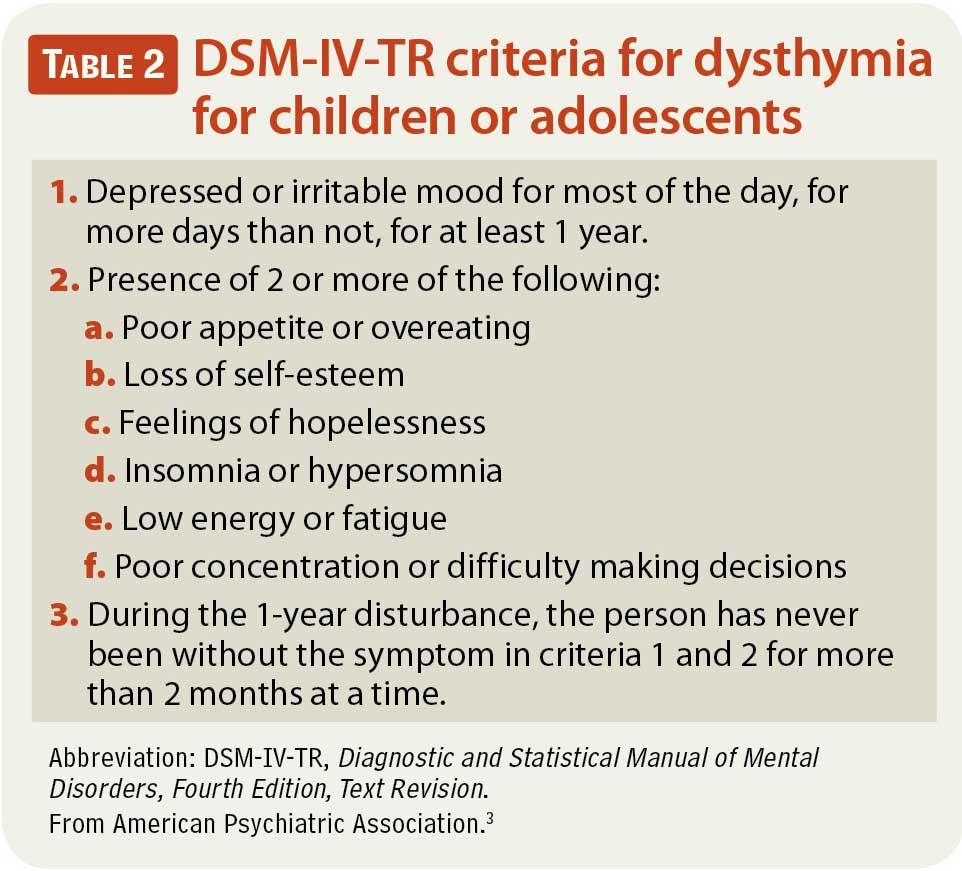
Most screening tools focus on severity of depressive symptoms, yielding a continuous score (with cutoff values for differentiating youth at risk from those not at risk), rather than on diagnostic criteria for depression. An understanding of the diagnostic criteria, however, can help pediatric primary care providers distinguish between different presentations of depression. Depressive disorders are classified under major depressive disorder, dysthymia, and adjustment disorder with depressed mood in the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR). Major depressive disorder requires the presence of a major depressive episode (Table 1).3 It also includes significant impairment in functioning, which for adolescents includes interference with daily routines, school performance, and social relationships. Dysthymia is characterized by having depressed mood that is generally less severe but lasts longer in duration; that is, at least 1 year (Table 2).3 Lastly, although depressive disorders and adjustment disorders overlap in the presentation of depressed mood, adjustment disorders are related to external stressors with symptoms emerging within 3 months of the stressor onset but not persisting longer than 6 months after cessation of the stressor.4 Irritability has been identified as the most common symptom of depression among adolescents and may be an expression of depressed mood in adolescents.
Prevalence
Transient depressive symptoms are common among typically developing adolescents, but adolescents with clinical depression, including major depressive disorder and dysthymia, experience a pervasive unhappy mood that is more severe than the occasional blues. The prevalence of depression increases with age. For example, the rates of major depression in preadolescent children are only 2%, but the rates increase 2- to 3-fold by adolescence and into adulthood.5 Specifically, for adolescents aged 14 to 18 years, the rate of major depression ranges from 4% to 7%.6 The average age for the first onset of depression is between the ages of 13 and 15 years, with some studies citing 14.9 years as the mean age of onset.7 Many longitudinal studies indicate an extremely high rate of recurrence of depressive episodes, showing that as many as 60% to 70% of depressive episodes in adolescents recur within a year.8 Depressive episodes by age 15 are considered “early-onset” and are associated with a more chronic and debilitating course of the disorder.9
Gender differences and comorbidities
As youth move through puberty and into adolescence the rate for depression increases for both boys and girls, but the rate of rise is more dramatic for girls, resulting in a 2:1 female-to-male prevalence.10 Family history of depression, family substance use disorders, and family conflict are important risk factors for youth depression.
Depression in adolescence rarely occurs in isolation. Approximately two-thirds of adolescents with depression have at least 1 comorbid psychiatric disorder and 10% to 15% have 2 or more comorbidities. The most common comorbid disorders in adolescents with major depressive disorder are anxiety disorders and specific phobias.11 Conduct disorder, dysthymia, attention-deficit/hyperactivity disorder (ADHD), and substance use disorders are also common in adolescents with depression.12 If adolescent depression co-occurs with self-harm or problematic substance use, providers should consider this a warning sign for increased self-harm and/or suicide risk.
Screening for depression
Given that depression is a widely prevalent but treatable condition among adolescents that creates long-term social, emotional, and economic burdens for the individual and the family, screening for depression is essential to ensure accurate diagnosis, follow-up, and effective treatment planning. The American Medical Association’s Guidelines for Adolescent Preventive Services (GAPS) and Bright Futures suggest that primary care providers in pediatric settings begin
screening for depression at age 11 and continue to do so annually thereafter.13,14 In addition the USPSTF now recommends depression screening in children and adolescents aged 12 to 18 years for major depressive disorder when systems are in place to ensure accurate diagnosis, psychotherapy, and follow-up.15 Even seemingly asymptomatic adolescents should be screened because depression may go unrecognized. The most widely used and recommended screening approaches and tools are discussed herein.
Physician interviews and forms
GAPS. GAPS provides templates and forms related to child and adolescent preventive services that can be utilized by all providers. Using these forms, providers are able to identify whether an adolescent is at risk for experiencing depression and also to inquire about suicidality. Age-specific GAPS forms are available for younger adolescents, middle/older adolescents, and parents, and can be found for free through the main GAPS Web site: http://www.ama-assn.org/ama/pub/physician-resources/public-health/promoting-healthy-lifestyles/adolescent-health/guidelines-adolescent-preventive-services.page.
HEEADSSS. A thorough psychosocial evaluation can yield important information, including the opportunity to gather specific information about depressive symptoms. An example of an evaluative approach that can be used in a pediatric primary care setting is the Home, Education and employment, Eating, Activities with peers, Drugs, Sexual activity, Suicide and depression, and Safety (HEEADSSS) assessment. This acronym is used to prompt providers to ask adolescents about each of these areas of risk. The symptoms of depression can be subtle; depression may be missed if providers do not explicitly ask about depression while under the assumption that adolescents appear to be doing well. Questions about suicidality naturally follow depression-specific questions. Providers should keep in mind that a trustworthy relationship with the adolescent is essential for openness and honesty.
When using either the GAPS guidelines or the HEEADSSS assessment, an adolescent might endorse having suicidal thoughts. Therefore providers should be ready to address suicidality directly, assess thoroughly for safety, and take action if needed. Questions that may be asked of the adolescent are: “Have you had thoughts of dying or death?”; “Have you harmed yourself?”; and “Do you have a plan?” Asking such questions is essential to clarify the adolescent’s risk for harm and will assist in developing a safety plan if needed.
Questionnaires
There are a variety of options for structured questionnaires that screen for adolescent depressive symptoms, as well as many that screen for general adolescent mental health. The tools listed here are not exhaustive, but do represent the most commonly used depression measures in primary care settings. Important information such as cost, time to administer, completion time, applicability to specific age groups, cutoff scores, and how to obtain them is provided for each screening questionnaire. It is recommended that providers choose a screening option that best fits the needs of their practice, considering their own clinical and patient population.
Depression-specific questionnaires.
Mood and Feelings Questionnaire (MFQ). The MFQ is a 32-item measure that consists of questions regarding how the adolescent has been feeling or acting within the past 2 weeks.16 A short version is also available that consists of 11 items and usually takes about 5 to 10 minutes to complete. For adolescents, the cutoff score on the full version for distinguishing those who are likely to have a depressive disorder from those who are not is 12 or higher. The MFQ can be used with children aged 8 to 17 years, and also has a parent version that can be used to assess symptoms based on parental report. The MFQ can be downloaded free at http://devepi.duhs.duke.edu/mfq.html.
Patient Health Questionnaire (PHQ-9). The PHQ-9 was originally developed for adults in primary care, with 9 items directly related to each of the criteria listed in the DSM-IV-TR for major depression. The PHQ-9 has been strongly supported for its applicability as a screening tool for adolescent depression in primary care as well as in pediatric hospital settings.17 The PHQ-9 takes approximately 5 to 10 minutes to complete. The optimal PHQ-9 cutoff score for adolescents is 11 or higher; it has been shown to have a sensitivity of 89.5% and specificity of 77.5% compared with a diagnosis of major depression on a structured mental health interview.18 There are also algorithms to use to determine if the adolescent meets diagnostic criteria for major depressive disorder or dysthymia. The PHQ-9 is free and available to the public: http://www.agencymeddirectors.wa.gov/Files/depressoverview.pdf.
In addition, the PHQ-2, a very brief depression screening scale consisting of the first 2 items of the PHQ-9, has been found to have good sensitivity and specificity for detecting major depression.19 The PHQ-2 may be used as a first step for screening. Adolescents who screen positive on the PHQ-2 may be further administered the rest of the PHQ-9.
Beck Depression Inventory (BDI)-II. The BDI-II is a 21-item instrument for detecting depression that can be completed by adolescents aged 13 years and older. The BDI-II aligns with the depressive symptom criteria of the DSM-IV-TR and takes about 10 minutes to complete. It was specifically constructed to measure the severity of self-reported depression in adolescents and adults.20 Although the BDI-II is typically a self-report measure, providers can also verbally administer the measure to adolescents. It contains 21 questions with a scale value of 0 to 3. A cutoff score above 20 suggests moderate depression and a score of 29 or higher suggests severe depression. The BDI-II can be used with patients aged 13 to 80 years and is available in Spanish. The BDI-II can be ordered at http://www.pearsonassessments.com and costs $120 for a kit including a manual and 25 forms.
Children’s Depression Inventory (CDI)-2. The CDI-2 is a 28-item scale used to assess for depressive symptoms in children and adolescents. It is derived from the BDI but modifies some questions to be more appropriate for younger ages.21 The CDI-2 is a self-report measure that is completed by the child or adolescent and usually takes about 15 to 20 minutes. It can be administered and scored using paper-and-pencil forms or online. It asks about key symptoms of depression, such as a child’s feelings of worthlessness and loss of interest in activities. The 28 items of the CDI-2 yield a total score, 2 scale scores (emotional problems and functional problems), and 4 subscale scores (negative mood/physical symptoms, negative self-esteem, interpersonal problems, and ineffectiveness). Each item allows the patient to respond to 3 choices that indicate 3 levels of symptoms: 0 (absence of symptoms), 1 (mild or probable symptoms), or 2 (definite symptoms). The CDI-2 can be used with patients who are aged 7 to 17 years, and can be particularly helpful for providers who want to track depressive symptoms over the course of treatment (http://www.mhs.com/CDI2). The CDI-2 can be obtained through http://www.pearsonassessments.com at a cost of $267 for a manual and 25 forms.
General mental health questionnaires
Pediatric Symptom Checklist (PSC). The PSC is a 35-item psychosocial screening tool designed to cover cognitive, emotional, and behavioral problems. It is completed by the parent and takes approximately 3 minutes. The PSC can be used with patients aged between 3 and 16 years. There is a total possible score of 70. For children aged 6 to 16 years, a total score of 28 or higher indicates significant impairment in functioning. The PSC has an internalizing scale that examines depression and anxiety together. For adolescents who are aged at least 11 years, there is also a youth self-report version (Y-PSC). Additionally the PSC and Y-PSC are available in Spanish, and the PSC is available in Japanese. There is also a 17-item scale that performs similarly to the 35-item scale, although this shorter version has not been as widely used. The PSC can be downloaded free at http://psc.partners.org/psc_order.htm. Scoring time is relatively brief and could be completed during the office visit. Response options within each category are added together and cutoff scores then indicate if there is significant psychosocial impairment.
Youth Self-Report Scale (YSR). The YSR is a youth version of the Child Behavior Checklist that consists of 112 items. The YSR can be used with adolescents aged 11 to 18 years and is meant to screen for a variety of behavioral concerns including depression, anxiety, attention problems, aggressive behavior, and social problems. The completion time for the YSR can be 15 minutes or longer because of the large number of questions. Therefore the YSR may be most useful when a provider wants to get a full picture of the adolescent or suspects other areas of concern in addition to depression. Responses on the YSR are added together and a t-score is derived and compared to normative responses of children who are the same age and gender. If t-scores are above the 98th percentile, they are considered to be in the clinical range and the child should be further evaluated. The YSR has also been translated into various languages including Spanish, Chinese, and Japanese. The YSR can be ordered at http://www.aseba.org/ and costs $25 for a package of 50 forms. Separate scoring software is available for purchase, and with the software the scoring time averages 10 minutes. Because of the need to score with software or use of more involved manual methods, results of the YSR may be more difficult to complete during a clinic visit.
Practical concerns about depression screening and follow-up
The USPSTF emphasizes the importance of implementing screening only when such screening is supported by systems that can assist with further evaluation, including confirming the diagnosis and initiating evidence-based treatments. Thus providers and clinics need to be certain when they institute screening that systems are in place to review screening results and take the next appropriate steps. Among the practical considerations to creating screening protocols, clinics need to determine which staff would be responsible for administering, scoring, and recording the questionnaire, as well as ordering and maintaining the screening supplies. A second consideration is when the screening questionnaire will be administered. For example, should it be administered to the adolescent in the waiting room prior to seeing the primary care provider, or in the room with the provider? If adolescents are asked to complete questionnaires in the waiting room, privacy needs to be ensured, as adolescents may feel uncomfortable answering the questions when their parents or others are present. Providers should explicitly discuss confidentiality expectations with parents and adolescents. Although confidentiality laws vary by state, the National Alliance to Advance Adolescent Health provides a good resource for adolescent confidentiality: http://ww2.nasbhc.org/RoadMap/CareManagement/Special Topics/State Policies and Confidential Care for Adolescents NAAAH.pdf.
During the course of depression screening the adolescent may disclose information about suicidal thoughts, intents, or plans. For a patient who indicates any suicidality, providers should be prepared to complete a thorough assessment prior to the adolescent leaving the room to ensure his or her safety. For a patient with suicidal thoughts but no plan or intent, a safety plan may be appropriate in which the adolescent agrees to stay safe and has a plan in place to seek assistance (from a trusted adult or the provider) if his or her suicidal thoughts worsen while the provider finds mental health specialty care. It is also important that providers counsel the parents and family of any suicidal adolescent to safeguard the home from medications, weapons, and lethal objects. Prior to assessment, providers should have an understanding of the resources available in their community if further assessment is warranted. The Centers for Disease Control and Prevention includes useful information on safety planning and resources on its Web page for suicide prevention in youths: https://www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/SuicideYouth.html.
Active monitoring for mild depression
After assessment for depressive symptoms has been conducted with the assessment tools previously discussed, a provider will have information about the level and severity of the adolescent’s symptoms. If an adolescent endorses symptoms that are consistent with mild depression, providers should engage in active monitoring practices according to the Guidelines for Adolescent Depression-Primary Care (GLAD-PC; http://glad-pc.org/). This is important because more than half of adolescents who screen positive for depression will have resolution of their symptoms without requiring psychotherapy or medications.22 Active monitoring is analogous to watchful waiting practices used in adult populations. Key aspects of active monitoring as emphasized by the GLAD-PC guidelines include increasing the frequency of follow-up visits, encouraging the adolescent to engage in regular exercise and activities, and identifying peer and adult support.23,24 Providers should also involve parents and engage them in being aware of their child’s symptoms and assisting in problem solving. Adolescents who are treated with active monitoring and who have persistent symptoms 6 to 8 weeks after screening should then receive evidence-based treatment for depression with regular follow-up visits until their symptoms have resolved.
Evidence-based treatment for moderate-to-severe depression
If an adolescent endorses symptoms consistent with moderate-to-severe depression, providers should discuss different treatment options, including psychotherapy, medication, or both. Evidence-based psychotherapies for adolescent depression exist; the most common treatments include cognitive-behavioral therapy (CBT) and interpersonal psychotherapy for adolescent depression (IPT-A), both of which have shown effectiveness in treating children and adolescents with depression.25,26 Behavioral activation (BA) is also a promising treatment that has been adapted to treating adolescent depression.27 Providers should be ready with referrals to therapists who can provide these psychotherapeutic treatments.
In advance of implementing screening, clinics can create a list of potential resources for psychological treatment so that this information is readily available when needed. Medication for depression may also be indicated as part of treatment. Specifically, selective serotonin reuptake inhibitors (SSRIs) have proven effective in reducing symptoms of depression in adolescents.28 Any adolescent who is started on antidepressants such as SSRIs, as well as his or her parents, should be counseled for the potential increased risk for suicidality and monitored closely in the beginning of medication treatment. Because medications and psychotherapy have similar efficacy, one reasonable approach would be to work with patients and families to determine their treatment preferences and needs of the adolescent. Similar to active monitoring, the key to the use of evidence-based treatments is to monitor adolescents closely and to advance treatment for those who are not improving after 6 to 8 weeks of treatment. If multiple treatment providers are involved in managing the depression, obtaining a waiver of confidentiality to allow communication on progress and needs is ideal.
Summary
Screening for adolescent depression can make a difference to adolescent health. The tools and resources described herein are intended to equip providers with the resources to conduct screening and follow-up with adolescent populations in primary care.
REFERENCES
1. Daley SE, Rizzo CJ, Gunderson BH. The longitudinal relation between personality disorder symptoms and depression in adolescence: the mediating role of interpersonal stress. J Pers Disord. 2006;20(4):352-368.
2. U.S. Preventive Services Task Force. Screening for depression: recommendations and rationale. Ann Intern Med. 2002;136(10):760-764.
3. American Psychiatric Association. Desk Reference to the Diagnostic Criteria From DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000;168-177.
4.Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. 2012;379(9820):1056-1067.
5. National Institute of Mental Health (NIMH). Breaking ground, breaking through: The strategic plan for mood disorders research of the National Institute of Mental Health. U.S. Department of Health and Human Services. http://www.nimh.nih.gov/about/strategic-planning-reports/breaking-ground-breaking-through--the-strategic-plan-for-mood-disorders-research.pdf. Published January 2003. Accessed June 11, 2013.
6. Costello EJ, Pine DS, Hammen C, et al. Development and natural history of mood disorders. Biol Psychiatry. 2002;52(6):529-542.
7. Lewinsohn PM, Clarke GN, Seeley JR, Rohde P. Major depression in community adolescents: age at onset, episode duration, and time to recurrence. J Am Acad Child Adolesc Psychiatry. 1994;33(6):809-818.
8. Dunn V, Goodyer IM. Longitudinal investigation into childhood- and adolescence-onset depression: psychiatric outcome in early adulthood. Br J Psychiatry. 2006;188:216-222.
9. Hammen C, Brennan PA, Keenan-Miller D, Herr NR. Early onset recurrent subtype of adolescent depression: clinical and psychosocial correlates. J Child Psychol Psychiatry. 2008;49(4):433-440.
10. Wade TJ, Cairney J, Pevalin DJ. Emergence of gender differences in depression during adolescence: national panel results from three countries. J Am Acad Child Adolesc Psychiatry. 2002;41(2):190-198.
11. Seligman LD, Ollendick TH. Comorbidity of anxiety and depression in children and adolescents: an integrative review. Clin Child Fam Psychol Rev. 1998;1(2):125-144.
12. Ford T, Goodman R, Meltzer H. The British Child and Adolescent Mental Health Survey 1999: the prevalence of DSM-IV disorders. J Am Acad Child Adolesc Psychiatry. 2003;42(10):1203-1211.
13. American Medical Association. Guidelines for Adolescent Preventive Services (GAPS): Recommendations monograph. http://www.ama-assn.org/resources/doc/ad-hlth/gapsmono.pdf. Published 1997. Accessed June 11, 2013.
14. Maternal and Child Health Bureau. Bright Futures Web site. http://www.brightfutures.org/. Accessed June 11, 2013.
15. U.S. Preventive Services Task Force. Screening and treatment for major depressive disorder in children and adolescents. http://www.uspreventiveservicestaskforce.org/uspstf09/depression/chdeprrs.htm. Published March 2009. Accessed June 11, 2013.
16. Angold A, Costello EJ. Mood and Feelings Questionnaire (MFQ). Durham, NC: Duke University Health System Center for Developmental Epidemiology; 1987. http://devepi.duhs.duke.edu/mfq.html. Accessed June 11, 2013.
17. Allgaier AK, Pietsch K, Frühe B, Sigl-Glöckner J, Schulte-Körne G. Screening for depression in adolescents: validity of the patient health questionnaire in pediatric care. Depress Anxiety. 2012;29(10):906-913.
18. Richardson LP, McCauley E, Grossman DC, et al. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117-1123.
19. Richardson LP, Rockhill C, Russo JE, et al. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125(5):e1097-e1103.
20. Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588-597.
21. Kovacs M. The Children’s Depression Inventory (CDI). Psychopharmacol Bull. 1985;21(4):995-998.
22. Richardson LP, McCauley E, McCarty CA, et al. Predictors of persistence after a positive depression screen among adolescents. Pediatrics. 2012;130(6):e1541-e1548.
23. Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D; GLAD-PC Steering Group. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): I. Identification, assessment, and initial management. Pediatrics. 2007;120(5):e1299–e1312.
24. Cheung AH, Zuckerbrot RA, Jensen PS, Ghalib K, Laraque D, Stein RE; GLAD-PC Steering Group. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): II. Treatment and ongoing management. Pediatrics. 2007;120(5):e1313-e1326.
25. Watanabe N, Hunot V, Omori IM, Churchill R, Furukawa TA. Psychotherapy for depression among children and adolescents: a systematic review. Acta Psychiatr Scand. 2007;116(2):84-95.
26. Mufson L, Dorta KP, Wickramaratne P, Nomura Y, Olfson M, Weissman MM. A randomized effectiveness trial of interpersonal psychotherapy for depressed adolescents. Arch Gen Psychiatry. 2004;61(6):577-584.
27. Dimidjian S, Barrera M Jr, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;7:1-38.
28. David-Ferdon C, Kaslow NJ. Evidence-based psychosocial treatments for child and adolescent depression. J Clin Child Adolesc Psychol. 2008;37(1):62-104.
MS CORONA is a doctoral student in child clinical psychology, University of Washington, Seattle. DR MCCARTY is research associate professor of pediatrics and adjunct research associate professor of psychology, University of Washington and Seattle Children’s Research Institute. DR RICHARDSON is professor of pediatrics, University of Washington and Seattle Children’s Research Institute. The authors have nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
DSM-5: What you need to know about the new psychiatric diagnostic criteria
The recent release of the American Psychiatric Association’s 5th edition of its Diagnostic and Statistical Manual of Mental Disorders, known as DSM-5, has sparked some controversy. Autism and Asperger syndrome are lumped together. Attention-deficit/hyperactivity disorder symptoms now have up to age 12 years to manifest. New disorders have been added. Existing disorders are recategorized. For community pediatricians, this adds confusion to an already complex patient assessment process.
However, the DSM-5 has much to offer, according to Gary G. Gintner, PhD, associate professor and program leader of the counseling program at Louisiana State University in Baton Rouge. Gintner served as the DSM-5 task force chair for the American Mental Health Counselors Association. The task force reviewed various DSM-5 draft proposals and provided review comments over the past 3 years.
Pediatricians screening for depression need to consider new disorders, including disruptive mood dysregulation disorder (DMDD). The DSM-5 added this disorder to address potential overdiagnosis of bipolar disorder in children. Researchers found that some children diagnosed as bipolar did not develop bipolar disorder as adults, instead being more likely to develop depressive or anxiety disorders. Diagnostic criteria for DMDD include common episodes of severe anger outbursts. Between these outbursts, there is a persistent angry or irritable mood. Symptoms have to appear by age 10 years and last for at least 1 year. “These are pretty significant criteria,” Gintner says, and they can help pediatricians differentiate DMDD from bipolar disorder in children (for which diagnostic criteria are the same as in adults).
The DSM-5 also adds premenstrual dysphoric disorder (PMDD), previously flagged in the DSM-IV appendix, as a new depressive disorder. “It’s not specific to adolescents,” Gintner says, but it can complicate diagnostics if pediatricians do not consider PMDD when screening their female patients for depression.
While the updated manual modifies diagnostic criteria, it also incorporates components to streamline the process. “DSM-5 changes how you diagnose relative to DSM-IV,” Gintner says, through the use of a single axis system similar to the International Classification of Diseases (ICD). Also, ICD-10 codes are noted with every disorder, eliminating the need to look them up.
Other major benefits of the DSM-5 are its numerous assessment tools. Available online at www.psychiatry.org/dsm5, these assessment measures can assist the pediatrician in the diagnostic process and enhance clinical decision making.