Skin lesions that mimic abuse
Is that "bruise" or "burn" really a sign of child abuse? To avoid a misdiagnosis that can have profound consequences for the child, family, and suspected perpetrator, be sure you consider the full range of possibilities.
Cover story
Skin lesions that mimic abuse
Is that "bruise" or "burn" really asign of child abuse? To avoid a misdiagnosis that can have profound consequencesfor the child, family, and suspected perpetrator, be sure you consider thefull range of possibilities.
Lesions of the skin are the most common manifestations of physical childabuse. Inflicted trauma may take the form of bruises, abrasions, lacerations,burns, bites, or hair loss.1 Cutaneous findings are also importantin recognizing children who may have been sexually abused. Genital or perianalbruises, abrasions, petechiae, or edema may suggest acute trauma while papulesor ulcers raise suspicion of sexually transmitted disease.2
In many instances, determining that a skin lesion is the result of abuseis straightforward. Pediatricians must be aware, however, that certain cutaneousdisorders produce lesions that can be misinterpreted as evidence of childabuse.3,4 Failing to consider this possibility may have veryserious consequences. A falsely accused parent may lose custody of a childor face criminal charges.5
To help pediatricians distinguish between skin lesions that are causedby abuse and those that are not, we will review dermatologic conditionsand traditional ethnic medicinal practices that mimic abuse and discusstheir differential diagnoses. We separate the disorders into those thatcan be mistakenfor physical abuse, including bruises, burns, and hair loss,and those that may masquerade as sexual abuse (see table, below). In somecases, we have included vignettes from published reports or our own experienceto describe the clinical presentation and illustrate the impact that anaccusation of abuse may have on a family.
Conditions mistaken for bruises
Soft tissue injuries such as bruises and abrasions are the most frequentsigns of physical abuse.6 The history, distribution, and patternof bruises as well as the child's age and developmental capabilities helpdifferentiate between lesions caused by inflicted or accidental trauma anddermatologic disorders characterized by purpura or hyperpigmentation. Inaddition, hyperpigmented lesions do not exhibit the evolution of color typicalof bruises.
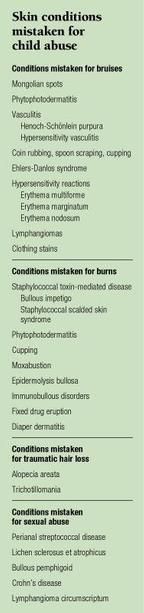
Mongolian spots are blue-gray macules or patches that are usually locatedover the lumbosacral area, although they may appear on the back, shoulders,or extremities (Figure 1). The spots, which result from the deposition ofmelanin in the dermis, are present at birth and tend to fade over severalyears. They are particularly common in African-Americans, Asians, and Hispanicsbut may also occur in white infants.
Because of their color, Mongolian spots have occasionally incited investigationsfor possible child abuse.4,7 The typical location and color ofthe spots, their presence at birth, and their failure to manifest colorprogression should help distinguish them from bruises, however. To minimizeconfusion, it is wise to document the presence and location of Mongolianspots in the patient record.
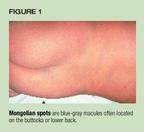
Phytophotodermatitis is a phototoxic reaction that occurs when skin thathas come into contact with certain plants is exposed to sunlight. The reactionis mediated by furocoumarins, a group of psoralen-like compounds that areliberated when the plant is crushed. Although lemons and limes are usuallyresponsible for the reaction, a variety of plants contain furocoumarins,including bergamot, celery, garden carrot, wild carrot, parsley, fennel,and dill.
When exposed to ultraviolet A radiation, the furocoumarins induce hyperpigmentationor, less commonly, an acute dermatitis characterized by erythema or vesicleformation. The reaction occurs several hours to days following exposureand the resulting lesions may have unusual patterns, such as a linear streakingor finger- or handprints (Figure 2).
These configurations may raise concern that the lesions are actuallybruises resulting from physical abuse.8,9 If blisters are present,they may be mistaken for indications of a scald burn. The correct diagnosisis suggested by a careful history, the presence of multiple lesions withunusual shapes, and failure of hyperpigmented lesions to change color asbruises do with time.
Henoch-Schönlein purpura (HSP) is an idiopathic cutaneous necrotizingvenulitis that occurs primarily in children and affects the skin, synovium,gastrointestinal tract, and kidneys. Typically, skin lesions begin as erythematousmacules or papules that evolve to form so-called palpable purpura. In ambulatorypatients, the lesions are located primarily on the lower extremities andbuttocks with sparing of the trunk, palms, and soles (Figure 3). Two-thirdsof children have periarticular swelling and pain, and two-thirds have GIinvolvement--abdominal pain or vomiting.

Although this constellation of symptoms and signs is generally sufficientto permit an accurate clinical diagnosis, atypical presentations have beenconfused with physical abuse.10 In particular, infants with HSPor a closely related condition called acute hemorrhagic edema of infancymay exhibit edema, erythema, or purpura of the face and ears before lesionsappear elsewhere (Figure 4).11

Brown and Melinkovich reported the case of an 8-month-old infant with"red, swollen ears and a facial bruise" that the physician initiallybelieved had resulted from inflictedtrauma. Within 24 hours, however, thechild developed fever and more widespread palpable purpura consistent withHSP.10
Hypersensitivity vasculitis is a group of disorders similar to HSP andcharacterized by involvement of small vessels. The condition results fromthe formation and deposition in the small vessels of immune complexes triggeredby infections and drugs.
A 2-year-old boy was brought to an emergency department by his fatherfor evaluation of purpuric lesions. The physical findings coupled with maternalaccusations of abuse led to the child's hospitalization for evaluation andprotection. A cutaneous biopsy, however, revealed leukocytoclastic angiitis,and a diagnosis of hypersensitivity vasculitis was made.12
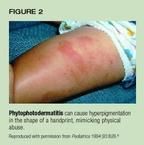
Coin rubbing, spoon scraping, cupping. Several cultural practices usedto treat illness can produce petechiae, purpura, or hyperpigmentation thatmimic physical abuse. Cao gio ("scratch the wind") is the Vietnamesepractice of rubbing the skin with a coin or spoon to alleviate "badwinds" that are presumed to cause fever.13 A medicated oilor ointment is applied to the chest and back after which a coin, spoon,or other object is scraped along the spine, neck, and intercostal spacesuntil petechiae or ecchymoses appear (Figure 5).13 A variantof spoon rubbing, called quat sha, is practiced by the Chinese.14Although many physicians are familiar with these practices, lack of awarenessby some has resulted in allegations of physical abuse.13 (See"Do traditional therapies constitute abuse?" below.)

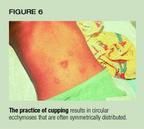
Cupping has been used for centuries to treat a variety of ailments.15In dry cupping, a heated vessel such as an eye cup or shot glass is appliedto the skin of the affected area to "elevate the congestion."The vacuum formed during this maneuver creates suction on the skin thatresults in a circular ecchymosis (Figure 6). Wet cupping is a similar procedurein which the vessel is applied to previously abraded skin.15
Ehlers-Danlos syndrome (EDS) is an inherited disorder with several variants,all characterized by skin laxity and hyperextensible joints. The abnormalcollagen present in patients with EDS results in vascular fragility anda tendency to develop ecchymoses following minor trauma (Figure 7). Multipleor extensive bruises in children not yet diagnosed have resulted in allegationsof physical abuse. Children with EDS also have fragile skin, which predisposesthem to lacerations from minor trauma. These children's frequent lacerationsand many scars have prompted reports of abuse.7

Hypersensitivity reactions. Adler and colleagues reported the cases ofthree children with unexplained, erythematous and ecchymotic macules.16Initially, the presence of purpura with an uncertain history led to concernthat the children had been physically harmed. Over time, however, the lesionsdeveloped a target-like appearance consistent with a diagnosis of erythemamultiforme (EM).16
EM is an acute, self-limited inflammatory disorder that occurs in minorand major forms. EM minor, as the name suggests, is the milder form andis thought to represent a hypersensitivity reaction to drugs or infectiousagents like herpes simplex virus. EM major arises from a toxic injury tothe skin produced, most often, by drugs.
The lesions of EM begin as erythematous macules or papules that are symmetricallydistributed, remain fixed in location, and have a predilection for the extensorsurfaces of the extremities and the palms and soles. As lesions progress,they often take on a target- or ring-like appearance, exhibiting an erythematousmargin with a dusky center that may later develop a central blister or crust(Figure 8). Resolving lesions may appear purpuric.

Children with acute rheumatic fever may develop erythema marginatum,an evanescent eruption composed of erythematous arcs or incomplete circles.This eruption may occasionally be mistaken for the injuries inflicted bystriking with a looped electrical cord.7The fleeting, migratorynature of erythema marginatum and its failure to progress through the colorchanges anticipated of bruises are generally sufficient to distinguish itfrom trauma. The other symptoms of acute rheumatic fever, including feverand arthralgias or swollen joints, also point to the diagnosis.
Erythema nodosum appears as tender, red nodules that typically are locatedon the extensor surfaces of the lower extremities, although the face, solesof the feet, and trunk may be involved (Figure 9). Given the appearanceof the lesions, it is not surprising that this condition has been confusedwith physical abuse.17 Erythema nodosum reflects injury to bloodvessels in the lower dermis and subcutaneous fat that probably results froman immunological response to an infectious agent.

Lymphangiomas are benign malformations of lymph channels that may appearclinically as cystic or vesicular lesions. Cystic forms, sometimes calledcystic hygromas, present at birth or early in life as soft tissue swellingsin the neck, axillae, or groin.18 Williams and colleagues describeda 3-year-old girl with an 8-month history of a "bruise-like lesion"on the right side of the neck. Physical abuse was considered in the differentialdiagnosis, but a cutaneous biopsy demonstrated changes characteristic ofa cystic lymphangioma.19 Although bruising resulting from aninflicted injury might be considered when lymphangiomas first appear, theirpersistent nature and failure to undergo evolution of color should makethis diagnosis untenable.
Clothing dyes, such as the dye from blue jeans, may impart a blue colorto the skin that can be mistaken for bruises. Tunnessen described an 18-month-old girl with apparent "bruising" of the legs thought to be theresult of physical abuse.20 The color was removed with an alcoholswab, however, leading to the correct diagnosis.
Conditions mistaken for burns
Skin lesions that mimic burns can result from a variety of conditionsranging from bacterial infection to folk medicine practices, diaper dermatitis,and drug reactions.
Staphylococcal toxin-mediated disease. Cutaneous infection with strainsof Staphylococcus aureus that produce an epidermolytic toxin causes a spectrumof disease ranging from bullous impetigo to staphylococcal scalded skinsyndrome. The toxin damages the granular cell layer of the epidermis resultingin the formation of flaccid bullae that rupture easily, leaving erosions.
Bullous impetigo is a localized form of toxin-mediated disease. Althoughthe primary lesion is a small vesicle or bulla, these rupture rapidly leavinground erosions that become crusted. Their appearance may be confused withcigarette burns(Figure 10).17 When involvement is more extensive,lesions may mimic scald burns.

A 21-month-old was brought to the pediatric emergency department at ourinstitution with a "rash" on the buttocks, fever, and unwillingnessto walk.21 He had been in the care of a family friend until twodays before the ED visit. When returned to his parents, he had a fever,erythema of the buttocks, and progressive refusal to walk. Examination revealedtwo large, symmetric, superficial crusted erosions overlying the convexitiesof the buttocks (Figure 11). The appearance and location of the lesionsraised concern that the child had suffered a scald burn. Dermatologic consultationand a punch biopsy, however, led to a diagnosis of bullous impetigo.

Staphylococcal scalded skin syndrome, a more extensive form of toxin-mediateddisease, causes large erosions that may be mistaken for burns. The potentialimpact of such confusion is illustrated by the case of a woman who was jailedin New York because her 4-year-old daughter had lesions that cliniciansbelieved to be the result of a scald burn. Charges were dropped when specialistsdetermined that the girl had staphylococcal scalded skin syndrome.22
Phytophotodermatitis. As discussed previously, phytophotodermatitis maybe characterized by erythema or formation of vesicles or bullae. The linearor streaked pattern of these lesions may resemble scald or caustic burns.23
Cupping may produce a burn if faulty technique is employed. To heat acup, alcohol is applied to the inner rim and ignited. If alcohol remainswhen the cup is applied to the skin, a burn may occur.24
Moxibustion. In the traditional Chinese medical practice of moxibustion,cutaneous burns are induced at areas of symptoms or at skin sites that correspondto afflicted organs. Small amounts of the moxa herb are burned on the skin,although cigarettes may be substituted. Children treated in this mannerexhibit acute burns or scars. A clue to diagnosis is that lesions may havea definite pattern of distribution, often around the umbilicus.25In a related practice known as Maqua or Arabian therapeutic burn, hot metalspits are applied to the skin at sites of disease or pain creating deepburns.26
Epidermolysis bullosa (EB) is a rare disorder characterized by blisteringand erosions that may be confused with inflicted burns or poorly cared forimpetigo.27 There are at least 18 types of EB, nearly all ofwhich are inherited. In EB, gene mutations lead to synthesis of defectivestructural proteins. As a result, the epidermis is poorly anchored and patientsdevelop blisters and erosions with minimal trauma.In severe forms, erosionsoccur in the oral cavity and respiratory tract and scarring leads to pseudowebbingof the digits and esophageal stricture.
A 2-year-old girl was referred to the child abuse clinic at our institutionfor evaluation of a "burn." The child had been left for severalhours with a baby-sitter and upon the mother's return was observed to havewhat appeared to be burns on the upper lip and hand. The baby-sitter andthe mother could offer no explanation for how the lesions might have occurred.The physical examination found an erosion on the philtrum and upper lipand a linear erosion on the right hand (Figure 12). These findings werebelieved to be most consistent with a "brand" burn caused by alinear object. A child abuse report was made, but a thorough investigationfailed to document abuse. One month later, the child awoke with a "darkspot" on the face. When the mother attempted to wipe this away, sloughingof skin occurred. A dermatologic consultation and cutaneous biopsy led toa diagnosis of EB simplex.
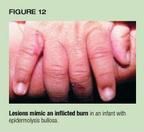
A diagnosis of EB, not abuse, is suggested by a history of blister formationfollowing mild trauma and, depending upon the type of disease, mucosal lesionsand a family history of blistering. Diagnostic confirmation requires a cutaneousbiopsy.
Immunobullous disorders. Immunologically mediated bullous disorders mayalso mimic burns. Both dermatitis herpetiformis and linear IgA dermatosisproduce vesicles that, following rupture, may be confused with cigaretteburns.27,28
Fixed drug eruption is a unique form of drug allergy in which characteristicskin lesions recur at the same location each time an offending agent isingested. This form of cutaneous reaction is observed most commonly in adultsbut may occur in children or adolescents. Clinically, the eruption presentsas solitary or multiple erythematous macules that evolve into edematousplaques. In some patients, bullae form that may be confused with inflictedburns.17 Healing occurs over 10 to 14 days and leaves hyperpigmentationthat may increase in intensity with subsequent exposures to the offendingagent. Many drugs have been reported to cause fixed drug eruptions, butthose most frequently implicated are barbiturates (especially phenobarbital),tetracycline, and sulfonamides.
Diaper dermatitis. Severe irritant diaper dermatitis produces erosionsthat can mimic scald burns.17 Involvement of the convexitiesof the buttocks as well as the perineum and suprapubic region suggests adiagnosis of diaper dermatitis.
Conditions mistaken for traumatic hair loss
Disorders characterized by alopecia may be mistaken for hair pullingas a manifestation of physical abuse. They include alopecia areata and trichotillomania.
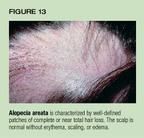
Alopecia areata is an autoimmune condition characterized by well-definedpatches of complete or near total hair loss (Figure 13). The scalp is normalwithout erythema, scaling, or edema.
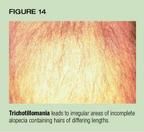
Trichotillomania produces irregular areas of incomplete alopecia, withinwhich are hairs of differing lengths (Figure 14). Occasionally, erosionsor petechiae are present on the scalp.
Hair pulling caused by physical abuse can generally be distinguishedfrom these and other hair disorders by the presence of scalp petechiae orpurpura, bogginess of the scalp caused by subgaleal hemorrhage, and evidenceof trauma at other sites.1,29
Conditions mistaken for sexual abuse
Concern about possible sexual abuse may arise from perineal or perianalerythema, erosions, swelling, or bleeding that suggest trauma, or by papulesor ulcers that may indicate a sexually transmitted disease.
Perianal streptococcal disease. Perianal infection with group A b-hemolyticstreptococci causes local itching, pain, erythema, and, occasionally, blood-streakedstool (Figure 15).30 These manifestations may be confused withtrauma resulting from sexual abuse. A bacterial culture or antigen-detectiontestwill confirm the diagnosis.

Lichen sclerosus et atrophicus (LS&A) is an uncommon disorder inchildren but one that has been commonly misdiagnosed as trauma resultingfrom sexual abuse.31 It typically occurs in girls and usuallyinvolves the genitalia.
Early lesions are white papules or plaques that become atrophic areas.Because the affected skin is fragile and susceptible to minor trauma, patientsoften have bruising, bullae (that may be hemorrhagic), or erosions withinor bleeding from affected areas. In girls, lesions are distributed aroundthe vulva and perianal region in a "figure-eight" or "hourglass"pattern (Figure 16). Symptoms of LS&Ainclude genital pruritus or discomfort,dysuria, painful defecation, hematochezia, or encopresis.

The typical morphology and distribution of lesions helps differentiateLS&A from the trauma associated with sexual abuse. Diagnosis may requirecutaneous biopsy, however.
Bullous pemphigoid (BP) is an acquired immunobullous disease that usuallyaffects the elderly.32 Affected individuals develop tense, sometimeshemorrhagic bullae and erosions (Figure 17). A rare variant of BP, localizedvulvar pemphigoid, occurs in children, creating lesions that may simulatethe trauma of sexual abuse or an ulcerative sexually transmitted disease.A definitive diagnosis requires cutaneous biopsy and direct immunofluorescencetesting.

Levine and colleagues reported the case of a 3-year-old girl who developedpruritic ulcers on her labia and vestibule. Evaluation by a pediatricianand a gynecologist suggested that the lesions were the result of sexualabuse. Although the girl was allowed to remain in her mother's custody,the child welfare agency stipulated that the father move out of the homeand have no contact with the child. Eleven monthslater the girl was examinedby a dermatologist who performed a skinbiopsy and diagnosed localized vulvarpemphigoid.28
Crohn's disease. A 10-year-old girl was brought to our institution withrectal bleeding, a perineal rash, and weight loss. The child's mother reportedthat the girl had spent the summer with relatives in another city and, uponreturning home, had these symptoms. Examination revealed marked edema andfissuring of the vulva (Figure 18) and multiple perianal fissures and erythematouspapules.

Initially, concern was raised that the edema resulted from sexual assaultand that the papules represented condyloma acuminata. A barium enema, however,demonstrated irregularity and ulceration of the rectal mucosa and narrowingof the rectum. A biopsy of one of the cutaneous papules showed a granulomatousdermatitis consistent with Crohn's disease.
Although diarrhea and abdominal pain are the usual symptoms of Crohn'sdisease, perianal and vulvar involvement may occur and, at times, precedeintestinal manifestations. Children with vulvar Crohn's disease exhibitabscesses, induration, or edema that may be mistaken for signs of trauma.Vulvar or perianal papules can mimic lesions of condyloma acuminata, whileulcers may be misinterpreted as evidence of an ulcerative sexually transmitteddisease. In the perianal region, fissures and skin tags may be mistakenfor evidence of anal penetration. An awareness of this presentation alongwith a careful history, growth evaluation, and physical examination maysuggest the diagnosis. Biopsy is often required for confirmation.
Lymphangioma circumscriptum. Darmstadt reported the case of a 5-year-oldboy who was the victim of anal intercourse. Coincidentally, he had an erythematousplaque on the buttock at the margin of which were clusters of "gelatinous-appearing,verrucous, coalescent papules."18 The appearance of thelesions and the history of sexual abuse led clinicians to diagnose condylomaacuminata and initiate cryotherapy, which proved of no benefit. A dermatologyconsultation and biopsy revealed lymphangioma circumscriptum.
As discussed previously, lymphangiomas are benign malformations of lymphchannels that may be manifest clinically as cystic or vesicular lesions.Lymphangioma circumscriptum is a form of this disorder characterized byvesicles that may be hemorrhagic (Figure 19). Typically, lesions are presentat birth or appear in early childhood. Vesicles may increase in number overtime, however. The condition persists and the only effective therapy isexcision.

A vital distinction
Abnormalities of the skin are the most common physical manifestationsof child abuse. Pediatricians must be aware, however, that certain dermatologicdisorders may produce lesions that can be mistaken for signs of inflictedinjury. An awareness of these conditions will help avoid false allegationsof abuse and their potentially devastating consequences.
REFERENCES
1. Ellerstein NS: Dermatologic manifestations of child abuse and neglect,in Ellerstein NS (ed): Child Abuse and Neglect. New York, Churchill Livingstone,1981, p 221
2. Sinal SH: Sexual abuse of children and adolescents. South Med J 1994;87:1242
3. Bays J: Conditions mistaken for child abuse, in Reece RM (ed): ChildAbuse: Medical Diagnosis and Management. Philadelphia, Lea & Febiger,1994, p 358
4. Bays J, Jenny C: Genital and anal conditions confused with child sexualabuse trauma. Am J Dis Child 1990;144:1319
5. Kaplan JM: Pseudoabuse--The misdiagnosis of child abuse. J ForensSci 1986;31:1420
6. Chadwick DL: The diagnosis of inflicted injury in infants and youngchildren. Pediatr Ann 1992;21:477
7. Saulsbury FT, Hayden GF: Skin conditions simulating child abuse. PediatrEmerg Care 1985;1:147
8. Coffman K, Boyce T, Hansen RC: Phytophotodermatitis simulating childabuse. Am J Dis Child 1985;139:239
9. Goskowicz MO, Friedlander SF, Eichenfield LF: Endemic "lime"disease: Phytophotodermatitis in San Diego County. Pediatrics 1994;93:828
10. Brown J, Melinkovich P: Schönlein-Henoch purpura misdiagnosedas suspected child abuse: A case report and literature review. JAMA 1986;256:617
11. Scaramuzza A, Pezzarossa E, Zambelloni C, et al: Case of the month:A girl with edema and purpuric eruption. Eur J Pediatr 1997;156:813
12. Waskerwitz S, Christoffel KK, Hauger S: Hypersensitivity vasculitispresenting as suspected child abuse: Case report and literature review.Pediatrics 1981;67:283
13. Anh NT: "Pseudo-battered child" syndrome. JAMA 1976;232:2288
14. Leung AKC: Ecchymoses from spoon scratching simulating child abuse.Clin Pediatr 1986;25:98
15. Asnes RS, Sisotsky DH: Cupping lesions simulating child abuse. JPediatr 1981;99:267
16. Adler R, Kane-Nussen B: Erythema multiforme: Confusion with childbattering syndrome. Pediatrics 1983;72:718
17. Wheeler DW, Hobbes C: Mistakes in diagnosing nonaccidental injury:10 years' experience. Br Med J 1988;296:233
18. Darmstadt GL: Perianal lymphangioma circumscriptum mistaken for genitalwarts. Pediatrics 1996;98:461
19. Williams CM, Spector R, Braun M: Cervical bruises--A battered child?Arch Dermatol 1986;122:1066
20. Tunnessen WW: The girl with the blue hands. Contemporary Pediatrics1985;2(1):55
21. Scales JW, Fleischer AB Jr, Krowchuk DP: Bullous impetigo. Arch PediatrAdolesc Med 1997;151:1168
22. Abuse charges dropped. Winston-Salem Journal, July 11, 1998, p B8
23. Dannaker CJ, Glover RA, Goltz RW: Phytophotodermatitis. Clin Pediatr1988;27:289
24.Sandler AP, Haynes V: Nonaccidental trauma and medical folk belief:A case of cupping. Pediatrics 1978;61:921
25. Reinhart MA, Ruhs H: Moxibustion: Another traumatic folk remedy.Clin Pediatr 1985;24:58
26. Rosenberg L, Sagi A, Stahl N, et al: Maqua (therapeutic burn) asan indicator of underlying disease. Plast Reconstr Surg 1988;82:277
27. Winship IM, Winship WS: Epidermolysis bullosa misdiagnosed as childabuse. A report of 3 cases. S Afr Med J 1988;73:369
28. Levine V, Sanchez M, Nestor M: Localized vulvar pemphigoid in a childmisdiagnosed as sexual abuse. Arch Dermatol 1992;128:804
29. Hamlin H: Subgaleal hematoma caused by hair-pull. JAMA 1968;204:339
30. Kokx NP, Comstock JA, Facklam RR: Streptococcal perianal diseasein children. Pediatrics 1987;80:659
31. Jenny C, Kirby P, Fuquay D: Genital lichen sclerosis mistaken forchild sexual abuse. Pediatrics 1981;83:597
32. Nemeth AJ, Klein AD, Schachner LA: Childhood bullous pemphigoid:Clinical and immunologic features, treatment and prognosis. Arch Dermatol1991;127:378
By Jeffrey W. Scales, MD, Alan B. Fleischer, Jr., MD, SaraH. Sinal, MD, and Daniel P. Krowchuk, MD.
DR. SCALES, a former Resident in the Department of Dermatology at Wake Forest University Baptist MedicalCenter, Winston-Salem, NC, is in the private practice of dermatology inDurham, NC.
DR. FLEISCHER is Associate Professor of Dermatology at WakeForest University School of Medicine, Winston-Salem.
DR. SINAL is Associate Professor of Pediatrics at Wake Forest University Schoolof Medicine.
DR. KROWCHUK is Associate Professor of Pediatrics and Dermatologyat Wake Forest University School of Medicine.
Cover story. Contemporary Pediatrics 1999;0:136.
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.