Spitz Nevus and Pyogenic Granuloma
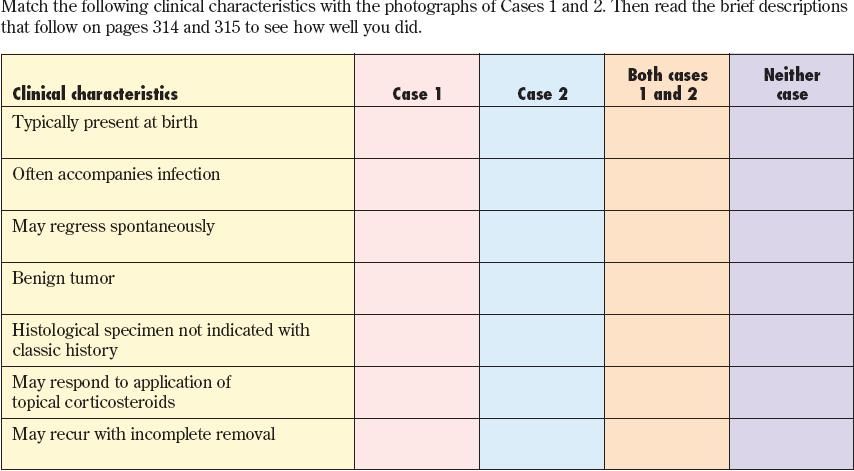
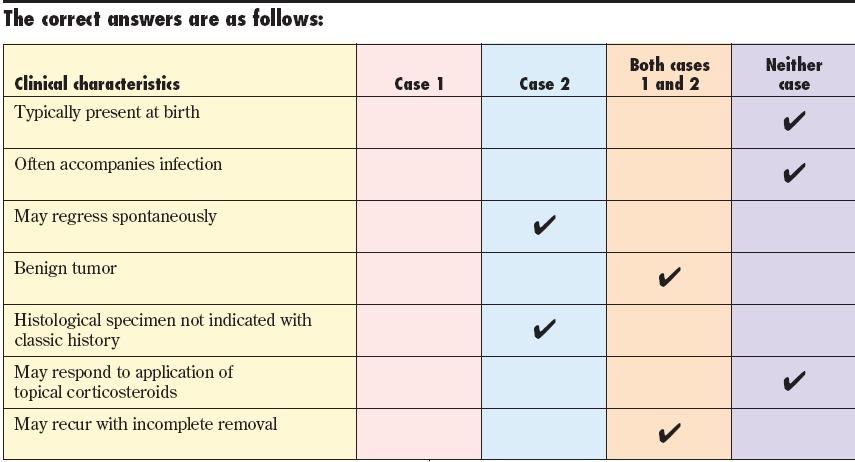
Match the following clinical characteristics with the photographs of Cases 1 and 2. Then read the brief descriptions that follow on pages 314 and 315 to see how well you did.
Figure
Figure
Figure
Figure

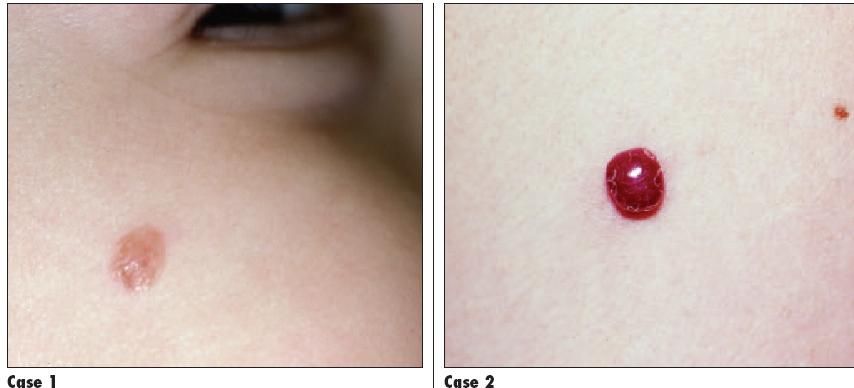
Figure>Case 1 and Case 2
Match the following clinical characteristics with the photographs of Cases 1 and 2. Then read the brief descriptions that follow on pages 314 and 315 to see how well you did.
DISCUSSION
Both of the disorders presented here are characterized clinically by relatively rapidly growing facial papules. In fact, there are remarkable similarities in many aspects of the 2 case presentations. However, Case 1 represents a Spitz nevus, while Case 2 is a classic pyogenic granuloma.
Case 1 shows a fair-complected 5-year-old girl who presented for evaluation of a pinkish brown papule on her right cheek. The lesion (5 mm in diameter) had grown rapidly over the previous 2 months: it was neither ulcerated nor pruritic. An excisional biopsy was performed, which demonstrated nests of spindle-shaped melanocytes, Kamino bodies (eosinophilic and periodic acid-Schiff-positive globules), and an absence of mitoses. A diagnosis of Spitz nevus was made, and there was no recurrence during 2 years of follow-up.
Spitz nevi-also referred to as benign juvenile melanoma-are benign lesions estimated to represent approximately 1% of all melanocytic nevi in children.1 They can resemble melanoma both clinically and histologically, with no clear diagnosis possible in approximately 8% of cases.2 On physical examination, the nevi are usually solitary red to brown nodules with smooth or warty surfaces, ranging in size from 0.3 to 1.5 cm. Histologically, the nevi are characterized by a single-file infiltration of collagen, well-demarcated lateral borders and confinement of pagetoid spread to the center of the lesion. Histochemical staining for specific markers including S100A6, HMB-45, Ki-67, and p21 may help confirm the diagnosis.3 Surgical biopsy with clear margins is the generally recommended treatment, especially for atypical Spitz nevi.
Most Spitz nevi occur in patients younger than 20 years old, with no clear gender predilection. They most commonly arise on the face (where they tend to be less heavily pigmented) or legs (where they tend to be more heavily pigmented), either de novo or within a preexisting melanocytic nevus.4 Their growth in the initial phase may be quite rapid. There have been reports of recurrence and rare cases with nodal micrometastases,5but simple excision is usually curative. While melanoma is uncommon in younger patients, it is nonetheless prudent to be concerned about any rapidly growing, pigmented neoplasm.6
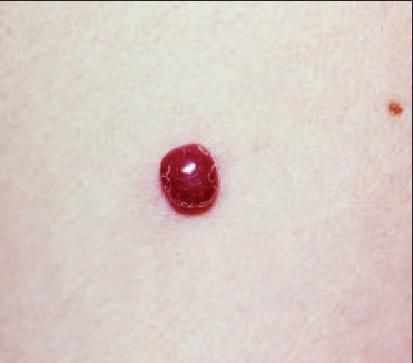
Case 2, much like the previous one, is that of a 7-year-old boy in whom a similarly sized, painless facial lesion developed that was characterized by very rapid growth. One difference historically was that this redder papule had bled profusely on several occasions following minor trauma.
This lesion is a classic pyogenic granuloma. This term is a complete misnomer, because the condition is neither infectious nor granulomatous. It is a common benign vascular neoplasm of the skin and mucosa that reaches its maximum size in a few weeks. Pyogenic granulomas are most often found on the head, neck, upper extremities, and trunk. There is no racial predilection, and males are affected slightly more often than females.7,8 Histology is that of a lobular capillary hemangioma. Because of its vascular nature, the pyogenic granuloma is prone to bleeding.
The underlying cause of pyogenic granuloma remains obscure. While trauma has long been considered a primary cause, a large study found that most patients did not have antecedent trauma.7
The diagnosis can often be made by history and physical examination, and biopsy should only be considered when the presentation is atypical. Untreated lesions most often regress, generally within 6 months of onset.
9
Treatment can be offered for cosmetic reasons or because of repeated bleeding. The most effective treatment is full-thickness excision, but this is often not done because of the young age of the patient or the cosmetically sensitive area in which pyogenic granuloma tends to arise. Alternative therapeutic maneuvers include light liquid nitrogen cryotherapy or curettage followed by electrocautery.8 Recurrence may follow incomplete removal.
References:
- Rapini RP. Spitz nevus or melanoma? Semin Cutan Med Surg. 1999;18:56-63.
- Branhill RL. The Spitzoid lesion: rethinking Spitz tumors, atypical variants, "Spitzoid melanoma" and risk assessment. Mod Pathol. 2006;19:S21-S33.
- Kapur P, Selim MA, Roy LC, et al. Spitz nevi and atypical Spitz nevi/tumors: a histologic and immunohistochemical analysis. Mod Pathol. 2005;18:197-204.
- Dal Pozzo V, Benelli C, Restano L, et al. Clinical review of 247 case records of Spitz nevus (epithelioid cell and/or spindle cell nevus). Dermatology. 1997; 194:20-25.
- Urso C, Borgognoni L, Saieva C, et al. Sentinel lymph node biopsy in patients with "atypical Spitz tumors." A report on 12 cases. Hum Pathol. 2006;37:816-823.
- Schaffer JV. Pigmented lesions in children: when to worry. Curr Opin Pediatr. 2007;19:430-440.
- Patrice SJ, Wiss K, Mulliken JB. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr Dermatol. 1991;8:267-276.
- Pagliai KA, Cohen BA. Pyogenic granuloma in children. Pediatr Dermatol. 2004;21:10-13.
- Requena L, Sangueza OP. Cutaneous vascular proliferation, part II: hyperplasias and benign neoplasms. J Am Acad Dermatol. 1997;37:887-919.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.