Surviving the challenges of healthcare reform
Pediatric practice requires that parent and physician navigate what has become a complex matrix of rules and regulations set in our path by insurance companies and the government. Thanks to the Affordable Care Act (ACA), these obstacles have never been more complicated.
Pediatric practice requires that parent and physician navigate what has become a complex matrix of rules and regulations set in our path by insurance companies and the government. Thanks to the Affordable Care Act (ACA), these obstacles have never been more complicated. In this installment of Peds v2.0, we’ll take a look back at the effect that insurance companies and government “interventions” have had on medical practice and suggest ways to minimize their impact on your practice.
Insurance and the doctor/patient relationship
In 1988, I started a small private practice in Manchester, New Hampshire. As that time, we collected payment in full upon visit completion, and if patients had insurance they would submit their receipts for reimbursement. We were sensitive to the financial circumstances of our patients. If parents had a financial hardship we would provide free or reduced-cost services. We supported our patients in this fashion until the parents’ circumstances improved.
When healthcare costs began to rise in the 1990s, most patients transitioned to either employer-provided or privately acquired health insurance, and we billed insurance companies directly for services rendered. We did our best when negotiating our contracts with insurance companies and graciously accepted discounted payments in order to build or maintain our patient base. At the time, we could not afford to accept Medicaid because the payments were inadequate to pay our costs of providing care for these patients.
Over time, insurance companies developed a variety of methods to lower their costs, which had the unfortunate effect of increasing the workload of providers and staff. Most insurance companies required that requests for imaging studies be reviewed by a radiologist employed by the company prior to approval. Additionally, we could only prescribe medications in an insurance company’s formulary, and patients could only receive care provided by hospitals, laboratories, surgery centers, and specialists in the insurance company’s service network. For patients enrolled in health maintenance organizations, physicians were placed in the uncomfortable position of acting as a “gatekeeper"-limiting our patients’ access to specialists and providing approval for patients’ access to emergency department services. Thus began the interesting triad of the doctor, patient, and insurance company that continues to this day.
Although most pediatricians disapproved of the bureaucracy associated with caring for insured patients, over time we learned the nuances that could help us avoid insurance-related obstacles. We learned what language we needed to put in a request for an imaging study to increase the likelihood of approval by the insurance company-employed radiologist. We also learned how to circumvent a pharmacist’s request for a prior approval of a prescribed medication, just by asking which alternatives could be substituted (so our staff did not need to stay on hold with insurance companies for hours or days at a time).
If we needed to deal with only the nuances and vagaries of the insurance system, the daily routine in a medical practice would be tolerable if not joyous. However, things got more complicated still when the government began to intervene.
CLIA ’88 and OSHA and HIPAA regs, oh my!
If you were in private pediatric practice in the 1980s, you will recall that we screened for anemia by spinning finger-stick blood placed in a hematocrit tube, and performed throat cultures and urine cultures using a small office incubator. Our rudimentary technology served both our patients and us well. Eventually our office technology began to evolve with the introduction of what was viewed as “sophisticated” tests (ie, chemistry analyzers, complete blood count machines, lipids assays, and rapid antigen tests) and legislators saw the need to protect the “patient consumer” from inaccurate testing in the medical office. As a consequence, the now-famous Clinical Laboratory Improvement Amendments-aka CLIA ’88-were implemented in the fall of 1992.
In retrospect, CLIA ’88 had the effect of minimizing the number of tests that could be performed in a small medical office, and eventually most practices decided to perform only tests that were designated as “CLIA waived.” Thus physicians could no longer perform office throat and urine cultures and needed to outsource many tests to hospital or commercial labs. This had the effect of making the practice of medicine less efficient, and most practices lost considerable lab revenue as a consequence. It also had a disruptive effect on medical innovation because manufacturers had to strive to make CLIA-waived products in order to turn a profit.
At the same time that CLIA ’88 went into effect, the Occupational Safety and Health Administration (OSHA) implemented a wide-ranging plan developed to reduce hazards in the medical workplace. It mandated the implementation of numerous procedures that would reduce the transmission of diseases via education and training of personnel. It was well intended, but compliance required significant effort on the part of office staff. The repercussion of noncompliance was hefty fines, and rumors of practice closures because of noncompliance were widespread. Years later, the regulation was revised to make handling of sharps less likely to cause injury in the medical workplace.
In 1996, the Health Insurance Portability and Accountability Act (HIPAA) went into effect, mandating that practices implement systems and actions to ensure the protection and privacy of our patients’ medical information. Our practice workload increased further as a result.
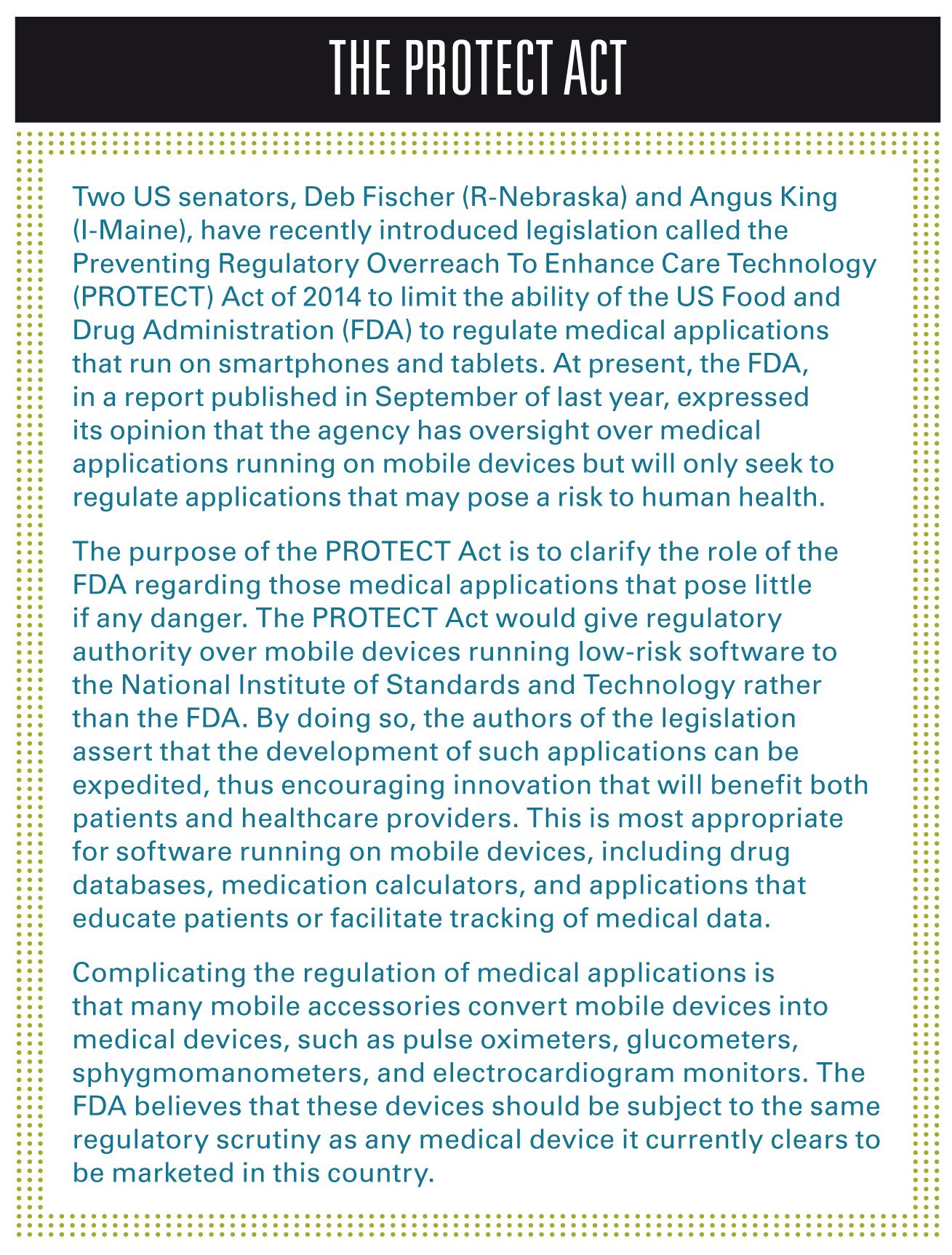
CLIA ’88, OSHA, and HIPAA regulations were our introduction to government regulation and onerous government paperwork. In hindsight, OSHA was and continues to be a good program, and little needs to be done to comply with regulations. In my view, HIPAA is too extreme in its requirements and continues to be burdensome for many practices. CLIA ’88 had the long-term effect of stifling medical innovation. The regulation of medical devices continues to this day.
The HITECH Act and the ACA
The recent changes in healthcare reform began innocently enough with the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009. Passed in conjunction with the American Recovery and Reinvestment Act of 2009, HITECH was developed to incentivize physicians to adopt approved electronic health records (EHRs) through modest payments over a period of years. Those participating in either Medicaid or Medicare (not both) would be eligible. As a consequence, eligible practices began to upgrade to EHR technology, only to discover that the incentive money could not offset the cost of implementation and the loss of productivity associated with adopting EHRs. Additionally, many were surprised by the complex requirements that had to be satisfied (ie, meaningful use 1, 2, and 3) in order for practices to continue to receive incentive payments through the final years of the program.
The ACA has been the subject of much controversy and discussion. It would be fair to say that as of this writing, the ACA has caused many families to lose insurance coverage and replace reasonable health plans with those having high deductibles and co-pays. It is commendable that the ACA mandates that preventive healthcare services be covered by insurance companies (unfortunately adding to the cost of all plans), and that Medicaid rates have been temporarily increased to the level that can support pediatrician participation.
The ACA also has given rise to new economic models for reimbursement based on quality of care and outcomes. Joining an Accountable Care Organization (ACO) will require generating data proving that you achieve certain benchmarks. Fail to comply and your revenue will fall. Such bureaucratic silliness is contributing to the growing angst among healthcare providers concerned about the potential impact the ACA will have on their practices and patient care. Not necessarily reassured by ACA proponents that “we’re from the government and we’re here to help you,” physicians are not so easily persuaded to welcome government involvement in the all-important doctor-patient relationship.
What to do?
In the profound words of Douglas Adams (TheHitchhiker’s Guide to the Galaxy), first “Don’t panic,” and continue to concentrate on providing the best “outcome” for each patient, one patient at a time, just as you have always done. Review some of the previous Peds v2.0 articles to improve your billing and office workflow; use your EHR efficiently; adopt useful technologies; and continue to be guided by the Golden Rule of Pediatric Practice (ie, treat your patient as you would like to be treated yourself).
Continue to circumvent insurance company obstacles. As nonproviders of Medicare, pediatricians won’t be penalized financially at this point if they choose not to adopt an EHR. One can choose not to participate in the meager financial incentives offered by the ACA, for which you won’t qualify unless you have at least 20% of your practice as Medicaid. In the months to come, we all will learn the fate of the ACA and if it will be repealed or revised following our November elections.
It might be time for traditionally timid pediatricians to become more active advocates for ourselves, our profession, and the patients in our care. The American Academy of Pediatrics (AAP) has historically advocated for improving the healthcare of our patients, and many members believe it needs to more aggressively advocate for the plight of pediatricians. One might consider joining the Association of American Physicians and Surgeons, which is a small organization of physicians (3000-plus strong) whose goal is to preserve the sanctity of the patient-physician relationship by removing regulatory obstacles.
It is not surprising what physicians can do when we band together. By working with our state chapter of the AAP, pediatricians in New Hampshire are now receiving payment from insurance companies (including Medicaid) for vision screening using photoscreening technology. We have also worked with our state Insurance commissioner to remedy problems with our new managed Medicaid plans.
Perhaps we will be guided by the wisdom of Jerry Garcia of the Grateful Dead who said, “Somebody has to do something, and it's just incredibly pathetic that it has to be us.”
Dr Schuman is adjunct associate professor of pediatrics, Geisel School of Medicine at Dartmouth, Lebanon, New Hampshire. He is also section editor for Peds v2.0 and editorial advisory board member for Contemporary Pediatrics. He has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.