A Toddler Intolerant of Tube Feeding
A 22-month-old boy with failure to thrive presented with a 3-day history of rhinorrhea, fever, and abdominal pain associated with tube feeding. A PEG tube had been placed 2 months before this visit.
A 22-month-old boy with failure to thrive presented with a 3-day history of rhinorrhea, fever, and abdominal pain associated with tube feeding. A percutaneous endoscopic gastrostomy (PEG) tube had been placed 2 months before this visit. Physical examination found tenderness on palpation around the PEG tube and a yellow discharge from the site. Culture of the discharge grew methicillin-sensitive Staphylococcus aureus. A blood culture was negative and fluoroscopy with contrast of the PEG tube was normal. The child was treated with antibiotic agents for a localized infection of the PEG tube site. After 7 days, however, symptoms failed to resolve.
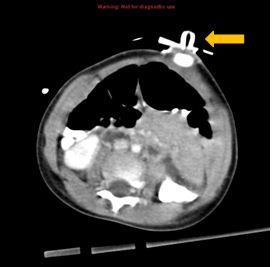

Figure 1.
Abdominal CT shows internal bumper of the PEG tube within the abdominal wall (arrows).
Follow-up examination found a palpable, erythematous mass at the PEG tube site, presumed to be an abscess. A subsequent ultrasound study, however, was negative for abscess or fluid collection. Fluoroscopy with contrast found normal flow into the stomach. A CT scan of the abdomen showed that the internal bumper of the PEG tube had migrated and lodged between the abdominal wall and the skin (Figures 1 and 2), a phenomenon called buried bumper syndrome. The bumper was the palpable mass noted above. The PEG tube was removed by external traction and replaced with a Tri-Funnel tube without complications and the local infection resolved.
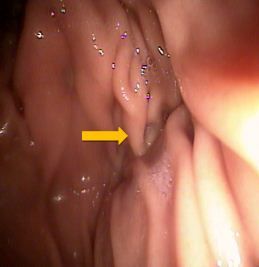
Figure 2.
Endoscopic view of previous PEG tube site in the gastric mucosa (arrow).
Discussion
Buried bumper syndrome is an uncommon but serious complication of a PEG tube. It occurs in 1.6% of children with the device and is generally a late complication, occurring months or even years after the initial tube placement.1 The internal bumper of the tube erodes through the gastric wall and becomes lodged between the wall and the skin along the original tube tract.2 The most likely cause is excessive tension between the internal and external bumpers. The most common presenting symptoms of buried bumper syndrome-abdominal pain, inability to infuse feedings, and leakage around the tube-are associated with clogging and immobilization of the tube.
A buried bumper should always be removed, even if the patient is asymptomatic, to avoid serious complications such as gastrointestinal bleeding, gastric perforation, and peritonitis.3 As this case illustrates, infusion of feeds may be unobstructed despite BBS. Also of note in this case, findings from ultrasound and fluoroscopic dye studies were negative. Abdominal CT may be required to identify the relocated bumper.
Teaching Points
• Clinicians should have a high index of suspicion for BBS in a child with a PEG tube who presents with feeding intolerance.
• High suspicion for BBS should remain if feeding intolerance persists despite normal findings on ultrasound and fluoroscopy with contrast.
• BBS typically is a late complication, and should be considered even several years after PEG tube placement.
References:
ReferencesÂ
1. Khalil Q, Kibria R, Akram S. Acute buried bumper syndrome. South Med J. 2010;103:1256-1258.
2. Schrag SP, Sharma R, Jaik NP, et al. Complications related to percutaneous endoscopic gastrostomy (PEG) tubes. A comprehensive clinical review. J Gastrointestin Liver Dis. 2007;16:407-418.
3. Schapiro GD, Edmundowicz SA. Complications of percutaneous endoscopic gastrostomy. Gastrointest Endosc Clin N Am. 1996;6:409-422.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.