The toxic toddler: Drugs that can kill in small doses
Toddlers are prime candidates for accidental poisonings, and certain medications found in many households dramatically increase the risk of death from swallowing even one or two pills. Recognizing the dangers of these drugs and taking a careful history can save a childs life
The toxic toddler:
Drugs that can kill in small doses
By Kevin C. Osterhoudt, MD
Toddlers are prime candidates for accidental poisonings, and certain medications found in many households dramatically increase the risk of death from swallowing even one or two pills. Recognizing the dangers of these drugs and taking a careful history can save a child's life.
Most children between 1 and 2 years of age have developed the dexterity to use a pincer grasp and have often just learned to walk. These developmental milestones allow a degree of mobility and exploration of the home for which parents commonly find themselves unprepared. Young children often explore their environment by putting objects in their mouths. They also like to mimic actions they have seen their parents perform. It is not surprising that accidental poisoning is a common medical emergency in this age group.
More than 2 million toxic exposures are reported to The American Association of Poison Control Centers each year, over half of them involving children under 6 years of age.1 Fortunately, this group accounts for fewer than 5% of all poisoning-related deaths.
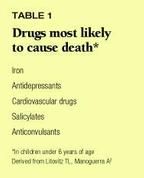
Pharmaceutical agents comprise 42% of all toxic exposures reported to poison centers.1 Table 1 lists the types of drugs that most often cause unintentional ingestion deaths in children.2 Review of these data and published case reports shows clearly that certain medications are inherently more dangerous to young children than others.
Health-care providers are often confronted with a toddler thought to have ingested just one or two doses of a medication. This can be a particularly vexing problem. Experience tells us that most of these children will be fine with little treatment beyond reassurance. A few drugs, however, can be life-threatening in small amounts, and in such cases, proper evaluation and intervention can save a child's life. Physicians need to be familiar with a modest list of drugs capable of killing a small child in one or two doses (Table 2) and adopt a systematic approach to evaluating children who have ingested them.

17 drugs highly toxic to toddlers
Considering the relatively high percentage of toxic exposures that involve drugs, it is fortunate that only a few medications are truly life-threatening to a young child who ingests only one or two pills or one to two teaspoon-sized swallows. None of the medications listed in Table 2 will injure every exposed child. Yet they have given physicians ample reason to be wary even though adequate epidemiologic estimates of their risks have not been performed to date. It is worth noting that antidepressants, cardiovascular medications, and salicylates comprise three of the five drug groups most lethal to children and also account for a large proportion of the medications that are dangerous in small amounts. Any list of toxic drugs will prove ultimately to be incomplete. Accidental childhood poisonings must be evaluated on a case-by-case basis.
Antidepressants and antipsychotics
Among antidepressant and antipsychotic drugs, cyclic antidepressants and phenothiazines are especially hazardous to young children. Several other classes of antipsychotics, including dibenzodiazepines such as clozapine, also may be dangerous to children in small doses.
Cyclic antidepressants are notorious for their cardiotoxic effects after intentional overdose and can cause serious problems in young children who accidentally ingest even small amounts. Characteristic toxic effects include widening of the QRS interval and ventricular arrhythmia, hypotension from ß-adrenergic blockade, central nervous system depression and convulsion, and anticholinergic activity.
The tricyclic agents imipramine and desipramine are commonly implicated in pediatric poisonings. Interestingly, imipramine retains some popularity in treating childhood enuresis. The drug, which is available in the US in a dose of 150 mg, has a minimum estimated fatal dose of 15 mg/kg.3 Ingestion of just one 150-mg pill by a toddler weighing 10 kg can be deadly.
Amoxapine is distinctive among cyclic antidepressants. It has less cardiotoxicity than other drugs in this class, and seizures and coma are frequent presenting signs of toxicity.
Phenothiazines. Chlorpromazine and thioridazine appear to be the most potent threats to young children from this class of drugs. These agents, in addition to their typical anticholinergic and CNS effects, seem to share the quinidine-like cardiotoxicity seen with cyclic antidepressants. Chlorpromazine, available in 200-mg doses, killed a child who ingested 20 mg/kg, and thioridazine has an estimated minimum potential fatal dose of 15 mg/kg.3,4 The dystonic reactions seen with these drugs, although uncomfortable, are rarely life-threatening.
Cardiovascular drugs
Cardiovascular drugs that can harm young children in small amounts include ß-blockers, calcium antagonists, clonidine, and quinidine.
ß-blockers. The bradycardia and hypotension associated with ß-adrenergic antagonism are generally well tolerated by children. An underappreciated toxicity of ß-blockers that affects children primarily is hypoglycemia. Hypoglycemic seizures and coma have been observed both after accidental ingestion and with therapeutic use.5 ß-adrenergic blockade may blunt objective signs of hypoglycemia, and younger children, who are especially susceptible to hypoglycemia, often cannot describe hypoglycemic symptoms.
Lipophilic ß-adrenergic blocking drugs, such as propranolol, possess membrane-depressant activities that can lead to seizures and altered cardiac conductivity. Sotalol, a ß-blocker with type III antiarrhythmic activity, causes dose-dependent prolongation of the QT interval, and young children may be susceptible to torsades de pointes after an accidental overdose.
Published case reports contain insufficient information to allow reliable calculation of a minimum potentially fatal dose for ß-blockers. Typically prescribed dosages for propranolol are in the range of 1 to 4 mg/kg/day, and the package insert warns against exceeding 16 mg/kg/day. Propranolol is available in 160-mg tablets.
Calcium antagonists. Bradycardia and hypotension are the most common manifestations of poisoning with calcium-channel blocking agents. Cardiovascular collapse and seizures occurred after ingestion of less than 40 mg/kg of verapamil by an infant.6
The widespread prescription of calcium antagonists to parents and grandparents puts children at inevitable risk of accidental exposures. Deaths of both adults and children from calcium-channel blocker overdose are reported yearly, and deaths of children have occurred from low-dose exposures. Some researchers are attempting to define a low-risk poisoning exposure from these drugs. Current evidence suggests that all exposures in young children should be regarded cautiously.7
Clonidine is used to treat hypertension, narcotic withdrawal, and childhood hyperactivity and anxiety disorders. This centrally acting ß-adrenergic agent decreases sympathetic outflow from the midbrain. Clonidine is a potent drug that is often prescribed to adults in doses of 100 to 300 mg. Ingestions of small amounts can lead to coma, miosis, bradycardia, hypotension, and hypothermia in children.8 Poisoning by exposure to clonidine transdermal patches has also been noted to cause critical cardiovascular depression.9
Clonidine is an imidazoline compound similar to over-the-counter topical preparations like tetrahydrozoline. Small ingestions of imidazoline eye drops have caused severe toxicity, including a report of sinoatrial node arrest.10
Quinidine. Considering the serious "quinidine-like" cardiotoxicity of cyclic antidepressants, selected phenothiazines, and selected ß-adrenergic antagonists, it should come as no surprise that this type 1a antiarrhythmic agent can be dangerous to toddlers. Approximately 50 mg/kg of quinidine has produced severe cardiac rhythm disturbances in young children.11
Opioids
Diphenoxylate and methadone present the greatest hazard to toddlers from low-dose ingestions.
Diphenoxylate. Lomotil is an antidiarrheal preparation containing diphenoxylate and atropine. This combination of opioid and anticholinergic medications may cause a confusing constellation of symptoms, but the coma and respiratory depression typical of opiate overdose are most common. Even one tablet (or teaspoon) can be expected to cause symptoms in toddlers, and as few as two tablets have proved fatal.12 Extended observation of any child who has ingested Lomotil is a wise precaution since the opioid's effects may be delayed and prolonged.
Methadone is a long-acting opioid used to treat opiate addiction. Fatal respiratory arrest has been reported in children after ingestion of 50 mg.13 The 10 mg/mL methadone suspension can be particularly dangerous to young children in the home of a drug-addicted caretaker because it is highly concentrated and easy to ingest.
Topical agents
Four drugs present in various topical preparationsbenzocaine, camphor, lindane, and methyl salicylatecan cause serious problems if ingested by toddlers.
Benzocaine. Many physicians are surprised to learn that benzocaine, a common ingredient in popular over-the-counter teething gels and other local anesthetic preparations, can cause severe methemoglobinemia in children. The most common scenario is overzealous mucosal applications of benzocaine gel by a well-meaning parent, but accidental ingestion also occurs.
Methemoglobin is an abnormal hemoglobin variant that causes cyanosis and decreased oxygen delivery to tissues. Children may vary in susceptibility to methemoglobinemia because of individual differences in innate methemoglobin reduction systems.
As little as 100 mg of benzocaine, an amount available in less than 2 cc of most teething gels, can produce symptomatic methemoglobinemia in an infant. Methemoglobin levels as high as 59% have been noted after application of teething gel.14 Seizures are another common toxic effect of local anesthetic agents, but they occur infrequently after accidental benzocaine exposure.
Camphor is another common ingredient in over-the-counter products, such as inhalants used for chest colds and topical anesthetics, whose potent toxicity comes as a surprise to many. Its range of neurotoxic effects includes CNS depression, respiratory depression, and seizures.
Highly concentrated camphorated oils are tightly regulated in the US, but popular camphor-containing products such as Campho-Phenique (10.8% camphor) and Vicks Vaporub (4.7% camphor) remain on the market. Accidental ingestion of 1 g of camphor, available in less than two teaspoons of Campho-Phenique, has resulted in the death of a toddler.15
Lindane. Seizures and CNS depression may follow ingestion of this popular topical organochlorine scabicide. Ingestions occur by accident or when caregivers misunderstand the instructions for its administration. Lindane poisonings are rarely fatal, but an estimated dose of 6 mg/kg has been implicated in the death of a young child.16 Agents containing permethrin are less toxic and often provide a therapeutic alternative.
Methyl salicylate. A toddler would have to ingest at least four extra-strength aspirin tablets to exceed the 200 mg/kg that is the estimated minimum potentially lethal dose of salicylate.3 It is important to recognize, however, that a highly concentrated form of salicylate, methyl salicylate, is found in many common commercial products. Liniments and food flavorings containing oil of wintergreen may be up to 98% methyl salicylate. One teaspoon of oil of wintergreen is equivalent to 7 g of salicylate, or 14 extra-strength aspirin tablets.
Methyl salicylate is also found in many topical arthritis remedies and muscle balms and in a variety of Chinese patent medicines. The candy-like aroma of these preparations makes them particularly attractive to children.
Other dangerous drugs
The remaining five drugs that can cause serious problems for toddlers in small doses are chloroquine, phenylpropanolamine, quinine, the sulfonylureas, and theophylline.
Chloroquine is widely prescribed around the world to prevent and treat malaria. Physicians practicing in the US often are not familiar with this drug and may not be aware of the hazards of an overdose. One 300-mg tablet has produced lethal cardiac dysfunction in a 1-year-old child.17 The narrow therapeutic margin of chloroquine necessitates careful anticipatory guidance with each prescription.
Phenylpropanolamine is a common ingredient in over-the-counter decongestants and has a narrow therapeutic-toxic margin. The ß-agonist action of this drug often produces a recognizable syndrome of hypertension with compensatory bradycardia. Idiosyncratic cerebral infarction has been noted in adults after ingestion of as little as one dose.18 Although severe toxicity in young children has been reported rarely, supraventricular tachycardia has been associated with therapeutic administration of less than 8 mg/kg in an infant.19
Quinine is structurally similar to quinidine and has been used to treat malaria and nocturnal muscle cramps. Quinine poisoning is notable for direct retinal toxicity. It is less cardiotoxic than quinidine. Life-threatening hypersensitivity reactions, such as "black water fever"(which leads to hemolysis and hemoglobinemia and can result in renal failure), also occur. The estimated minimum potential fatal dose is 80 mg/kg.3 Fortunately, 650-mg tablets of quinine sulfate are no longer marketed in the US.
Sulfonylurea hypoglycemic agents. Insulin is not pharmacologically active after accidental oral ingestion, but an overdose of sulfonylurea drugs, such as glyburide and chlorpropamide, can lead to hypoglycemia. Ingestion of a single tablet of glyburide has produced hypoglycemia. The hypoglycemic effects of sulfonylureas may be delayed or persistent.20 Metformin, a biguanide, is not expected to cause hypoglycemia.
Theophylline. Despite declining therapeutic use, theophylline is still widely prescribed to treat asthma, apnea of prematurity, and chronic obstructive pulmonary disease. It is available in a 500-mg dose, which could produce a serum theophylline level near 100 mg/mL in a 10-kg child. Life-threatening seizures and cardiac arrhythmias have been associated with this level of intoxication.21
Evaluation:
The importance of history
Figure 1 outlines an approach to evaluating and treating possible small-dose ingestions in toddlers that begins with a careful history of the incident. Although physicians experienced in adolescent poisonings may be dismayed at the prospect of trying to obtain an accurate history, several characteristics of poisonings in toddlers make the history a useful clinical tool. Small children typically become intoxicated accidentally with drugs or household agents that are attractive and available. This contrasts with adolescent ingestions, which result from intentional abuse or misuse, or a suicidal gesture. Toddlers are most often poisoned by one agent rather than multiple drugs. Parents or other caretakers often witness the child eating a medication and may be able to identify the offending poison, the dose size, and the time of ingestion.

Even if caretakers did not witness the ingestion directly, they may be able to detail the locations to which the child had access and create a list of potential poisons. It may be useful to have parents describe the medications and household products they have used in the last 24 hours. Children are keenly observant and often mimic their parents' actions.
A thorough history is the most useful tool in evaluating the asymptomatic, potentially poisoned young child. Any such child who may have been exposed to one or more of the medications discussed in this article should be referred to an emergency department.
Clues in the physical exam
In the symptomatic patient, specific physical signs may point to a differential diagnosis. Miotic pupils, for example, may suggest poisoning caused by narcotics or cholinergic drugs. Pay special attention to the patient's mental status and neurologic exam, vital signs, pupil size and reactivity, skin moisture and color, and bowel sounds. Abnormal signs often can be grouped into common recognizable syndromes known as toxidromes. Delineating such toxidromes is often more productive than laboratory toxicologic screening. Many toxocologic references contain full descriptions of toxidromes.22,23
Laboratory assessment
The history and physical exam are sufficient to diagnose most poisonings in young children and suggest appropriate treatment. Occasionally, ancillary studies provide useful information. Serum chemistries may detect hypoglycemia or metabolic acidosis, which can be ominous manifestations of poisoning. An electrocardiogram may reveal dysrhythmias or conduction delay, among the most dangerous sequelae of drug overdose. Other studies such as kidney function tests, tests for liver injury, carbon monoxide or methemoglobin determinations, osmolar gap calculations, and radiographs may prove useful in specific situations.
Toxicologic screens of the urine and blood are among the tests most often used to evaluate the poisoned patient. They are likely to have limited utility beyond that of the history and physical exam in managing the acutely ill patient, however.22 Physicians need to recognize that each hospital's toxicology testing capabilities are different. The most sophisticated laboratories can only screen for a small fraction of available drugs. Indeed, of the drugs listed in Table 2, only cyclic antidepressants, phenothiazines, phenylpropanolamine (amphetamine), and salicylates, can be detected by most of the commonly used qualitative screens. Most hospital laboratories can quantify theophylline levels.
Treating the toxic toddler
The first priority in treating any child who has ingested a toxic substance is to make sure the airway is stable and take steps, if necessary, to maintain adequate ventilation, and circulation. If the child is asymptomatic, obtain a precise history and direct treatment toward the offending toxin once it has been identified. The potential severity of the ingestion can be estimated by how much of what was ingested, when, and by whom (that is, the specific characteristics of the patient, such as age, weight, other medications the child may be taking, and any other medical conditions he may have).
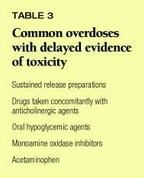
The patient who may have ingested only one or two pills (swallows) of an unknown drug presents a difficult situation. A careful history, physical exam, and laboratory investigation guided by the findings of the history and physical may narrow the differential diagnosis and facilitate an educated assessment of the potential severity of the exposure. If you cannot exclude medications that can be fatal to toddlers in one or two doses, it may be prudent to consider decontaminating the child by one of the methods discussed below and observe him for a period of time. Most severe drug overdoses produce symptoms within four to six hours after ingestion. Table 3 lists medications known to have delayed onset of symptoms beyond four to six hours.
If the child is symptomatic, give priority to the airway, breathing, and circulation and monitor vital signs frequently. Pay close attention to oxygen and blood glucose levels in a child with depressed consciousness since these substrates are vital to brain function. CNS and respiratory depression may warrant an empiric trial of 1 to 2 mg of naloxone. Higher doses may be needed to reverse the effects of certain opiate medications. Other emergent conditions that may require a medical response include seizures and abnormal thermoregulation.
Strategies to decontaminate the poisoned toddler include removing toxins from the gastrointestinal tract, preventing absorption of ingested drugs, and enhancing elimination of already absorbed toxins. Methods to remove poisons from the GI tract, such as ipecac-induced emesis or gastric lavage, are falling out of favor but may have limited application.24 Absorption of many ingested drugs can be prevented by giving activated charcoal (about 1 g/kg) or, in rare instances, whole-bowel irrigation with Golytely (250 to 500 cc/hr in toddlers). Occasionally, multiple-dose activated charcoal, urinary alkalinization, and dialysis or hemoperfusion may be indicated to enhance elimination of already absorbed poisons. Contrary to popular perception, specific antidotes are available for only a minority of poisons.
Good, fundamental supportive care is the mainstay of therapy for most intoxicated children. Regional poison control centers provide a readily accessible source of information and advice.
Big dangers in small doses
Some common medications can kill a toddler with only one to two doses. Although modest in number, they account for a large proportion of observed pediatric poisoning deaths. Physicians must recognize the serious threat these drugs pose to young children. Evaluating a toddler who has ingested as little as one or two doses of medication presents the pediatrician with a problematic clinical situation. A systematic approach centered on a careful history is of paramount importance. h
Acknowledgment: This manuscript is an expansion of ideas the author has presented in Tox Talk, an educational brochure produced by the Poison Control Center at Philadelphia.
REFERENCES
1. Litovitz TL, Klein-Schwartz W, Dyer KS, et al: 1997 annual report of the American Association of Poison Control Centers toxic exposure surveillance system. Am J Emerg Med 1998;16(5):443
2. Litovitz TL, Manoguerra A: Comparison of pediatric poisoning hazards: An analysis of 3.8 million exposure incidents. Pediatrics 1992;89(6):999
3. Koren G: Medications which can kill a toddler with one tablet or teaspoonful. Clinical Toxicology 1993;31(3):407
4. Davis JM, Bartlett E, Termini BA: Overdosage of psychotropic drugs: A review. Diseases of the Nervous System 1968;29:157
5. Reith DM, Dawason AH, Whyte IM, et al: Relative toxicity of ß-blockers in overdose. Clinical Toxicology 1996;34(3):273
6. Passal DB, Crespin FH: Verapamil poisoning in an infant. Pediatrics 1984;73(4):543
7. Osterhoudt KC, Henretig FM: How much confidence that calcium-channel blockers are safe? (letter). Vet Human Toxicol 1998;40(4):239
8. Neuvonen PJ, Vilska J, Keranen A: Severe poisoning in a child caused by a small dose of clonidine. Clinical Toxicology 1979;14(4):369
9. Caravati EM, Bennett DL: Clonidine transdermal patch poisoning. Ann Emerg Med 1988;17(2):175
10. Jones DG, Osterhoudt K, Stone M, et al: Sinoatrial node dysfunction following tetrahydrozoline ingestion (abstract). J Toxicol Clin Toxicol 1996;34(5):564
11. Dellocchio T, Pailli F, Testa O, et al: Accidental quinidine poisoning in two children. Pediatrics 1976;58(2):288
12. Emery D, Singer JI: Highly toxic ingestions for toddlers: When a pill can kill. Pediatr Emerg Med Reports 1998;3(12):111
13. Smialek JE, Monforte JR, Aronow R, et al: Methadone deaths in children. JAMA 1977;238(23):2516
14. Liebelt EL, Shannon MW: Small doses, big problems: A selected review of highly toxic common medications. Pediatr Emerg Care 1993;9(5):292
15. Smith AG, Margolis G: Camphor poisoning: Anatomical and pharmacologic study; Report of a fatal case; experimental investigation of protective action of barbiturate. Am J Pathol 1954;30:857
16. Falk W, Hinrichs R: Jacutin poisoning in childhood. Med Klin Wsch 1957;42:1837
17. Kelly JC, Wasserman GS, Bernard WD: Chloroquine poisoning in a child. Ann Emerg Med 1990;19(1):47
18. Edwards M, Russo L, Harwood-Nuss A: Cerebral infarction with a single oral dose of phenylpropanolamine. Am J Emerg Med 1987;5(2):163
19. Conway EE, Walsh CA, Palomba AL: Supraventricular tachycardia following the administration of phenylpropanolamine in an infant. Pediatr Emerg Care 1989;5(3):173
20. Quadrani DA, Spiller HA, Widder P: Five-year retrospective evaluation of sulfonylurea ingestion in children. J Toxicol Clin Toxicol 1996;34:267
21. Shannon M, Lovejoy FH: Effect of acute vs.chronic intoxication on clinical features of theophylline poisoning in children. J Pediatr 1992;121(1):125
22. Henretig F: Special considerations in the poisoned pediatric patient. Emerg Med Clin North Am 1994;12(2):549
23. Osterhoudt KC, Shannon M, Henretig F: Toxicologic emergencies, in Fleisher GR and Ludwig S (eds): Textbook of Pediatric Emergency Medicine, ed 4. Philadelphia, Lippincott Williams & Wilkins, 2000, pp 887942
24. Pond SM, Lewis-Driver DJ, Williams G, et al: Gastric emptying in acute overdose. Med J Aust 1995;163:345
THE AUTHOR is Assistant Professor of Pediatrics, Division of Emergency Medicine, The Children's Hospital of Philadelphia and University of Pennsylvania School of Medicine, and Associate Medical Director of The Poison Control Center, Philadelphia.
Kevin Osterhoudt. The toxic toddler: Drugs that can kill in small doses.
Contemporary Pediatrics
2000;3:73.




















