Treating infection in burns
Most pediatric burns are small and can be managed by primary care physicians. However, knowing when to contact a local burn center for assessment and treatment of burn injuries can minimize adverse outcomes and optimize care for the burn-injured child.
If all types of burns are considered, there is scarcely a child who has not been burned. Burns most commonly occur during routine activities of daily living and play. Sources of injury include scalds, fire, chemicals, radiation, electricity, and hot objects.1 Scald burns (hot foods or drinks, showers, or tubs) are the most common type of burn among children aged younger than 5 years; older children, adolescents, and teens may be more likely to suffer a burn from fire (candles, matches, lighters, and house fires).1 Fortunately, most burns are small, heal spontaneously, and can be adequately managed in the outpatient setting by the general pediatric practitioner. Some burns, however, can be large or associated with infections and long-term sequelae such as scarring. Therefore, all providers should be familiar with the assessment and treatment of burns to minimize the risk of adverse outcomes. This article focuses on burns and infections relevant to primary care pediatric practice.
Initial assessment of a burn injury
When a child presents with a burn, it is important to obtain a detailed account of the circumstances and mechanism of the burn injury from the adult caregiver and the child (when possible). Important details to note are the etiology of injury, time interval from the injury to medical treatment, steps used to clean and treat the wound before the evaluation, and presence of other injuries. Should any suspicion of abuse or neglect arise, the patient should be considered for referral to the local child protection authorities. Such cases could include those in which the reported circumstances of injury are unclear, vary when recounted, or are inconsistent with the clinical presentation. Other warning signs include a previous burn injury, delay in seeking care, presence or suspicion of other injuries, and specific patterns such as cigarette burns or scald burns with well-demarcated borders and/or absence of marks to surrounding areas.2
Need for referral
At initial presentation, all burns should be evaluated for anatomic location, size, and depth. These factors are important both individually and synergistically to help determine the
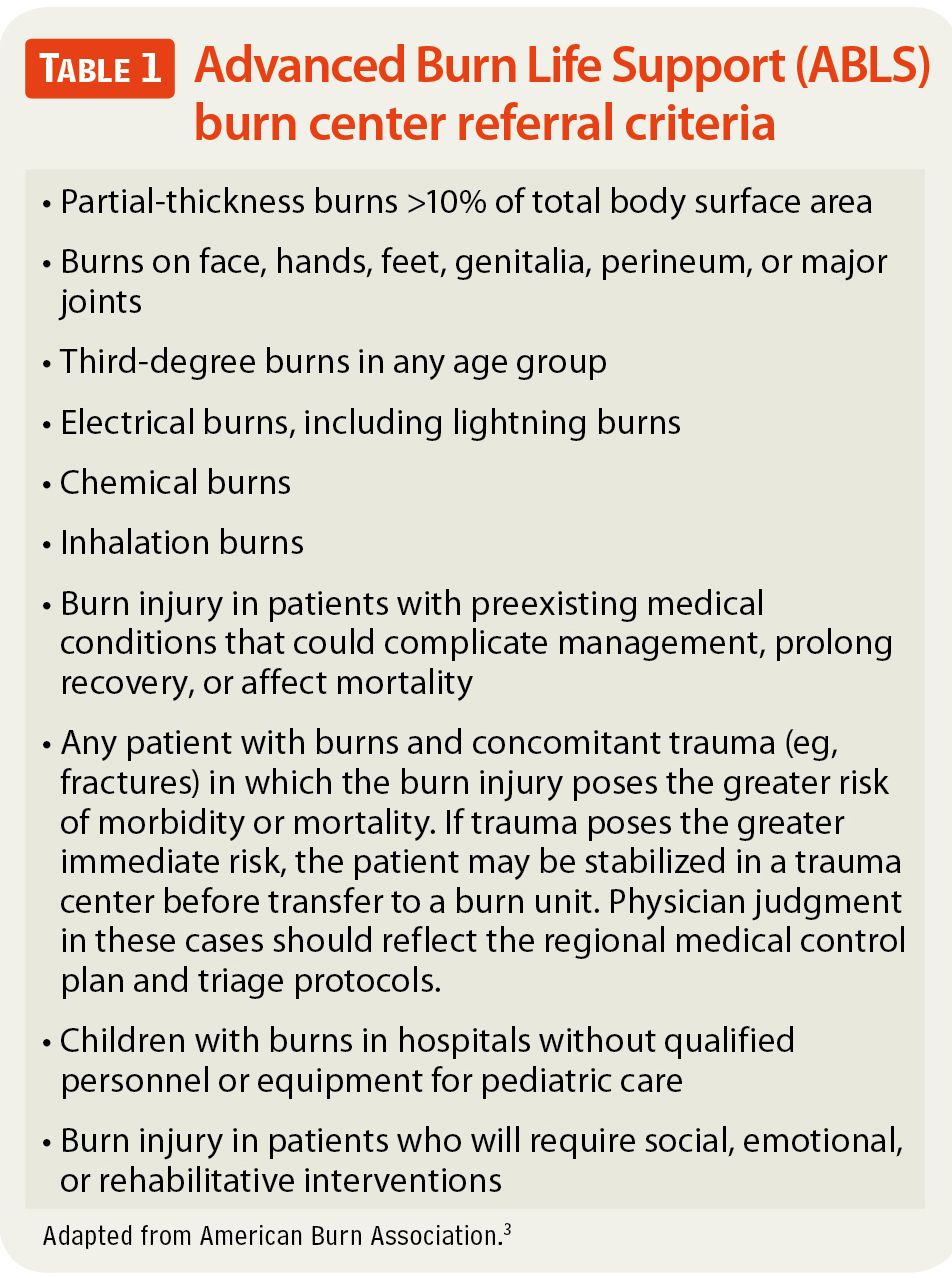
appropriate treatment, including referral to a burn center if needed.3 In particular, pediatricians should refer the patient to a burn center when burns involve the face, hands, feet, genitalia, perineum, or major joints; when partial-thickness burns cover more than 10% of the body surface area; and for any third-degree burn. Children with preexisting medical conditions or burns that will require long-term rehabilitation and social service coordination should be referred to a burn center. Finally, any burn injury involving an electrical, chemical, or inhalational source should be managed in a burn center and not by the primary care pediatrician (Table 1).3
Burn depth
Burns can present as first, second, third, and fourth degree and involve
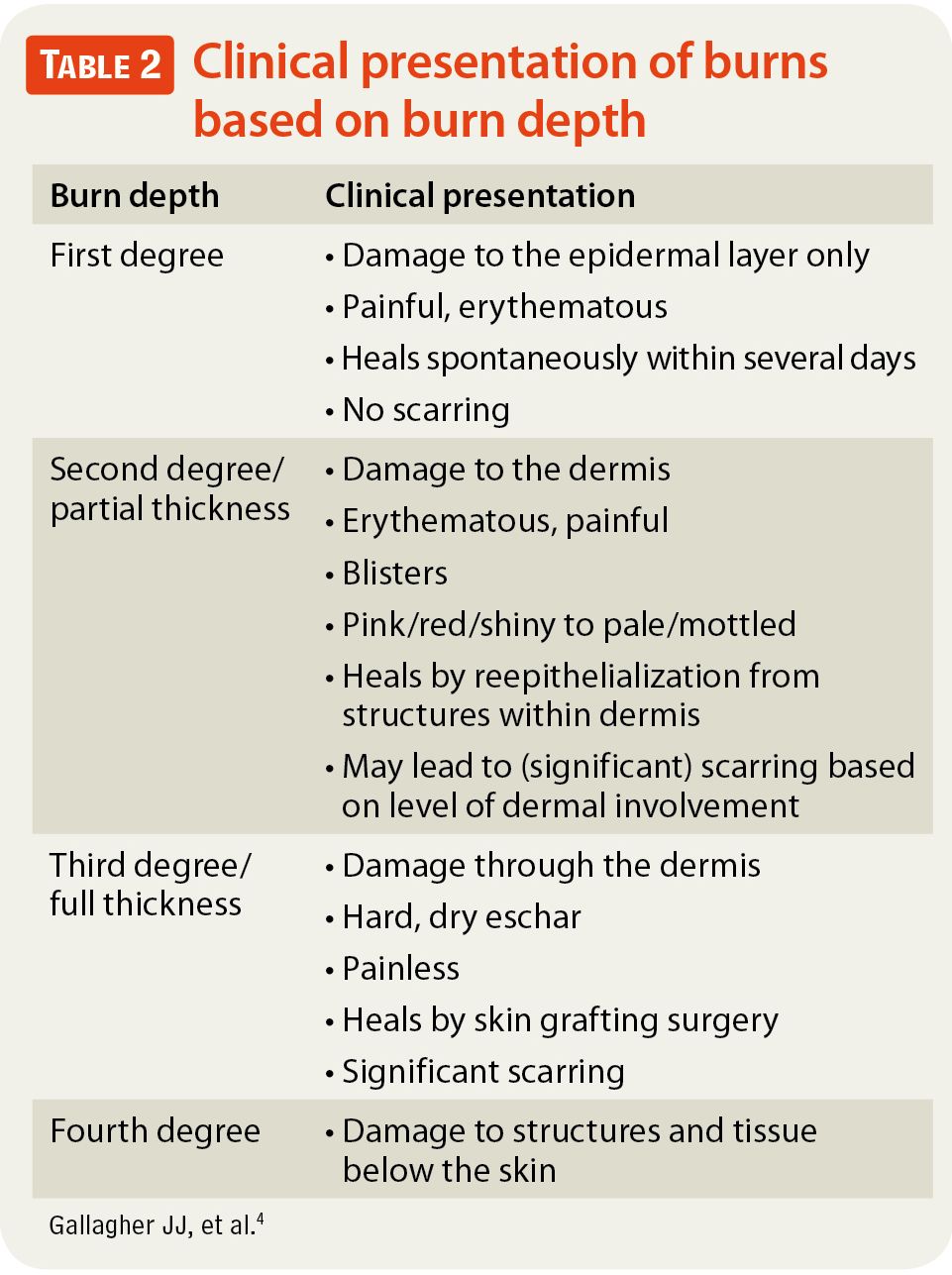
layers from the epidermis through the deep dermis and underlying tissue (Table 2).4 Commonly, burns are of mixed depth, and clinical judgment remains the best tool for determining wound depth and the need for skin grafting.2 To ensure the most accurate assessment of wound size and depth, the burned areas should be thoroughly cleaned and patted dry before visualization. Once dry, the wounds should be inspected for the extent of injury, the development of moisture, and the presence of pain. It is commonly agreed among burn surgeons that the more exudate is present, the higher the likelihood that the wound is superficial and will heal spontaneously. The drier the wound, the more likely it is to be deep and require further intervention. Pain associated with the wound can also provide insight into the depth; significant pain is characteristic of superficial to mid-dermal wounds, whereas minimal pain or absence of pain can indicate nerve damage consistent with deep partial or full-thickness injury.4
Burn size
Burn size can be estimated using various tools, including the “rule of nines,” the Lund and Browder chart, or the use of the palmar surface of the patient’s hand to represent approximately 1% of the total body surface area.4 Regardless of the tool used, estimates of burn size should include only areas of skin loss and exclude areas of first-degree injury.2 Although estimates of burn size often vary between and among providers of different training levels and backgrounds, burns that are less than 10% of the total body surface area pose a low risk of mortality to the patient in most cases.1
Related:DERMCASE diagnosis: ANOGENITAL WARTS
Caring for the burn wound
The goals of wound care are to remove dead tissue and promote healing while minimizing the risks of infection and scarring.
Cleaning and debridement
Basic wound care performed in the outpatient clinic setting should include gentle debridement (use of antimicrobial or mild soap on cotton gauze) as a first step to gently remove loose skin and any existing topical application before wound evaluation. Blisters should be allowed to remain intact.5 If large or interfering with function, blisters are best treated by unroofing and gentle cleansing. Burns should then be evaluated for size, depth, presence of infection, and appropriate topical antimicrobial treatment.
Topical and antimicrobial therapy
Silver sulfadiazine (SSD) offers broad-spectrum coverage and is most often used for middermal to full-thickness wounds with necrosis and in areas distant from mucous membranes (Table 3).4-7 Topical antibiotic ointments such as bacitracin are recommended
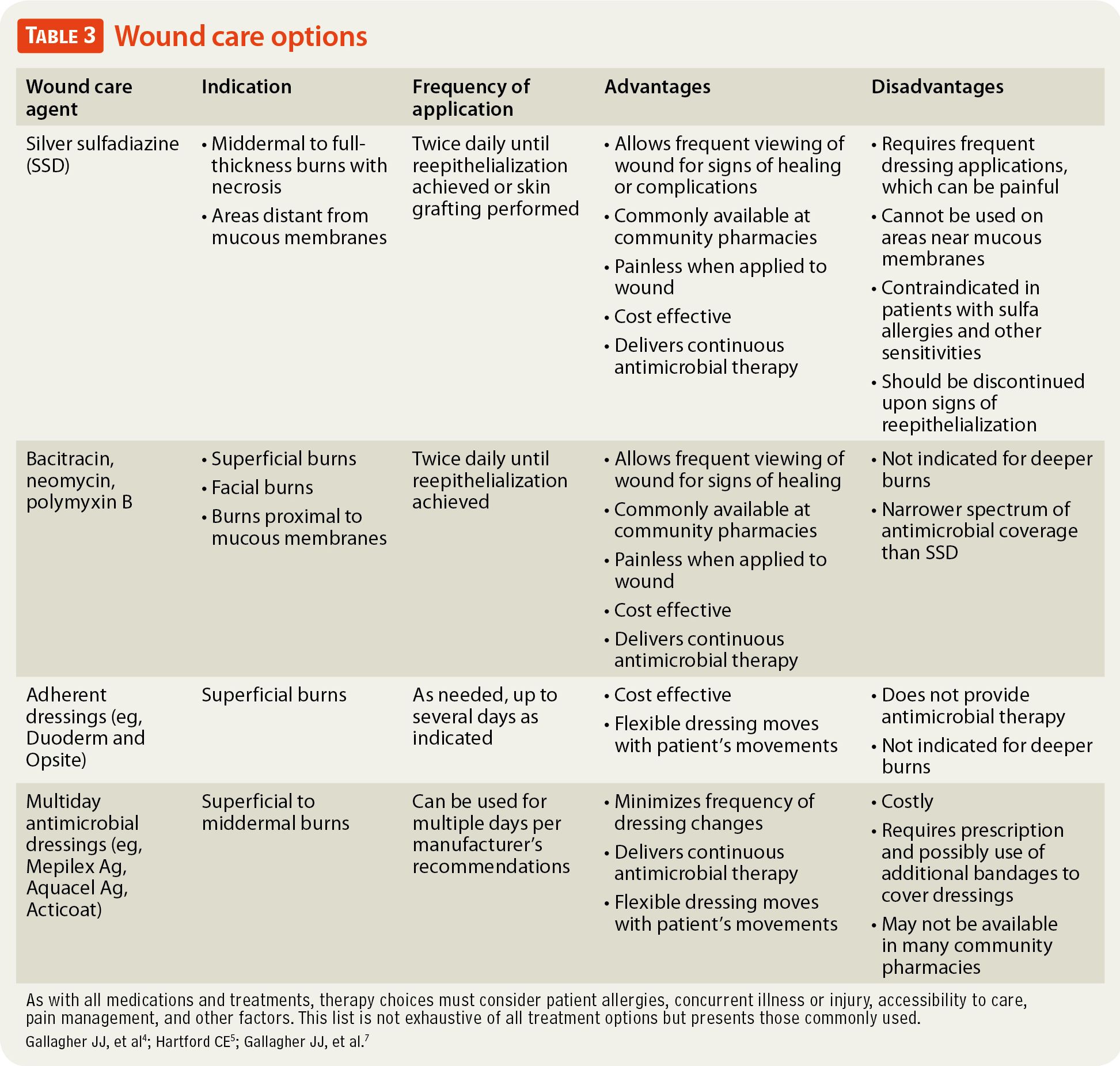
for treatment of superficial burns, burns to the face or areas near mucous membranes, or burns in patients who have sulfa allergies and are unable to tolerate SSD.4,5,8 These agents do not provide the antimicrobial coverage offered by SSD but are cost effective and can be purchased over the counter.4-6,8
Once the topical agent has been applied, the affected area should be wrapped using a minimal amount of petrolatum emulsion-soaked gauze (eg, Adaptic) or nonstick pads and cotton wrap dressings (eg, Kerlix, Kling) to absorb the exudate while keeping the topical application in contact with the wound and protecting the area.4-6 The parent should be taught this routine and then continue this care twice daily until the follow-up visits when the provider judges the skin to have reepithelialized. Wounds that do not heal within 14 to 21 days or those that appear to be full thickness should be referred for grafting, preferably at a burn center.5
As an alternative to a twice-daily wound care regimen, multiday dressings can be used for uncomplicated burn injuries. Adherent occlusive dressings can be used safely for several days in superficial wounds. Such products include Duoderm and Opsite, which cover the wound but do not offer antimicrobial protection.4,5 Clinical experience shows that these dressings are well suited for placement onto a wound that has a border of intact skin to anchor the dressing.
Newer to the dressing-care market are multiday antimicrobial dressings (such as Mepilex Ag, Aquacel Ag, and Acticoat), which are put onto a clean, superficial to middermal burn wound and left in place to maintain the moist environment, thereby facilitating antimicrobial delivery. Each dressing should be kept in place for several days according to the manufacturer’s recommendations, barring any suspected complications. These dressings obviate the need for daily wound care and thereby reduce pain.7,9
Regardless of the wound care regimen used, patients, families, and providers must be aware that an evaluation by the clinician for a wound check is indicated if signs and symptoms of wound infection occur. If the wound develops purulent discharge, a change in color or odor, or erythema, the child should return for further evaluation and treatment.7
Infectious complications: What to look for and when to treat
The burning process itself kills bacteria on the skin surface. In the absence of clinical signs of infection, the routine use of antibiotics in burn injury is not recommended.5,10
Fever
Fever is commonly present after burn injury, although the mechanism is poorly understood. Elevated temperature cannot be relied upon as a sole indictor of infection, even among children with minor burns.11 Only sustained fever for more than 48 hours was significantly associated with infectious complications. In addition, the presence of fever should not automatically mandate an investigation for infection or prescription of an antibiotic. However, in daily practice, providers should be aware of common generalized signs of worsening infection, such as mental status changes, tachypnea, decreased oral intake, decreased urine output, increased pain, and changes in the wound as described below.
Tetanus
As a matter of routine, a burn-injured patient should be considered for administration of tetanus toxoid if the date of the last dose received is unknown or if the patient’s last dose of toxoid or booster was more than 3 years or 10 years ago, respectively.7
Burn wound erythema versus cellulitis
Burn wound erythema can be a normal part of burn pathophysiology. This painless, benign erythema characteristically occurs 3 to 5 days after the initial injury, surrounds the injury to within 2 cm of the burn edge, and subsides spontaneously.7 Recognition of this entity is important to decrease the unnecessary use of antibiotics and to differentiate it from burn wound cellulitis.
Burn wound cellulitis presents with advancing erythema, warmth, and tenderness, which must be distinguished from the initial blanching appearance of burn wound erythema. The most common organism is Staphylococcus aureus, and appropriate antibiotics should be initiated with close follow-up.7 If the cellulitis does not respond to oral antibiotics or affects a large area, if additional infection is suspected, or if the patient and family are unable to secure follow-up care, the burn-injured child should be transferred to a burn center. A wound with surrounding cellulitis should not be considered for a multiday dressing; instead, twice-daily wound care with washing and topical ointments is the preferred treatment for these burns. The clinical suspicion of infection should be addressed as soon as possible because inadequate treatment of a burn wound infection can lead to adverse systemic consequences and deepen the wound, thereby increasing the likelihood of scarring and possibly the need for surgery.
Severe infections
More severe forms of burn wound infection are commonly limited to large burns, which

FIGURE Lateral left chest of a child with scald injury on day 10 after the burn. Scalloped epithelial edges are characteristic of viral infection.require the monitoring and expertise of a burn center. Some atypical forms of burn wound infections, however, may present in small and superficial burns; for example, herpes simplex virus.12 In these cases, inspection will show an atypical pattern, with the burn wound healing edges scalloped with visible vesicles. A careful history should reveal previous herpes simplex infection in the child. Appropriate antiviral therapy should allow normal healing (Figure).
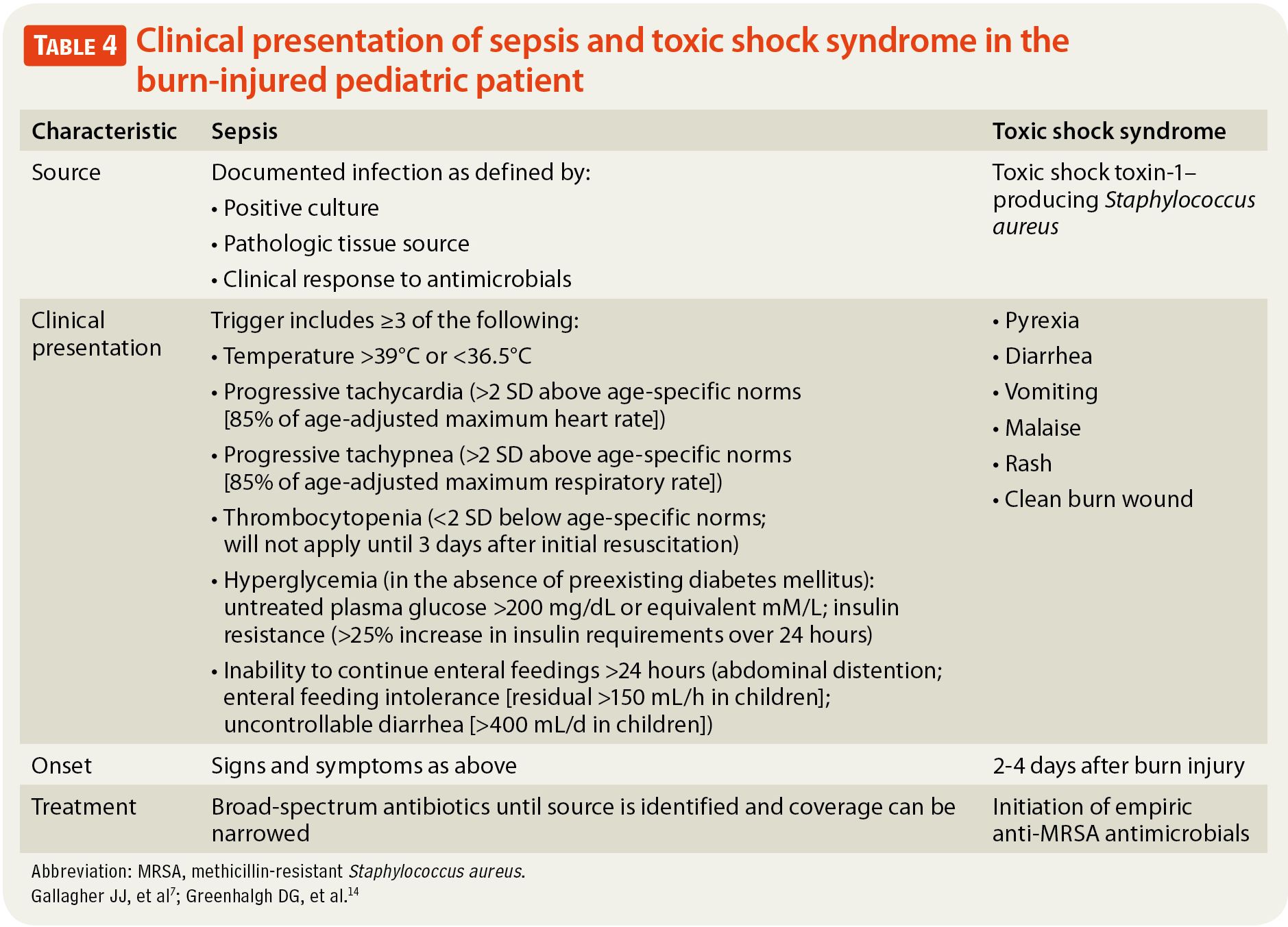
Toxic shock syndrome (TSS) from toxic shock toxin-1–producing S aureus is a rare but serious complication of burn infection that primarily affects young children because of their lower levels of protective antibodies.13 Clinical TSS presents with a variety of symptoms, including rash, irritability or lethargy, pyrexia, and shock.7,13 A common scenario of TSS involves a young child with a small burn who experiences rapid deterioration; the condition can become life threatening within hours unless it is recognized and treated promptly.13 Mortality is a significant risk.7 Children with bacterial sepsis deteriorate over 12 to 24 hours, and in most cases respond

FIGURE Appearance of wound after 7 days of treatment with antiviral therapy.to antibiotics13 (Table 47,14). In contrast, children with TSS can deteriorate in 1 to 2 hours and are unresponsive to antibiotics alone.13
The development of shock and suspected sepsis always requires that the wound be inspected and considered as a possible source. However, clinicians should keep in mind that in the case of small and moderate burns, the burn wound itself is not the most common source of infection. Other sources of sepsis, such as recent urinary catheterization, should be considered. In addition, children with burns are part of the general pediatric population, and they can develop a second problem such as appendicitis, respiratory infection, or gastroenteritis.
Management of pain and itching
Most burns can be extremely painful. To treat the pain associated with minor burns, options include narcotics, acetaminophen, or other nonsteroidal anti-inflammatory agents (barring the possibility of surgery) as needed, especially for use as a premedication before wound care.5,15 As the areas heal, itching becomes extremely common among children. This may last 18 months or longer after the burn and may result in scratching to the point of injury and infection of the regenerating tissue.15 First-line treatments include liberal use of a mild lotion (cocoa butter, Elta, Lubriderm, Nivea) or oatmeal baths. Pharmacologic options can include antihistamines given orally or topically.15,16
Care of the healed areas
Areas of healed burns may remain sensitive for months after the initial injury and more prone to traumatic reinjury than areas of uninjured skin. Rough play or specific activities should be limited to prevent tears of the regenerated tissue.16 Although all areas of the body should be protected from the sun with sunscreen, healed burn sites require vigilant use of sunscreen and ultraviolet protective clothing to prevent permanent scarring of those areas. Loose-fitting cotton clothes are preferred to tight-fitting clothes, belts, and elastic-waist pants, which can rub and cause blisters. Patients and families should expect that the color of the healed skin will change over time depending on the child’s original pigmentation, injury depth, and other factors.
Conclusion
The vast majority of burns sustained by children can be managed by primary care pediatricians. However, if a pediatrician is unsure about management at any stage, or if the burn is deep or is developing an infection, he or she should contact the local burn center to arrange transfer for the child. In many cases, the primary care pediatrician can be assisted by a discussion with a burn surgeon who has reviewed a good-quality photograph of the burn injury. Together, they can formulate a plan for optimal care of the burn-injured child.
REFERENCES
1. American Burn Association. 2012 National Burn Repository: report of data from 2002-2011. Dataset version 8.0. Chicago, IL. 2012. http://ameriburn.org/2012NBRAnnualReport.pdf. Accessed July 30, 2013.
2. Gallagher JJ. Burn wound management. In: Cameron JL, Cameron AM, eds. Current Surgical Therapy. 10th ed. Philadelphia, PA: Elsevier Saunders; 2011:1032-1036.
3. American Burn Association. Burn center referral criteria. http://www.ameriburn.org/BurnCenterReferralCriteria.pdf. Accessed July 30, 2013.
4. Gallagher JJ, Wolf SE, Herndon DN. Burns. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice. 18th ed. Philadelphia, PA: Saunders Elsevier; 2008:559-585.
5. Hartford CE. Care of outpatient burns. In: Herndon DN, ed. Total Burn Care. 4th ed. Philadelphia, PA: Saunders; 2012:81e2-92e2.
6. Lexicomp Online. Silver sulfadiazine. Wolters Kluwer Health. http://www.crlonline.com/lco/action/doc/retrieve/docid/nypres_f/249727. Accessed July 31, 2013.
7. Gallagher JJ, Branski LK, Williams-Bouyer N, Villarreal C, Herndon DN. Treatment of infection in burns. In: Herndon DN, ed. Total Burn Care. 4th ed. Philadelphia, PA: Saunders; 2012:137e2-156.e2.
8. Lexicomp Online. Bacitracin. Wolters Kluwer Health. http://www.crlonline.com/lco/action/doc/retrieve/docid/nypres_f/249010. Accessed July 31, 2013.
9. Lee JO, Norbury WB, Herndon DN. Special considerations of age: the pediatric burned patient. In: Herndon DN, ed. Total Burn Care. 4th ed. Philadelphia, PA: Saunders; 2012:405e2-414.e2.
10. Pruitt BA Jr, McManus AT, Kim SH, Goodwin CW. Burn wound infections: current status. World J Surg. 1998;22(2):135-145.
11. Rodgers GL, Kim J, Long SS. Fever in burned children and its association with infectious complications. Clin Pediatr (Phila). 2000;39(9):553-556.
12. Linnemann CC Jr, MacMillan BG. Viral infections in pediatric burn patients. Am J Dis Child. 1981;135(8):750-753.
13. Laabei M, Young A, Jenkins TA. In vitro studies of toxic shock toxin-1-secreting Staphylococcus aureus and implications for burn care in children. Pediatr Infect Dis J. 2012;31(5):e73-e77.
14. Greenhalgh DG, Saffle JR, Holmes JH IV, et al; American Burn Association Consensus Conference on Burn Sepsis and Infection Group. American Burn Association consensus conference to define sepsis and infection in burns. J Burn Care Res. 2007;28(6):776-790.
15. Meyer WJ III, Wiechman S, Woodson L, Jaco M, Thomas CR. Management of pain and other discomforts in burned patients. In: Herndon DN, ed. Total Burn Care. 4th ed. Philadelphia, PA: Saunders; 2012:715-731.e6.
16. New York-Presbyterian Hospital, William Randolph Hearst Burn Center. Parent and caregiver guide. New York, NY. 2011. http://nyp.org/pdf/burn_center/WRH_Burn_Center_Parent_and_Caregiver_Guide_Final.pdf. Accessed July 18, 2013.
IMAGE CREDIT/AUTHOR SUPPLIED
DR MITCHELL is chief resident in general surgery, New York-Presbyterian Hospital/Weill Cornell Medical Center, New York, New York. MS LEAHY is manager, Community Outreach and Professional Education Program, William Randolph Hearst Burn Center, New York-Presbyterian/Weill Cornell Medical Center, New York. DR GALLAGHER is assistant professor of surgery and assistant attending burn surgeon, William Randolph Hearst Burn Center, New York-Presbyterian Hospital/Weill Cornell Medical Center, New York. The authors have been active in developing a pediatric burn unit at New York-Presbyterian Hospital/Weill Cornell Medical Center’s partner hospital in Tanzania, East Africa. They have nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
Subscribe to Contemporary Pediatrics to get monthly clinical advice for today's pediatrician.