A unilateral white pupil in a 6-year-old girl
You are working in your outpatient pediatric clinic, when an apparently healthy 6-year-old girl is brought in with a chief complaint of a unilateral "white pupil" noted on photographs taken at her kindergarten graduation. Prior photographs of the patient had never before revealed this.

On careful history, you learn that the mother delivered a healthy baby without any neonatal problems. The patient’s mother denies infections during pregnancy, and the patient has not had any serious illnesses or hospitalizations. The patient and her mother deny ocular complaints such as visual disturbance, eye pain, proptosis, strabismus, or signs of intracranial dysfunction. The child has not been taking any prescribed or over-the-counter medications. The patient denies having any pets, and she has not had any recent contact with animals. There has been no recent travel.
On review of the patient’s chart, you see that at her recent well-child checkup, her visual acuity was 20/20 in both eyes, and color vision was normal bilaterally. You also see that there is no family history of ocular problems or cancers, and you confirm that this remains true.
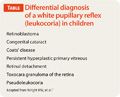
The child’s mother tells you that she performed an Internet search and that her biggest concern is the possibility of a malignant tumor in her child’s eye. You concur with the mother that this is also your most serious diagnosis. You consult several reliable references for additional causes of unilateral leukocoria (Table).1
Physical exam
The patient’s outward appearance and behavior are unremarkable. External examination of the eyes and adnexae reveals no abnormalities. Gaze is central, steady, and maintained. Extraocular muscle function is normal bilaterally (without manifest or latent strabismus). Both pupils are equal, round, and reactive to bright light in a darkened room, and you note that red reflex is present bilaterally on direct ophthalmic exam.
Direct ophthalmoscopy further reveals that the visual axis is clear without any obstructing mass or cataract. The optic disc, macula, and retinal vessels appear to be normal. Visual acuity remains at 20/20 in both eyes, and color vision is normal.
While you consider your differential, you rule out congenital cataracts on the basis of normal visual acuity and lack of pupillary cloudiness on exam. You also confidently rule out Coats’ disease, because not only is this is more common in males, it often presents with visual disturbances and a “yellowish” leukocoria rather than the white pupil you see in the picture.
Being that your patient has had normal vision since birth and has had normal eye exams in the past, persistent primary vitreous can also confidently be removed from your differential. Your concern for retinoblastoma remains, but you are reassured by your inability to visualize any sign of a tumor on the retina via direct ophthalmoscopy.
Based on the benign exam, lack of ocular symptoms, and your inability to reproduce leukocoria on direct ophthalmoscopy, you consider the diagnosis of pseudoleukocoria, a recently described entity that is an artifact of a flash-illuminated digital camera photograph not associated with any ocular pathology.
You explain this along with further reassurance to the patient’s mother but decide to schedule an immediate referral to a pediatric ophthalmologist for confirmation of this less well-known diagnosis.
The patient is evaluated by the ophthalmologist who confirms the benign exam and agrees with the diagnosis of pseudoleukocoria. No diagnostic imaging studies or follow-up office visits are required.
Leukocoria
Unilateral leukocoria (white pupillary reflex) traditionally has been an ominous sign of serious ocular pathology.
Retinoblastoma is the most common primary ocular malignancy in childhood. Early identification is critical because cure rates, after enucleation of unilateral retinoblastoma, are higher than 90% if the tumor is localized within the eye.
The most common presenting signs are leukocoria, the presenting sign in more than 50% of retinoblastoma cases, and strabismus, the presenting sign in about 20% of cases. Thus, the sudden clinical or photographic appearance of unilateral leukocoria warrants a thorough ophthalmologic examination by a primary physician followed by that of a pediatric ophthalmologist.
True leukocoria may be caused by more than 20 additional ocular entities.2 These pathologies include anterior segment pathology such as congenital cataract, posterior segment pathology such as retinoblastoma and Coats’ disease, and mixed anterior and posterior segment pathology.
Persistent hyperplastic primary vitreous (PHPV) is a congenital, unilateral, microphthalmic eye disease of full-term infants in which remnants of the embryonic vitreous and its hyaloid vasculature fail to involute completely during fetal life, leading to fibrosis, cataract, elongation of the ciliary processes, secondary glaucoma, and retinal detachment. There is loss of unilateral vision in most children with this condition.3
Toxocara endophthalmitis is caused by the migration of immature canine roundworm larvae (Toxocara canis), leading to an intense, opaque, inflammatory reaction in the posterior segment of the eye.
Congenital Coats’ disease, in which retinal telangiectasia and aneurysmal retinal blood vessels leak a lipoproteinaceous subretinal transudate, leads to bullous retinal detachment.4
High-grade retinopathy of prematurity (ROP) is a proliferative vascular disease that may result in retinal detachment. Congenital chorioretinitis can be caused by Toxoplasma gondii, rubella, or cytomegalovirus infections.
The greatest difficulty for pediatric ophthalmologists is in the differentiation between retinoblastoma, Coats’ disease, and toxocara granuloma of the retina.5
Unilateral pseudoleukocoria (false white pupil) is better known as photoleukocoria. This optical phenomenon is most commonly seen in a flash-illuminated, digital photograph (with suppression of red reflex option) of a child who is looking away from the camera lens at an approximate angle of 15 degrees.6-9
On thorough ocular examination of the child, there is no leukocoria, proptosis, strabismus, or opaque mass in the ocular lens, vitreous, or retina. The reason given for photoleukocoria is that the optic nerve appears white under bright illumination. If light is shined into the eye from an oblique angle of approximately 15 degrees while the child is looking toward his or her nose, the bright white light reflected from the optic nerve may fill the pupillary opening on the photograph, producing the appearance of true leukocoria.
Approach to a patient with a white pupil
A careful current, past, prenatal, and family history must be obtained from the parent and, when possible, from the child. To best evaluate a red reflex, use a direct ophthalmoscope positioned 2 to 3 feet away from the child’s face in a darkened room. If a parent reports an abnormal red reflex, but it is not apparent when shining the light from straight ahead, assess and compare each red reflex as you move the ophthalmoscope from side to side.
There is a clear distinction between corneal opacity from congenital glaucoma and leukocoria. If the details of the iris and pupil are clearly seen on exam, then the opacity is behind the pupil and is thus leukocoria.
Patients with suspected or definite leukocoria require a thorough ophthalmologic evaluation, preferably by a pediatric ophthalmologist.1 Because of the serious consequences of mistaking true leukocoria for photoleukocoria, it is recommended that children with a suspected diagnosis of photoleukocoria be urgently examined by an ophthalmologist.10
Our patient
The obvious image of a unilateral white pupil will be incongruent with the normal findings obtained during a careful examination of the eye. Although pseudoleukocoria is a completely benign artifact of digital photography, it still warrants immediate evaluation. As health care providers and the general population more frequently recognize this photographic phenomenon, it could eventually lead to less urgency in investigating the cause of white pupil.
Although this condition is not rare, the current recommendation is to refer all such children for thorough eye examination, preferably by a pediatric ophthalmologist.
What happened with this patient illustrates what is the standard of care. Photoleukocoria will more often than not be benign pseudoleukocoria, but leukocoria in photographs remains 1 of the most common presenting symptoms of many serious, and even grave, diagnoses.
References
1. Wright KW, Farzavandi S. Leukocoria: cataracts, retinal tumors, and Coats disease. In: Pediatric Ophthalmology for Primary Care. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2008:285-310.
2. Shields JA, Parsons HM, Shields CL, Shah P. Lesions simulating retinoblastoma. J Pediatr Ophthalmol Strabismus. 1991;28(6):338-340.
3. Pollard ZF. Persistent hyperplastic primary vitreous: diagnosis, treatment and results. Trans Am Ophthalmol Soc. 1997;95:487-549.
4. Edward DP, Mafee MF, Garcia-Valenzuela E, Weiss RA. Coats’ disease and persistent hyperplastic primary vitreous. Role of MR imaging and CT. Radiol Clin North Am. 1998;36(6):1119-1131.
5. Shields JA, Shields CL. Differentiation of coats’ disease and retinoblastoma. J Pediatr Ophthalmol Strabismus. 2001;38(5):262-266.
6. Marshall J, Gole GA. Unilateral leukocoria in off axis flash photographs of normal eyes. Am J Ophthalmol. 2003;135(5):709-711.
7. Russell HC, Agarwal PK, Somner JE, Bowman RJ, Dutton GN. Off-axis digital flash photography: a common cause of artefact leukocoria in children. J Pediatr Ophthalmol Strabismus. 2010. Epub ahead of print.
8. Murphy D, Bishop H, Edgar A. Leukocoria and retinoblastoma-pitfalls of the digital age? Lancet. 2012;379(9835):2465.
9. Pesin N, Noble J, Gallie BL. Question: can you identify this condition? Answer: leukocoria. Can Fam Physician. 2010;56(2):155-156.
10. Lueder GT. Abnormal red reflex. In: Pediatric Practice. Ophthalmology. New York: McGraw-Hill Medical; 2011:114-117.