Unusual Skin Elasticity, Joint Hypermobility, Violaceous Plaques in 3 Different Patients: What’s Your Diagnosis?
Digital extension; joint hypermobility; skin elasticity with keloid scars; pectus and scoliosis from skeletal flexibility and deformation; these disparate symptoms and findings point to what diagnosis?
Case 1. A 16-year-old girl visits her obstetrician for her first prenatal visit. Her genetic history questionnaire notes that her mother has chronic fatigue syndrome with arthritis, migraines, and irritable bowel syndrome. Her mother also has anxiety disorder and is viewed by the family as a hypochondriac. The obstetrician notes joint hypermobility and unusual skin elasticity on examination (Figure, A-C) and tells the girl that he would like her to see a cardiologist even though she has never had signs or symptoms of heart disease.



Figure:
Digital extension (A) and joint hypermobility (B); skin elasticity (C) with “cigarette-paper”
Case 2. A 12-year-old girl is evaluated by an orthopedist because of frequent fractures and dislocations, particularly affecting her left knee that prevent her from participating on an elite soccer team. She was a “rubber-band” baby according to her mother, able to hold her bottle with her feet and often sitting in the “W” position. She required glasses for myopia at age 4 and will be starting orthodontic treatment for crowded teeth. She was delayed in her motor milestones and was very clumsy, with many falls when learning to walk. She can “pop” many of her joints and shows off by turning her elbows completely anterior and joining her hands, one over her shoulder, the other around her back. She has had 6 fractures of her wrists, elbows, and ankles, and frequently sprains her ankles.


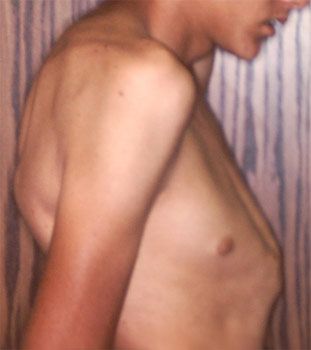
Figure:
(D) or keloid (E) scars; pectus and scoliosis due to skeletal flexibility and deformation (F)
Examination shows soft skin; a white scar with fine wrinkles over a site of fracture repair (Figure, D); and joint hypermobility, including the ability to bend her fingers back over 90 degrees and to touch her palms to the floor. She also had scoliosis of 8 degrees (Figure, F). X-rays films of her knees show lax ligaments and an area of dead bone on her lower left tibia; her hips show some joint erosion.
Case 3. A 2-year-old boy is evaluated by a pediatrician for motor delays because he is only now beginning to walk. He has a broad based and wobbly gait, prompting concern about a myopathy. Speech is normal. His physical examination seems otherwise normal except for many violaceous plaques over pressure points and some scars with purplish edges on his forehead, elbows, forearms, and knees (eg, Figure, E). His mother says he is very clumsy and falls frequently, and has required stitches on several occasions. She seems very intense and begins relating her own health problems, which have included disabling back and joint pain with need for vertebral fusion; dizziness on standing with occasional syncope, hypotension, and fatigue; abdominal pain with constipation or diarrhea (diagnosed as gastroparesis); frequent migraines that she attributes to poor circulation because she has Raynaud phenomenon and pooling with discoloration in her pelvic area; metrorrhagia with endometriosis that led to hysterectomy after her son’s birth. Prior physicians raised concern about maternal mental illness and child abuse, but this pediatrician ascertains that the boy was premature and diagnoses a familial illness.
To what common diagnosis do these disparate symptoms and findings point?
(Answer and discussion on following page.)
ANSWER: Ehlers-Danlos Syndrome
All of these patients exhibit signs and symptoms of connective tissue dysplasia or weakness caused by various degrees of Ehlers-Danlos syndrome (EDS).
It is important to recognize EDS in pregnant women (Case 1) so as to anticipate such complications as premature delivery, postpartum hemorrhage, cardiac valve leakage, and uterine or bladder prolapse. Hypermobility (Figure, A-B) or skin changes (C-E) are key features, heralding a broad range of potential medical complications (Table) illustrated by the early myopia, orthodontic needs, frequent fractures/dislocations (Case 2), and migraines, irritable bowel syndrome, and orthostatic symptoms (Case 3). Many of these complications can be avoided or ameliorated by anticipatory guidance.
Awareness of these diverse manifestations is required for proper interpretation of the family history (usually autosomal dominant inheritance) and appropriate diagnosis of disabling conditions rather than dismissal as hypochondriasis or mental illness (eg, for the mother of Case 3). Chronic joint pain and the dizziness/fatigue of paroxysmal orthostatic tachycardia syndrome (POTS) can lead to depressive symptoms, just as frequent mitral valve prolapse can lead to panic attacks and anxiety.
Viewed insightfully, the patient in Case 1 has EDS. The mother in Case 3 clearly has EDS, and this is the basis for her son’s prematurity, motor delay, frequent falls/poor coordination from lax joints, and multiple scars. Concerns about myopathy or developmental disability for her son can thus be allayed when his delay in walking is attributed to EDS.
The spectrum can be remembered by the comments of a patient relayed by Dr. Peter Beighton, a pioneer and leader in the field: “When I was a baby they called me a floppy infant, and now the doctors tell me that I am a loose woman.”1
The Broad Clinical Spectrum of Connective Tissue Dysplasia
Although Marfan syndrome and severe forms of EDS (eg, EDS type IV) are viewed as rare diseases, patients with the broader spectrum of connective tissue dysplasia/EDS are commonly encountered in pediatric, obstetric, and primary care.1-4 Connective tissue dysplasia refers to congenital structural deficiency rather than the acquired, inflammatory changes of autoimmune connective tissue/ “collagen vascular” disease (eg, lupus or scleroderma). However, the chronic wear-and-tear joint/vascular injuries of connective tissue dysplasia may overlap with joint inflammation in susceptible individuals. The author has recently seen patients with EDS symptoms who presented with HLA B27-positive ankylosing spondylitis.
Signs and symptoms of EDS can affect the face, eyes, dentition, heart, bones, joints, skin, or vasculature (migraines, irritable bowel syndrome, POTS) and are summarized in the Table.2-6 Severe forms like Marfan syndrome or EDS type IV are prototypes with extreme complications that are paralleled by milder findings in the more common types.5 The severe aortic dilatation/dissection or anterior disc herniation of Marfan syndrome is echoed by milder aortic root prominence, valve prolapse, or frequent disc herniation and the uterine/bowel ruptures of EDS IV are mimicked by endometriosis/metrorrhagia and abdominal pain/irritable bowel syndrome seen in many EDS patients.
Informed interpretation of the family history will often reveal affected males and females; this suggests autosomal dominant inheritance with variable expression that produces a remarkable variety of symptoms in the same family. As with other dominantly inherited conditions, patients with EDS may present as a new mutation without any family history of disease-this absence of family history also occurs with rarer, recessive forms.
Affected individuals usually have one normal and one abnormal allele. The abnormal allele produces a mutated connective tissue protein that has altered shape. The resulting connective tissue “walls” are then constructed from square and curved bricks, producing wobbly structures that are weaker, more deformable, and subject to tearing, hemorrhage, or fracture. Genetic testing initially displayed the altered proteins as with the type I collagens in osteogenesis imperfecta; it then progressed to gene (DNA) diagnosis that is now fairly sensitive for fibrillin mutations in Marfan syndrome. However, the multiple types and at least 30 genes involved in the EDS spectrum do not allow sensitive testing although analysis of selected genes is listed on commercial catalogues. The physician must depend on clinical diagnosis from family and medical history, supplemented by the Beighton score for hypermobility (bending the fingers back, touching hands to floor, etc.) and physical findings like those in the Figures or Table.
Although EDS is classically grouped into types, these are not yet well-correlated with specific molecular mutations or discrete symptoms, and it is more important for the generalist to recognize EDS as a spectrum with multiple clinical implications.5,7 Patients like those described in Cases 1 and 2 with hypermobility might be classified as types II or III, while most patients have the broad, variable symptoms of type I EDS, like the mother in Case 3. Joint hypermobility occurs in children with underlying hypotonia or as a general feature of conditions like achondroplasia where it produces motor delays without cognitive problems, as in Case 3.
Other rare disorders fall into the connective tissue category, including Marfan syndrome, homocystinuria, or osteogenesis imperfecta.8 Recent molecular studies of Loeys-Dietz syndrome have placed the transforming growth factor-beta receptor within the fibrillin pathway and joined its well-known inhibitor (the antihypertensive medicine Losartan) with beta-blockers as treatments for aortic root enlargement.9
This diversity of genetic causes emphasizes that hypermobility is a multifactorial trait, occurring in healthy people but worthy of medical evaluation when extreme or associated with other symptoms. It is common to find individuals with EDS symptoms on both sides of the family; this supports the interaction of several gene mutations in many EDS patients and suggests that comprehensive molecular analyses foretold by exome sequencing will reveal many more EDS types than are listed in current classifications.
Take Home Points
Clinical recognition is paramount because it allows life-enhancing and life-saving strategies.6 Restriction from contact or collision sports is needed for individuals with severe forms of EDS or Marfan who have aortic root enlargement. Emphasis on childhood joint protection can lessen adult arthritis and prevent end-states like fibromyalgia or chronic fatigue syndrome; even teenagers or young adults can become inactive and dysfunctional when faced with chronic pain or cardiogenic lethargy. Weight loss and moderate weight-training can lessen joint load and enhance muscular protection of lax joints. Activities such as swimming as opposed to jogging or cross-country running can lessen joint damage, as can braces on extremity joints with vigorous exercise.
Treatment of frequent sprain/dislocations with RICE (Rest, Ice, Compression, Elevation) and education for individuals to “keep in touch” with their joints will preserve necessary function and activity. Alertness for dizziness on standing, sudden fainting, sensitivity to overheating (particularly after showers), and salt-craving can identify POTS symptoms that respond to hydration/saline or even fludrocortisone/beta-blocker therapies. Attention to hydration and bland diets, even gluten exclusion, also diminishes GI symptoms of hypomotility. Recognition of EDS in children often serves as important therapy for parents and other relatives, because it explains the child’s diverse and disabling symptoms and rescues them from diagnoses like hypochondriasis, psychogenic illness, or malingering.
References:
References:
1. Steinmann B, Royce PM, Superti-Furga A. The Ehlers-Danlos syndrome. In: Royce PM, Steinmann B, eds. Connective Tissue and Its Heritable Disorders. New York: Wiley-Liss. 1993:351-408.
2. Ehlers Danlos National Foundation. www.ednf.org.
3. Adib N, Davies K, Grahame R, et al. Joint hypermobility syndrome in childhood. A not so benign multisystem disorder? Rheumatology (Oxford). 2005;44:744-750.
4. Volkov N, Nisenblat V, Ohel G, et al. Ehlers-Danlos syndrome: insights on obstetric aspects. Obstet Gynecol Survey. 2007;62:51-57.
5. Beighton P, De Paepe A, Steinmann B, et al. Ehlers- Danlos syndromes: revised nosology, Villefranche 1997. Am J Med Genetics. 1998;77:31-37.
6. Wilson GN, Cooley WCC. Connective tissue disorders. In: Preventive Health Care for Children with Genetic Conditions. Providing a Primary Care Medical Home. 2nd ed. Cambridge: Cambridge University Press, 2006; 413-436.
7. Numbers following the disorder access the relevant entry in Online Mendelian Inheritance in Man. www.ncbi.nlm.nih.gov/omim. EDS type I classical (130000); EDS type II classical (130010); EDS type III hypermobility (130020) EDS type IV vascular (225400); EDS type VI ocular-scoliosis (229200); EDS type VIIA, B arthrochalasis (130060); EDS type VIIC dermatosparaxis (225410); EDS type VIII periodontal (130080).
8. Marfan syndrome (154700); homocystinuria (236300) osteogenesis imperfecta (166210); Beals contractural arachnodactyly (121050); Loeys-Dietz syndrome (609192); Pseudoxanthoma elasticum (264800) Stickler syndrome (108300); Larsen syndrome (150250).
9. Pyeritz RE. A small molecule for a large disease. New Engl J Med. 2008;358:2829-2831.
10. Eisenstadt L. What is exome sequencing? www.broadinstitute.org/blog/what-exome-sequencing; accessed 4-12.