Why is this baby blistering?
A 7-month-old child appears at the derm office with a blistering eruption that started six days before on her face and neck, and has spread to trunk and extremities.
» How would you treat him?
» What's the diagnosis?


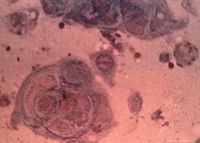
From the clinical appearance, the diagnosis of eczema herpeticum (EH) was made. Viral skin culture from the initial visit later grew herpes simplex virus type 1.
Clinical findings
EH, also known as Kaposi's varicelliform eruption (KVE), results from cutaneous dissemination of herpes simplex virus in the setting of a preexisting skin condition such as atopic dermatitis.1 KVE can also occur as a complication of smallpox vaccination, in that case it is referred to as eczema vaccinatum (EV). However, the most common etiology of KVE is herpes simplex virus (HSV), with HSV-1 more common than HSV-2. The virus often spreads quickly by autoinoculation over the areas with involvement of the underlying skin eruption. Moreover, in the setting of atopic dermatitis, the skin disease does not have to be severe, prompting investigators to suggest that atopics may be predisposed to develop disseminated herpes virus infections.
The key to EH diagnosis is correct identification of the primary lesions, which are uniform clustered 2- to 3-mm crusted vesicles. Conditions such as psoriasis, seborrheic dermatitis, immunobullous dis-orders, and burns may also lead to primary disseminated cutaneous HSV infection.
When not diagnosed and treated correctly, EH may be associated with serious complications such as herpetic keratitis with resulting visual impairment, bacterial superinfections, and widespread systemic dissemination of the virus.2 Prompt initiation of intravenous acyclovir is recommended. In older children who do not have involvement of the mouth, oral valacyclovir may be an effective alternative.
Differential diagnosis
The differential diagnosis for EH includes bullous impetigo, arthropod bites, scabies, papular urticaria, varicella, bacterial superinfection of atopic dermatitis, and disseminated herpes zoster. EH's clustered uniform crusted vesicles will help differentiate EH from these other disorders. EH should be considered in any patient with atopic dermatitis who presents with exacerbation of the underlying skin disease and fever.
Although the factors that predispose atopics to EH is unknown, some researchers propose that infection is likely due to inadequate cutaneous and extracutaneous immune response to the viral infection.3,4
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.