How to diagnose shoulder injuries in young athletes
Arm pain is a common complaint in young athletes but playing though shoulder pain can have serious consequences. Here is guidance for diagnosing shoulder pain and helping these players get their game on.
Figure 1
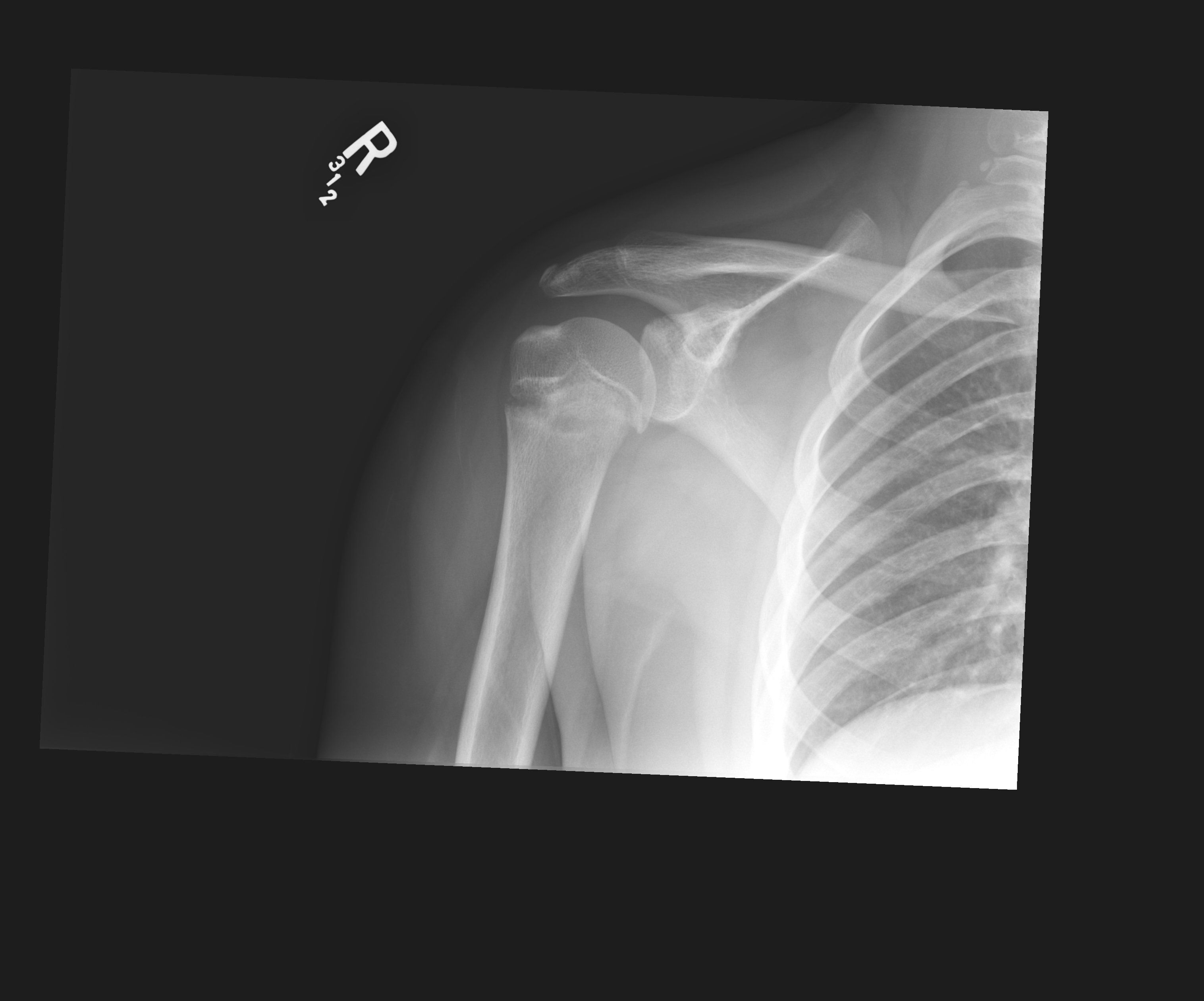
Figure 2a
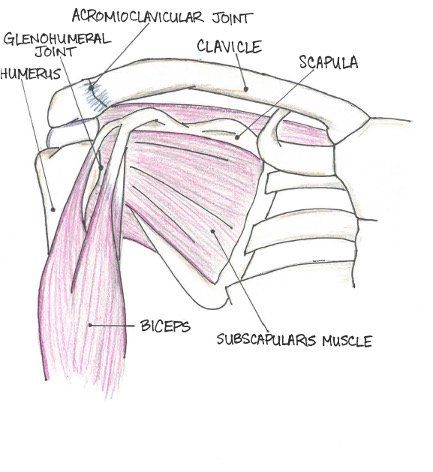
Figure 2b
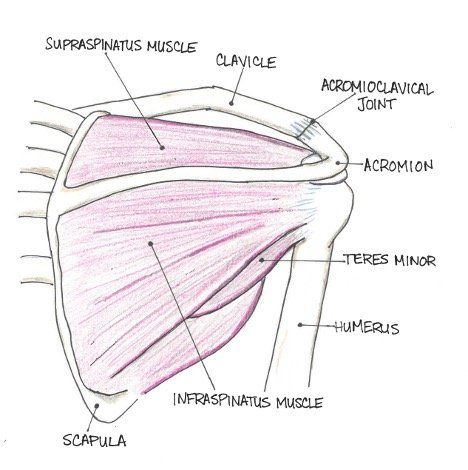
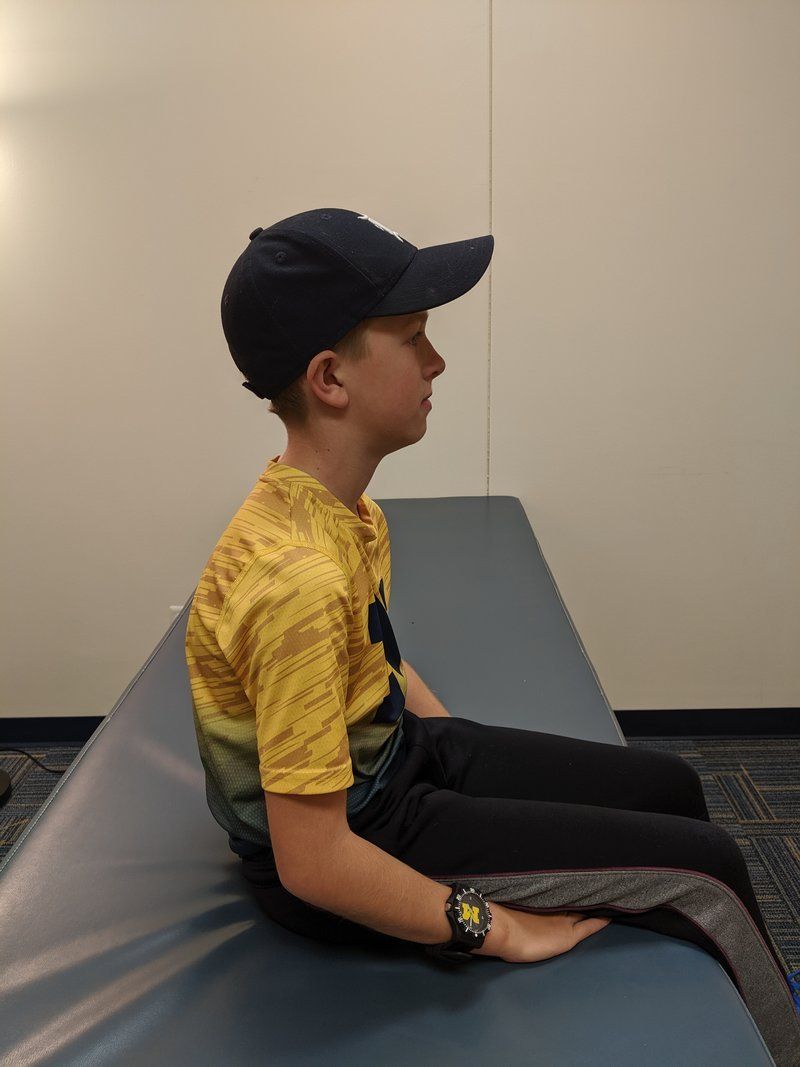
Figure 3
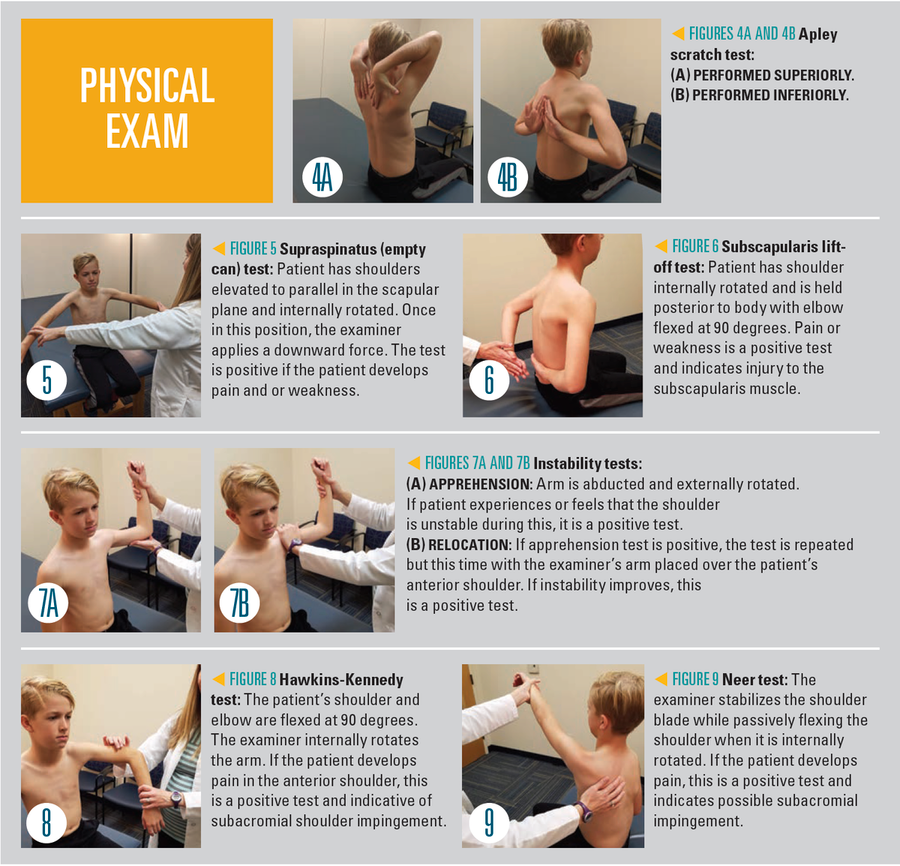
Physical exam
10a
10b
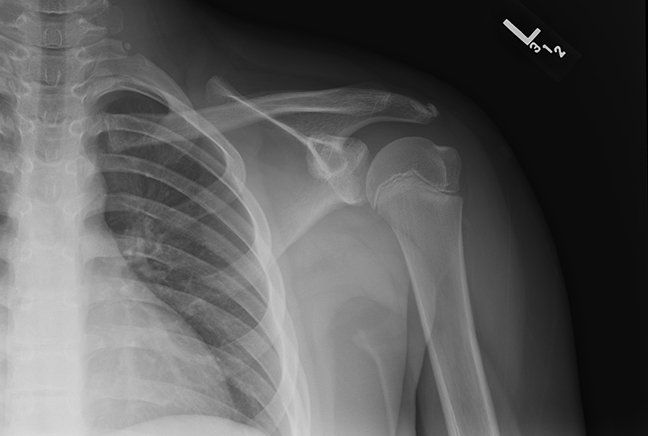
Figure 11
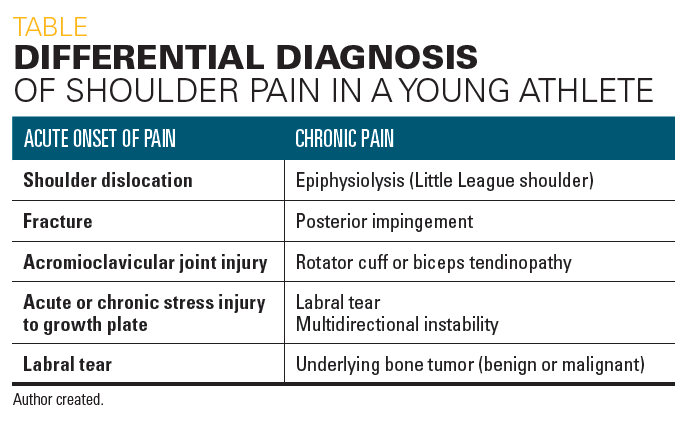
Table
The case
A 12-year-old, right-hand dominant male travel baseball player presents to your clinic complaining of right shoulder pain. He is a pitcher and also plays the catcher position. His pain has been present for 3 weeks and is located “in his shoulder joint.” He has no neck or elbow pain. The patient denies a history of trauma, shoulder dislocation, or shoulder instability. He reports that he is unable to throw as hard or as accurately as he was able to prior to the onset of this pain, and that no specific throw type exacerbates his pain. This athlete has stated that he has multiple upcoming tournaments, that he “is the star pitcher for his team,” and “that he cannot sit out from playing baseball and his team needs him.”
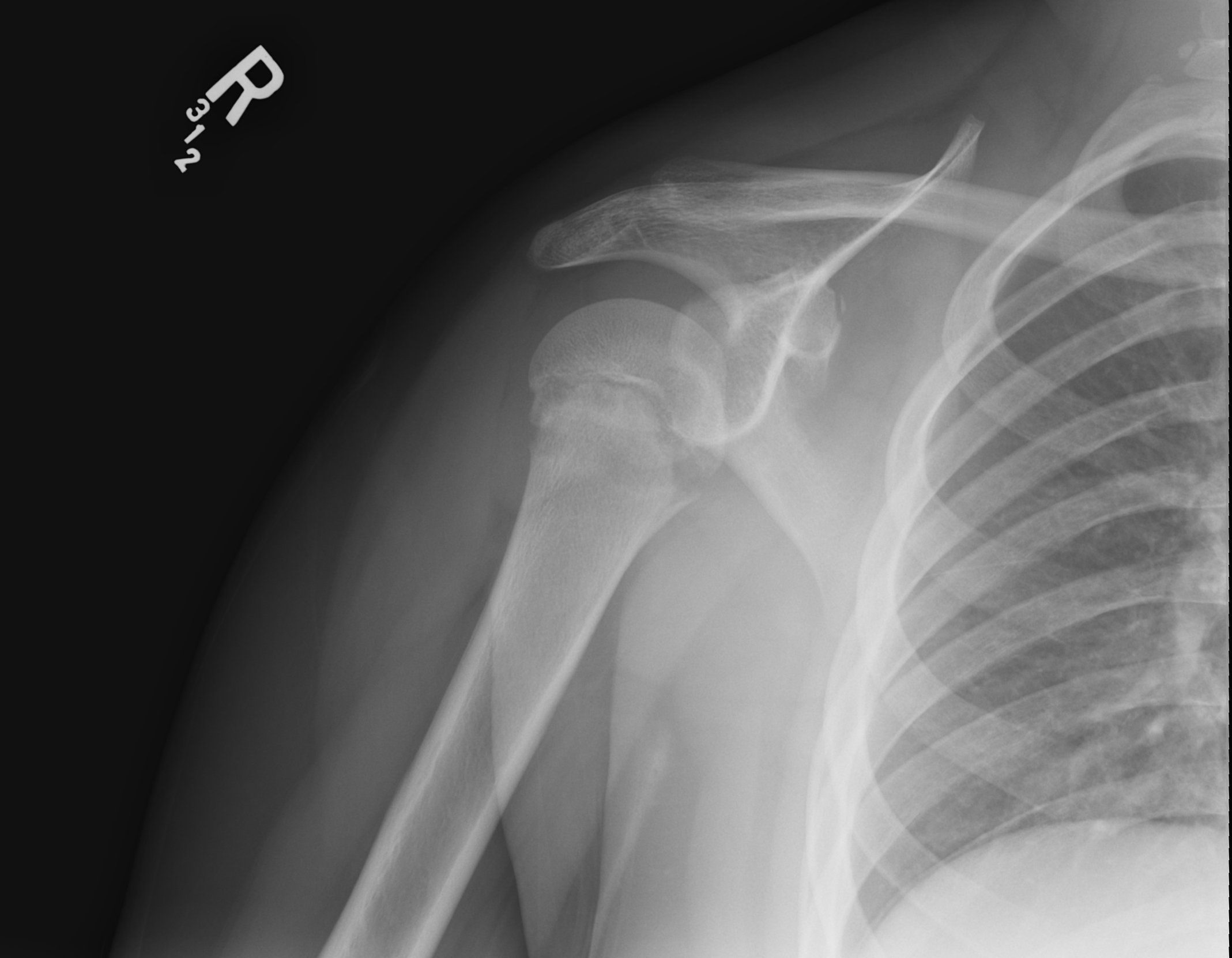
Your exam reveals tenderness on palpation of the right proximal humerus and pain with resisted internal and external rotation of the shoulder. He also has very poor posture with forward-slumped shoulders. You obtain radiographs of his shoulder that demonstrate widening of the proximal humeral physis (Figure 1).
Introduction
Arm pain is a common complaint in overhead-throwing athletes. In a survey of youth baseball players, only 26% reported that they did not have arm pain while throwing.1 Throwing a baseball applies sheer torsional stress on the proximal humerus and valgus stress on the medial elbow. Shoulder pain is a common presenting complaint in young athletes, particularly with recurrent overhead arm movement, not only in baseball and softball but also commonly in swimming, tennis, and volleyball. Other sport activity where upper body motion is not as repetitive yet with high risk for falls and direct blows to the shoulder include football, hockey, wrestling, and winter sports such as skiing and snowboarding.
The shoulder is a ball-and-socket joint that allows a large range of motion. However, it is relatively unstable. This joint is made up of a large humeral head fitting into the small glenoid fossa of the scapula. The labrum is a fibrocartilaginous cup that helps deepen the socket of the shoulder joint to increase stability. Glenohumeral ligaments and the joint capsule are static stabilizers.
Dynamic stabilizers are muscles that allow movement but are also needed to help keep the joint stable. They consist of the rotator cuff muscles (supraspinatus, infraspinatus, subscapularis, teres minor) and scapular stabilizers (trapezius, pectoralis minor, and serratus anterior muscles). Strong scapular stabilizers are essential to help with the motion and function of the rotator cuff (Figures 2A and 2B).
Differential diagnosis
Differential diagnosis for shoulder pain can be helpful to think about in terms of whether there is an event that caused an acute onset of pain or if the pain is chronic. Acute pain could be due to clavicle fracture; acromioclavicular joint sprain; shoulder (glenohumeral) joint dislocation or subluxation; labral tear; proximal humeral fracture; or contusion. Our athlete in this case did not have acute onset of pain, and these injuries are therefore not included in his differential diagnosis.
In contrast, insidious onset of pain in a young athlete typically is due to overuse injury from repetitive stress applied to a tendon, bone, growth plate, or fascia. Differential diagnosis of insidious symptom onset that results in chronic shoulder pain includes impingement, rotator cuff tendinopathy, biceps tendinopathy, labral tear, epiphysiolysis of the humeral head, and multidirectional instability.
Tumors also are possible and may present with pain that has a gradual onset or that may be acute in the instance of a pathologic fracture. Benign tumors include unicameral bone cysts, chondroblastoma, osteochondroma, enchondroma, and periosteal chondroma. Osteosarcoma is the most common malignant tumor of bone in adolescents followed by Ewing sarcoma. Other causes of shoulder pain may be referred pain from cervical, myocardial, or abdominal injury/pain. The Table outlines the differential diagnosis for shoulder pain in a youth athlete.
Little League shoulder
The patient described in this article has a classic history, physical exam, and radiographic findings of Little League shoulder (proximal humeral epiphysiolysis), an injury to the proximal humeral growth plate and unique to a skeletally immature athlete. Growth plates are 2 to 5 times weaker than bone and their surrounding ligament and tendon attachments, and they are prone to injury. Little League shoulder also may be described as proximal humeral epiphysiolysis, epiphysitis, or Salter-Harris type 1 injury to the proximal humeral physis.
The injury is due to repetitive overhead rotational stress that, as the name suggests, is most often seen in baseball or softball players but that also may occur in swimmers, tennis players, gymnasts, and volleyball players. It is most common in athletes aged between 10 and 14 years. In Little League shoulder, athletes will report insidious onset of pain with throwing or overhead activity. They may also report loss of velocity or accuracy with throwing. The diagnosis is clinical and made when a young athlete has tenderness on exam over the proximal humeral growth plate. Radiographs may or may not demonstrate widening of the growth plate.
Rotator cuff tendinopathy, biceps tendinopathy, or shoulder impingement also would be a consideration in this patient as these diagnoses can be frequently seen in overhead-throwing athletes. However, this patient is skeletally immature and has tenderness on palpation over the proximal humeral physis, which is consistent with the diagnosis of Little League shoulder. He does not have a history of shoulder dislocation or subluxation events making the diagnosis of shoulder instability less likely. Multidirectional instability is a condition in which there is increased laxity in both shoulders and that may be present in any direction. This can be an underlying condition that may predispose an athlete to develop shoulder pain. It is treated with rest and physical therapy to strengthen surrounding muscles. The lack of an osseous mass on imaging or an acute fracture in this case excludes other entities in our differential diagnosis.
Physical exam
The physical exam should include inspection of the patient with the shirt off in boys or in a tank top or gown in girls. Visible deformity, swelling, and ecchymosis can be seen with acute trauma such as clavicular fracture or as sternoclavicular or acromioclavicular dislocation. The examiner should take note of the patient’s posture as it may be poor with forward-slumped shoulders potentially contributing to pain or injury (Figure 3). Asymmetric shoulder height may be due to scoliosis, trapezius spasm, or repetitive shoulder use of the dominant arm causing increased strength of the rotator cuff and depression of the ipsilateral shoulder.
Palpation of the shoulder should include the clavicle, acromioclavicular (AC) joint, proximal biceps tendon, proximal humeral head, scapular, and periscapular musculature. Range of motion (preferably active) should be evaluated and may be performed with the Apley scratch test (Figure 4). This test may be performed superiorly, which evaluates abduction and external rotation, or inferiorly, which evaluates internal rotation and adduction. In sports with repetitive overhead motion, such as baseball in particular, there may be an increase in external rotation and loss of internal rotation in the dominant shoulder.
Strength of the rotator cuff muscles should be evaluated, which includes the supraspinatus (empty can) test (Figure 5); subscapularis testing (Figure 6); and resisted internal and external rotation. There are numerous specialized tests that can be performed on the shoulder, including stability tests (apprehension, relocation; Figure 7) and impingement tests (Hawkins-Kennedy, Figure 8; Neer, Figure 9). More testing may be performed in the sports medicine or orthopedic office but are often not necessary in the primary care setting.
Imaging
Initial workup of shoulder pain by a primary care provider should begin with 2 views of the shoulder, typically anteroposterior (AP) and Grashey views. Additional views may be considered by a sports medicine physician or orthopedic surgeon including trans-scapular Y lateral and axillary views. Radiographs should be obtained in instances of acute trauma, pain for longer than 1 month, nighttime pain, and history of instability episodes. When Little League shoulder is suspected, shoulder radiographs may demonstrate widening with adjacent sclerosis of the proximal humeral physis, particularly along the lateral aspect. It can be helpful to obtain a contralateral view as a comparison to better identify the abnormality of the growth plate.
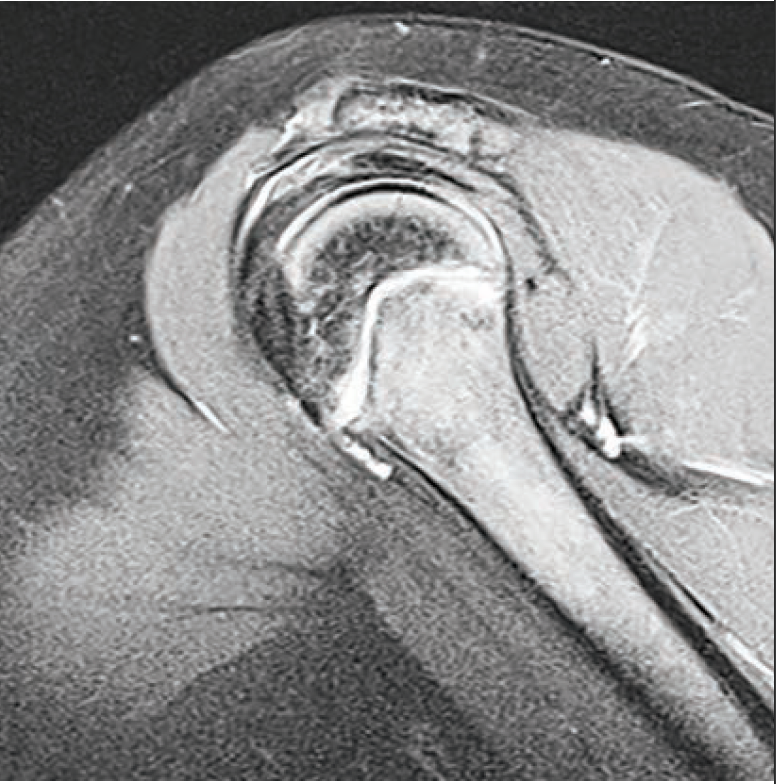
Even if radiographs are symmetric, the diagnosis may still be Little League shoulder if the patient has tenderness on palpation over the proximal humeral physis. Magnetic resonance imaging (MRI) is the most sensitive test for detecting subtle physeal injury although MRI typically is not needed in making a diagnosis of Little League shoulder. If an MRI is obtained, it may demonstrate physeal widening on T1-weighted and non–fat-saturated proton density images, and periphyseal edema on T2-weighted sequence.2
In cases of glenohumeral dislocation, instability, and suspected labral tears, a magnetic resonance (MR) arthrogram should be obtained to fully evaluate the fibrocartilaginous labrum. An MR arthrogram is performed following the image-guided injection of gadolinium-based contrast material into a joint with specific T1-weighted sequences obtained in the MRI scanner. Downsides to obtaining an MR arthrogram include cost, time, need for gadolinium administration, and the invasive nature of the study (injection into the joint performed by a radiologist). If a pediatrician is considering MRI evaluation for chronic shoulder pain in a young athlete with either positive or negative radiographic findings, it is likely time to consider referral to a sports medicine physician or orthopedic surgeon.
In a study in which shoulder MRI was performed on asymptomatic Little League baseball players, 12 of 23 players had positive MRI findings on the dominant shoulder compared with the nondominant shoulder. Most athletes demonstrated widening or periphyseal edema of the proximal humeral physis, but labral tears and partial-thickness rotator cuff tears also were present in high numbers. Risk factors associated with MRI findings were year-round play and players that only participate in baseball.3 Ultrasound may be of benefit to evaluate soft tissue structures including the rotator cuff tendons and presence of joint effusion but do not adequately evaluate the labrum. Ultrasound is unique in that it may offer the opportunity for dynamic evaluation and does not require sedation or radiation.
Treatment
One of the most important aspects of treatment of Little League shoulder is rest from throwing and overhead activities to allow the growth plate to heal. Allowing the athlete to participate in batting as long as it does not elicit pain may be considered. In doing so, it will allow the athlete to remain involved with their team, which is important from a psychosocial standpoint.
Physical therapy is important to work on range of motion, posture, and strength. Strengthening of not only the shoulder muscles, including the rotator cuff, but also scapular stabilizers, hip, core, and lower extremity muscles is important. Correction of posture can be helpful to align shoulders to a neutral position and avoid forward slumping with associated pectoralis tightness and scapular muscle weakness.
Once the patient is pain free and has appropriate strength, a gradual return to a throwing program may be initiated. Total course of treatment and return to full play typically takes approximately 3 months but may take longer.
Prevention
Shoulder overuse injuries in young athletes have been identified as common but largely preventable issues. Risk factors for development of overuse injuries include pitching with arm fatigue, higher volumes of pitching, pitching consecutive days, and pitching through pain.
A study of 9- to 14-year-old male baseball players identified that taller players and those with faster pitching velocities are at a higher risk of development of pain.4
Recommendations regarding maximum pitch counts as well as appropriate length of rest depending on age of the pitcher have been established by USA Baseball and should be followed to decrease risk of overuse injuries.5 Avoidance of high-velocity (fastballs) and breaking balls (curveballs or sliders) has been recommended until an athlete is skeletally mature (aged ~14 years). Throwing mechanics should be reviewed by a pitching coach. Resting from overhead sport for at least 4 months of the year is also recommended. Youth athletes and families should be educated to not ignore or try to play through upper extremity pain but instead should rest and be evaluated promptly.
A survey looking at healthy youth baseball players identified that there are psychosocial effects of arm pain that include decreased enjoyment of playing, and that players felt encouraged to keep playing despite arm pain.1
References:
1. Makhni EC, Morrow ZS, Luchetti TJ, et al. Arm pain in youth baseball players: a survey of healthy players. Am J Sports Med. 2015;43(1):41-46.
2. Aoyama JT, Maier P, Servaes S, et al. MR imaging of the shoulder in youth baseball players: anatomy, pathophysiology, and treatment. Clin Imaging. 2019;57:99-109.
3. Pennock AT, Dwek J, Levy E, et al. Shoulder MRI abnormalities in asymptomatic Little League baseball players. Orthop J Sports Med. 2018;6(2):2325967118756825.
4. Greenberg EM, Lawrence JTR, Fernandez-Fernandez A, et al. Physical and functional differences in youth baseball players with and without throwing-related pain. Orthop J Sports Med. 2017;5(11):2325967117737731.
5. USA Baseball. Pitch Smart. Available at; https://www.mlb.com/pitch-smart/. Accessed March 17, 2020.

Low vitamin D levels associated with slowed fracture healing
September 29th 2024“Getting outside and enjoying the fresh air can do wonders for your health while also upping Vitamin D absorption, said Jessica McQuerry, MD, lead study author of an abstract presented at the 2024 AAP National Conference & Exhibition.