3 steps to boost health literacy
What do patients and their families really understand about their healthcare and what can pediatricians do about it?
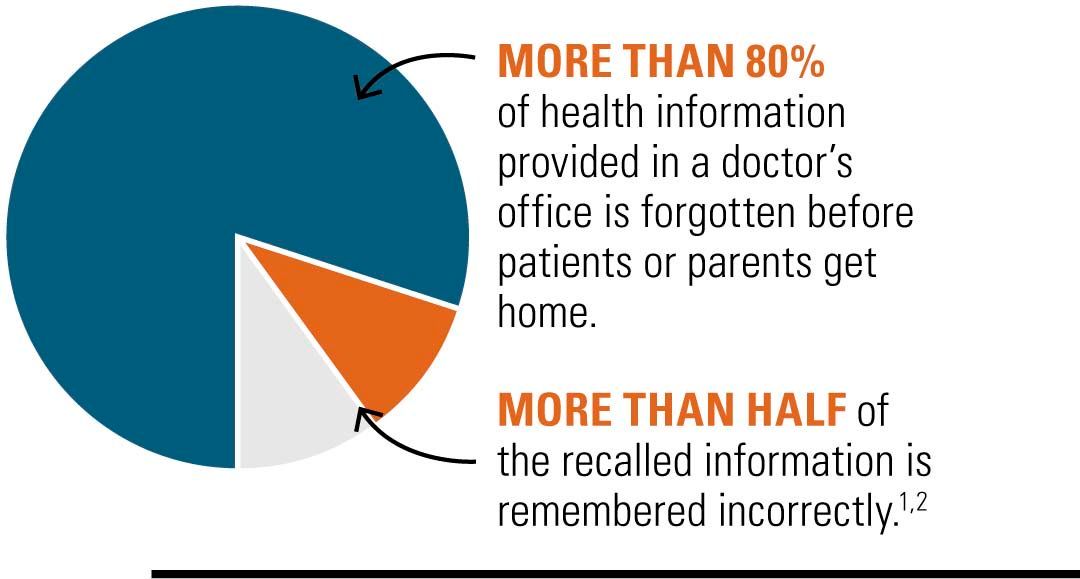
More than 80% of health information provided in a doctor’s office is forgotten before patients or parents get home. More than half of the recalled information is remembered incorrectly.1,2
While fully aware of the role of health literacy-related problems in patient care and the importance of good communication skills, pediatricians often struggle with and underutilize specific techniques to improve communication.3 Pediatricians should be aware of what health literacy is, how it might impact their practice, and steps they can take to improve health literacy in patients and their families.
What is health literacy?
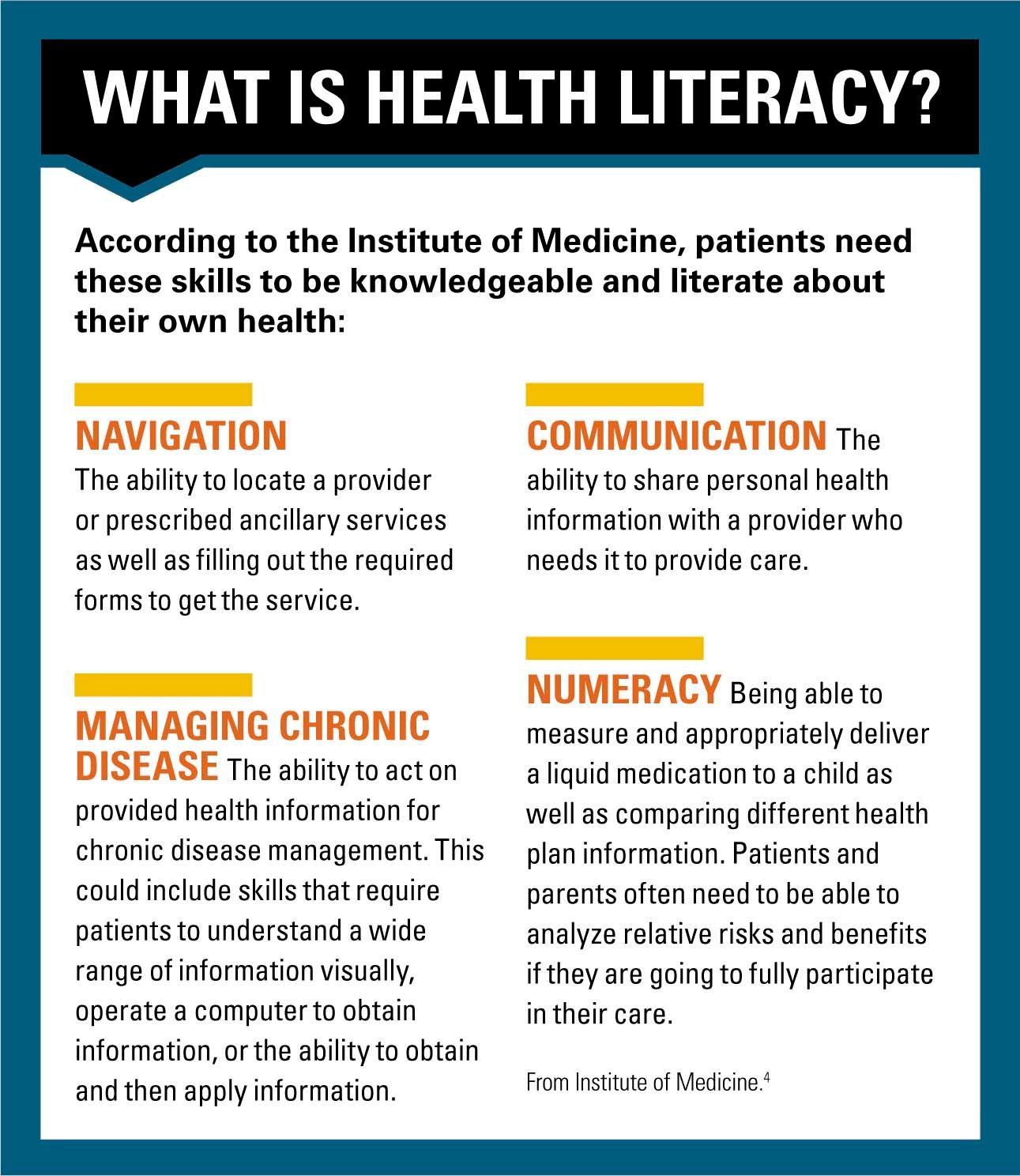
In Health Literacy: A Prescription to End Confusion, the Institute of Medicine defines health literacy as ‘‘the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.”4 Just because a person is able to function at home or work does not mean that they will have adequate literacy in the healthcare setting.
More: Health home meets foster care's complex needs
Health literacy is complex and encompasses a number of skills and abilities for patients to be successful. This can be challenging as it includes several different tasks, such as:4
· Navigation: The ability to locate a provider or prescribed ancillary services as well as filling out the required forms to get the service.
· Communication: The ability to share personal health information with a provider who needs it to provide care.
· Managing chronic disease: The ability to act on provided health information for chronic disease management. This could include skills that require patients to understand a wide range of information visually, operate a computer to obtain information, or the ability to obtain and then apply information.
· Numeracy: Being able to measure and appropriately deliver a liquid medication to a child as well as comparing different health plan information. Patients and parents often need to be able to analyze relative risks and benefits if they are going to fully participate in their care.
Although the pediatrician may not be able to address a number of the societal issues and causes of poor health literacy in his or her own practice, the pediatrician can ensure the practice is health-literacy friendly so that patients and parents can fully engage in care that is needed.
How health literacy impacts patients
Patients with poor health literacy are less likely to participate in preventive care activities such as flu shots.5,6 Low health-literate patients are less knowledgeable about their chronic disease7 and are less able to effectively manage a number of chronic diseases such as high blood pressure, chronic renal disease, diabetes, and asthma.8-11 Low health literacy of parents is also associated with a number of poor health outcomes in pediatrics such as poor asthma12,13 and diabetes control,14 increased use of emergency departments (EDs), incorrect dispensing of medication,15 and decreased rates of breastfeeding.16 In the United States, the economic impact of poor health literacy exceeds $100 billion annually.
Addressing literacy makes a difference
Sometimes pediatricians believe that the societal issues leading to poor health literacy are not really amenable to interventions in a medical practice. Several examples, however, point out that significant differences actually can be made and care can be improved.
NEXT: What can you do in your practice?
Herman and Jackson17 used Head Start sites to evaluate use of a low literacy health book that taught parents how to respond to common childhood illnesses and symptoms. The training lasted approximately 2 hours. The book covers 50 common pediatric problems and symptoms such as fever, pink eye, nose bleeds, and earaches.
Each family’s doctor and ED visits were tracked for 3 months before training and for 6 months following training. Following the intervention, there was a 40% decrease in clinic visits corresponding to 1.5 fewer visits per year. There was a 58% decrease in ED visits corresponding to a decrease of 0.5 visits per year. These improvements translated to a 29% decrease in missed school days and a 42% decrease in missed workdays by caregivers.17
Yin and colleagues18 examined the impact of health literacy on the manner in which dosing instructions were delivered to caregivers as well as the instruments used. The study looked at the dose accuracy measured by caregivers using dosing cups, droppers, dosing spoons, and oral syringes. Overall dosing cups had significantly more dosing errors compared with the other administration instruments, and patients with poor health literacy had significantly more dosing errors across all dosing instruments. Patients with poor health literacy had significantly more problems with the dosing cups, indicating that greater health literacy is needed when dispensing medication with dosing cups. In a follow-up study, Yin found that counseling and provision of a dosing instrument in the ED significantly reduced dosing errors for children being prescribed liquid medication.19
Recommended: Improving the patient visit
Given the recent issues and national concern related to overdoses with pediatric cough and cold medicines, the pediatrician may want to consider education for parents to use an alternative dosing instrument because most cough and cold medications come packaged with a cup.
Finally, although oral instructions are the most common education given to caregivers for administration of medication, few studies have examined alternative strategies and their impact on dosing errors. The HELPix intervention (Health Education and Literacy for Parents [HELP] Project from New York University School of Medicine/Bellevue Hospital Center, New York) uses plain language, pictogram-based medication instruction sheets to assist with adherence and correct dosing.20The instruction sheets are used as part of medication counseling and include a process referred to as “teach back,” wherein patients are asked to demonstrate what they will do to the healthcare provider performing the counseling. The intervention takes 1.5 to 3 minutes depending on how complicated the dosing regimen is. Whereas health literacy was not measured as part of this study, this ED primarily serves at-risk families of low socioeconomic status and low educational attainment, both of which are risk factors for poor health literacy. The pictogram-based, plain-language intervention led to a 42% absolute risk reduction in dosing errors, requiring a number needed to treat of 2 to prevent 1 dosing error.20 Adherence and knowledge were also significantly greater among the intervention group.
What you can do in your practice
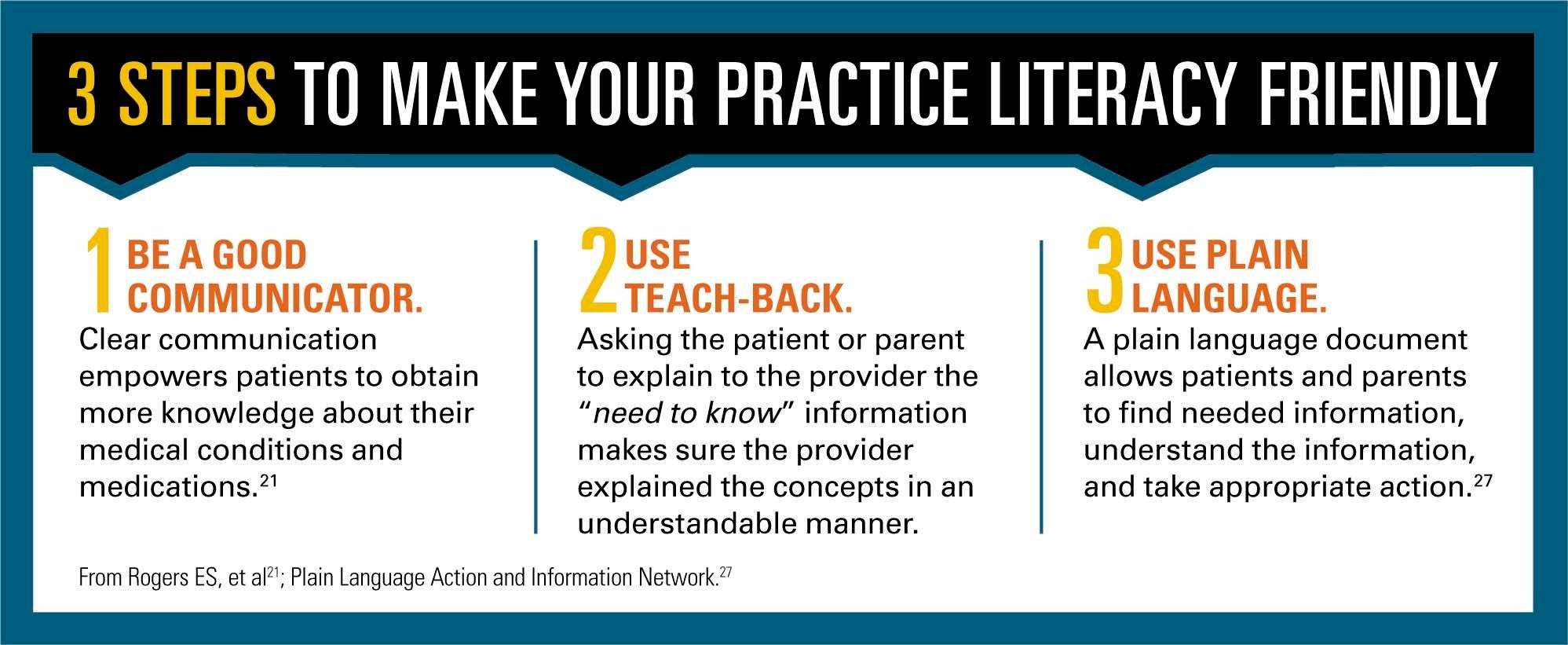
Given the demand and time constraints of practice, pediatricians may wonder if research findings or other health-literacy interventions can be implemented efficiently into their practice. Here are several things you can do to make your practice more health-literacy friendly:
1. Be a good communicator. Clear oral communication is essential for optimal care as physicians are unlikely to be able to predict which patients or parents will have problems understanding medical information.21 The helpful Ask Me 3 communication tool specifies that patients minimally need to be able to answer 3 questions related to their medical problems or goals.22These key questions are:
1. What is the main problem?
2. What actions does the patient or parent need to take?
3. Why are the actions important?
Answers to these 3 questions provide the pediatrician with an assessment of their patient’s understanding of what was communicated to them about a problem. The Ask Me 3 program (created by the Partnership for Clear Health Communication, National Patient Safety Foundation, North Adams, Massachusetts) empowers patients to obtain more knowledge about their medical conditions and medications.
2. Use teach-back. Asking the patient or parent to explain to the provider the “need to know” information makes sure the provider explained the concepts in an understandable manner. For example, a pediatrician could ask a parent, “If you had to explain to your spouse/babysitter/grandparent how to give this antibiotic, what would you say?” Providing patients/parents/caregivers with education in the teach-back format is associated with decreased postoperative infection rates, improved parental assessment of communication, improved outcomes in chronic disease, and improved understanding of medication dosing and discharge instructions.11,23-26
NEXT: Using plain language to communicate
3. Use plain language. Something can be said to be written in plain language when information is understood the first time it is read or heard. A plain language document allows patients and parents to find needed information, understand the information, and take appropriate action.27
When developing or evaluating materials for patients and parents in your practice, you will want to ask yourself several questions:28
· Who is my audience?
· What is my purpose?
· What is my message?
· How urgent is my message?
· What is the “need to know and do”?
Key components for materials include:29,30
· Placing the most important points first.
· Chunking information or breaking complex topics into understandable chunks.
· Using simple, living-room language rather than technical language.
· Making sure your document answers questions that your parents and patients have about a particular topic.
· If you need to use technical language, make sure to provide a definition.
· Using the active voice. Active voice makes it clear who needs to take action.
· Writing in the first or second person when possible.
· Shorter is better. Not just total length, but paragraphs of 5 sentences with each sentence containing 10 to 20 words is optimal.
· If you can use a picture, table, or illustration instead of a paragraph, that is optimal.
· Using easy-to-read fonts and having plenty of white space.
· Making your document skimmable by using headings and numbered or bulleted lists.
Summary
Health literacy cannot be seen, but the pediatrician should assume patients and parents in his or her practice have issues with health literacy. Small changes in communication, developing materials, and addressing how patients are instructed to take medications can make the difference in whether or not patients follow instructions and take their medication correctly. In addition, the pediatrician should consider advocacy to promote health literacy in his or her hospital and community.
Next: Office preparedness for childhood for emergencies
REFERENCES
1. Anderson JL, Dodman S, Kopelman M, Fleming A. Patient information recall in a rheumatology clinic. Rheumatol Rehabil. 1979;18(1):18-22.
2. Kessels RP. Patients' memory for medical information. J R Soc Med. 2003;96(5):219-222.
3. Turner T, Cull WL, Bayldon B, et al. Pediatricians and health literacy: descriptive results from a national survey. Pediatrics. 2009;124 suppl 3:S299-S305.
4. Institute of Medicine (US) Committee on Health Literacy; Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press; 2004.
5. Scott TL, Gazmararian JA, Williams MV, Baker DW. Health literacy and preventive health care use among Medicare enrollees in a managed care organization. Med Care. 2002;40(5):395-404.
6. MacLeod S, Musich S, Gulyas S, et al. The impact of inadequate health literacy on patient satisfaction, healthcare utilization, and expenditures among older adults. Geriatr Nurs. 2017;38(4):334-341.
7. Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51(3):267-275.
8. Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self-care. Chest. 1998;114(4):1008-1015.
9. Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158(2):166-172.
10. Lai AY, Ishikawa H, Kiuchi T, Mooppil N, Griva K. Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemodialysis. Patient Educ Couns. 2013;91(2):221-227.
11. Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83-90.
12. DeWalt DA, Dilling MH, Rosenthal MS, Pignone MP. Low parental literacy is associated with worse asthma care measures in children. Ambul Pediatr. 2007;7(1):25-31.
13. Harrington KF, Zhang B, Magruder T, Bailey WC, Gerald LB. The impact of parent's health literacy on pediatric asthma outcomes. Pediatr Allergy Immunol Pulmonol. 2015;28(1):20-26.
14. Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with Type 1 diabetes. Diabet Med. 2001;18(5):364-369.
15. Yin HS, Dreyer BP, Foltin G, van Schaick L, Mendelsohn AL. Association of low caregiver health literacy with reported use of nonstandardized dosing instruments and lack of knowledge of weight-based dosing. Ambul Pediatr. 2007;7(4):292-298.
16. DeWalt DA, Hink A. Health literacy and child health outcomes: a systematic review of the literature. Pediatrics. 2009;124 suppl 3:S265-S274.
17. Herman A, Jackson P. Empowering low-income parents with skills to reduce excess pediatric emergency room and clinic visits through a tailored low literacy training intervention. J Health Commun. 2010;15(8):895-910.
18. Yin HS, Mendelsohn AL, Wolf MS, et al. Parents' medication administration errors: role of dosing instruments and health literacy. Arch Pediatr Adolesc Med. 2010;164(2):181-186.
19. Yin HS, Dreyer BP, Moreira HA, et al. Liquid medication dosing errors in children: role of provider counseling strategies. Acad Pediatr. 2014;14(3):262-270.
20. Yin HS, Dreyer BP, van Schaick L, Foltin GL, Dinglas C, Mendelsohn AL. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adolesc Med. 2008;162(9):814-822.
21. Rogers ES, Wallace LS, Weiss BD. Misperceptions of medical understanding in low-literacy patients: implications for cancer prevention. Cancer Control. 2006;13(3):225-229.
22. Graham S, Brookey J. Do patients understand? Perm J. 2008;12(3):67-69.
23. Kornburger C, Gibson C, Sadowski S, Maletta K, Klingbeil C. Using “teach-back” to promote a safe transition from hospital to home: an evidence-based approach to improving the discharge process. J Pediatr Nurs. 2013;28(3):282-291.
24. Badaczewski A, Bauman LJ, Blank AE, et al. Relationship between Teach-back and patient-centered communication in primary care pediatric encounters. Patient Educ Couns. 2017;100(7):1345-1352.
25. Mallory LA, Diminick NP, Bourque JP, et al. Pediatric patient-centered transitions from hospital to home: improving the discharge medication process. Hosp Pediatr. 2017;7(12):723-730.
26. Gould JM, Hennessey P, Kiernan A, Safier S, Herman M. A novel prevention bundle to reduce surgical site infections in pediatric spinal fusion patients. Infect Control Hosp Epidemiol. 2016;37(5):527-534.
27. Plain Language Action and Information Network. What is plain language? Available at: https://www.plainlanguage.gov/about/definitions/. Accessed December 11, 2017.
28. National Institutes of Health. Plain language: Before you start writing. Available at: https://www.nih.gov/institutes-nih/nih-office-director/office-communications-public-liaison/clear-communication/plain-language/before-you-start-writing. Published March 27, 2017. Accessed December 11, 2017.
29. Doak CC, Doak LG, Root JH. Teaching Patients with Low Literacy Skills. 2nd ed. Philadelphia, PA: J.B. Lippincott Co.; 1996.
30. Doak CC, Doak LG, Friedell GH, Meade CD. Improving comprehension for cancer patients with low literacy skills: strategies for clinicians. CA Cancer J Clin. 1998;48(3):151-162.
Anger hurts your team’s performance and health, and yours too
October 25th 2024Anger in health care affects both patients and professionals with rising violence and negative health outcomes, but understanding its triggers and applying de-escalation techniques can help manage this pervasive issue.