The adolescent with a painful scrotum
A painful or swollen scrotum is a potential emergency. Be sure you know how to distinguish testicular torsion from less urgent problems.
The adolescent with a painful scrotum
By William P. Adelman, MD, and Alain Joffe, MD, MPH
A painful or swollen scrotum is a potential emergency. Be sure you know how to distinguish testicular torsion from less urgent problems.
The painful or acutely swollen scrotum requires accurate and timely assessment. An adolescent with these symptoms should be examined promptly and thoroughly, looking particularly for the signs of torsion and epididymitis reviewed here. This article is a companion piece to our overview of the male genital examination, which appeared in Contemporary Pediatrics last July.
Who gets what?
Case studies of patients with acute scrotal pain indicate varying etiologies for the condition. A review of the charts of 387 inpatients with acute scrotal pain showed that in all children under 6 years old the problem was testicular torsion, as it was in half the patients 7 to 12 years of age. The remaining cases were caused by torsion of an intrascrotal appendage. In 13- to 18-year-old patients, 76% had testicular torsion, 16% had torsive appendages, and 8% had epididymitis. In 80% of 19- to 24-year-olds, the cause of pain was epididymitis.
In another review of multiple surgical admissions and hospital patients, testicular torsion accounted for acute scrotal pain in approximately 42% of children. This review combined 211 cases from four different case series. Patients ranged in age from 2 to 18 years. Other diagnoses were torsion of an appendage in 29%, epididymitis in 22%, and orchitis in 3%.1 A more recent study looked at 238 patientsinfants, children, and adolescents up to 19 years oldwho came to the emergency room in a children's hospital. Sixteen percent of boys had testicular torsion, 35% epididymitis, and 46% torsion of an intrascrotal appendage.2
Testicular torsion
Testicular torsion is a twisting of the testis and spermatic cord that results in venous obstruction, progressive edema, arterial compromise, and, eventually, testicular infarction. It is a surgical emergency: A delay in diagnosis of only four to six hours may result in abnormal testicular function, and a delay of more than six hours often leads to removal of the testicle. Testicular torsion is the most common cause of testicular loss in young males. The risk of developing torsion by age 25 is estimated to be about one in 160.3
There are two types of torsion, defined by their relationship to the tunica vaginalis: extravaginal and intravaginal. Extravaginal torsion occurs primarily in neonates or occasionally in utero and accounts for less than 10% of all cases of torsion. It occurs when the gubernaculum and testicular tunics are not completely attached to the scrotal wall and involves a complete twisting of the scrotal contents (testis, epididymis, and tunica vaginalis) on the spermatic cord. Extravaginal torsion usually causes little distress, and the testicular salvage rate is poor. Intravaginal torsion, twisting of the testis within the tunica vaginalis, accounts for 90% of all cases of torsion and nearly all cases in children older than 2 years. While it may happen at any age, two thirds of cases occur in boys between 12 and 18 years, with incidence peaking at 15 to 16 years.
The "bell-clapper" deformity (Figure 1) refers to the anatomical appearance of the testis within an abnormally enlarged and engulfing tunica vaginalis. This deformity. which is congenital and predisposes to torsion, looks like a clapper in a bell. It generally occurs bilaterally when the tunica vaginalis attaches higher on the spermatic cord than usual.
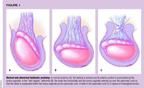
The testis may rotate within the enlarged tunica vaginalis, obstructing both venous outflow and arterial inflow and resulting in ischemia.4 Bell clapper deformity is often associated with horizontal orientation ("horizontal lie" or "transverse lie") of the testicle. This causes the testicle to be more mobile than a normal testicle, and more susceptible to torsion.5
History and physical exam. Characteristically, the history for testicular torsion begins with the sudden onset of pain and swelling in one testicle, often while the young man is sleeping or otherwise inactive. Occasionally the problem is associated with minor trauma, strenuous exercise, or sexual activity. The onset of pain is more gradual in up to one quarter of cases. One third to one half of patients mention previous episodes of similar pain, probably a sign of torsion that resolved spontaneously. Pain may be referred to the abdomen, back, flank, groin, or thigh, so all boys with pain in these areas deserve a careful genital examination. Nausea and vomiting often occur. If testicular torsion is suspected, a urologist should be consulted immediately.3,4
Examination of a standing patient usually reveals an elevated, tender testis on the side of the torsion. When the testicle twists on itself, it shortens the vascular pedicle from which the testicle hangs. This results in the elevation of the testicle in the scrotum. In some cases, the testis appears to be horizontal. Early in torsion, the epididymis may be felt anteriorly and high in the scrotum. If presentation is delayed, the entire gonad may become so swollen that the epididymis cannot be distinguished from the testis on palpation.5 If presentation is early, transillumination of the scrotum will not work. If a reactive hydrocele develops later, partial transillumination of the scrotum is possible. Clearly, transillumination is not very useful when managing painful scrotal conditions. Examination of the contralateral testis is usually necessary to determine relative position, lie, and feel of affected testis.
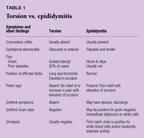
Differentiating torsion from epididymitis. Testicular torsion is often difficult to differentiate from epididymitis (Table 1). Alleviation of testicular pain by elevating the testis above the pubic symphysis (Prehn sign) suggests epididymitis. Failure to lessen pain with elevation of the testis suggests torsion. We hypothesize that since ischemia causes the pain from torsion, elevation of the testicle would not be expected to alleviate it. This test is not completely reliable, however, especially if torsion is of long duration.
An absent cremasteric reflex is the most sensitive physical finding for diagnosing testicular torsion.6 The cremaster muscle reflexively draws the testis upward within the scrotum. Contraction of the cremaster muscle can be produced by lightly scratching the skin in the area served by the ilioinguinal nerve, which is the medial aspect of the upper thigh (Figure 2). This results in reflex retraction of the ipsilateral testicle. The cremasteric reflex is much more active in children and adolescents than in adults. In the case of intravaginal testicular torsion, the cremaster muscle cannot contract effectively, so patients with a tender testicle and an absent cremasteric reflex are much more likely to have testicular torsion than epididymitis or torsion of the appendix testis. Conversely, the presence of a cremasteric reflex almost always allows the physician to rule out testicular torsion.

Urinary symptoms are uncommon in testicular torsion. Only 6% of patients with testicular torsion have irritative voiding symptoms, and only 7% have significant pyuria.6
Signs and symptoms such as low-grade fever, elevated white blood cell count, Prehn sign, a previous history of pain, elevation of the testicle, and abnormal lie of the testicles may be present in 21% to 50% of torsion cases.1 No single sign or symptom is sufficiently sensitive or specific to confirm or exclude the diagnosis of testicular torsion.
Other entities in the differential. Besides epididymitis, the differential diagnosis of testicular torsion includes torsion of intrascrotal appendages such as the appendix testis or appendix epididymis. Other less common entities that may be confused with torsion include:
- acute hemorrhage into a testicular neoplasm
- epididymo-orchitis, which results from mumps or other viral illness
- testicular abscess
- incarcerated scrotal hernia
- traumatic hydrocele, or trauma that causes testicular rupture (hematocele)
- testicular torsion following a history of orchidopexy.7
Laboratory tests and imaging studies. If a reasonable suspicion of torsion exists, the primary therapy should be surgical exploration, without a delay to order diagnostic tests. On the other hand, if torsion appears less likely than another diagnosis such as epididymitis but cannot be excluded, a testicular scan or Doppler flow study is helpful. To ensure a timely evaluation, it is imperative to involve a urologist in the care of the patient from the time of presentation. Many pediatricians practice in places where immediate evaluation by a urologist is not possible. In such a situation, the pediatrician needs to know what additional testing is available and whether the urology consultant would prefer the pediatrician to order tests immediately or wait for the consultant. Of course, if immediate radiologic support is also not available, evaluation in the operating room is the best course of action.
Scintigraphy for diagnosis of testicular torsion has a sensitivity of 80% to 100% and a specificity of 89% to 100%.8 It is most helpful in the first few hours, before reactive hyperemia of scrotal skin takes place. It may show decreased or absent testicular blood flow consistent with an ischemic testis. With inflammatory disorders such as epididymitis and orchitis, increased blood flow and blood pool activity are seen. A halo sign (a rim of increased perfusion around the avascular testis) appears on scintigraphy if complete torsion is not treated and becomes chronic.9
Color Doppler ultrasonography has a sensitivity of 80% to 100%, a specificity of 90% to 100%, and an accuracy of 97% to 100% when used as an adjunctive tool in the diagnosis of torsion to assess the perfusion of the testis.4,6,10,11 As these studies are not 100% sensitive and specific, a negative study should not preclude emergency operative exploration of a clinically suspicious lesion.12
Treatment. Surgical exploration remains the best diagnostic tool and is necessary to salvage the testis. During the follow-up appointment, the presence of a normal testicle on palpation indicates successful salvage. Whether the testicle can be saved depends on the amount of time between onset of symptoms and surgical exploration.13 Patients operated on within three hours have a near 100% salvage rate. After six hours, the salvage rate drops to 92%. It is 62% at six to 12 hours, 38% at 12 to 24 hours, and 11% at 24 to 48 hours. Surgical orchidopexy is required to prevent recurrence. If an infarcted testicle is discovered during surgical exploration, it is removed. Exploration of the contralateral side is standard, since the anomaly of the tunic is encountered in more than 50% of contralateral testicles. Five percent to 30% of contralateral testes that do not undergo surgical fixation will subsequently develop torsion.1
Torsion of the appendages
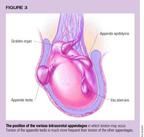
As shown in Figure 3, there are four intrascrotal appendages (appendix testis, appendix epididymis, vas aberrans, and Giraldes organ) but only the appendix testis and epididymis are significantly prone to torsion. In contrast to testicular torsion, torsion of the appendix testis or appendix epididymis has a good prognosis and rarely results in significant sequelae. Anatomic studies reveal an appendix testis in 92% of testicles. This structure, a remnant of the müllerian duct located on the upper pole of the testis or in the cleft between the testis and the epididymis, accounts for 90% of torsive appendages. In contrast, the appendix epididymis is encountered in 34% of anatomic studies but is responsible for only 7% of torsive appendages. It is a remnant of the wolffian duct and is located at the head of the epididymis. The incidence of torsion of an appendage peaks between 10 and 14 years of age. The right and left sides are affected equally often.1
Most commonly, a young adolescent presents with subacute scrotal pain, describing its onset as either abrupt or gradual. The pain is usually much less intense than that of testicular torsion. Early in the natural history, pain is localized in the area of the torsion and a small, tender mass can be palpated. The examiner may see a "blue dot," representing a gangrenous appendix; it is most evident when the scrotal skin is stretched taut, or with transillumination. As the torsion progresses, most patients develop a reactive hydrocele and significant edema and erythema, making the examination difficult. White blood cell count and urinalysis are unremarkable. Further studies are rarely required.
A urologist should be consulted promptly but the affected appendage can often be left alone to autoamputate. Treatment with analgesics and bed rest are recommended, and pain usually subsides in a few days. Some urologists advocate surgical removal.
Epididymitis
Epididymitis is an inflammation of the epididymis caused by infection or trauma; it is primarily a problem of sexually active adolescents. Epididymitis is uncommon before puberty,14 and, when present, is often associated with underlying genitourinary anomalies.15 The urethritis that precedes epididymitis may be asymptomatic. Among males younger than 35, epididymitis is most often caused by Chlamydia trachomatis or Neisseria gonorrhoeae. Escherichia coli is a causative agent among men who engage in insertive anal intercourse.16 An adolescent who is not sexually active may develop epididymitis from trauma or an underlying genitourinary anomaly.
In a typical case, a sexually active young man reports subacute pain in the hemiscrotum, inguinal area, or abdomen. Approximately two thirds of individuals see a physician after 24 hours of painlater than those who have testicular torsion.3 Some patients have a history of dysuria or urethral discharge, but the symptoms may be so mild that they go unnoticed or unmentioned. On physical examination, the typical patient has unilateral testicular pain and tenderness. In an early stage, only the epididymis is tender, swollen, and thickened. Later, swelling of the scrotum, testis and spermatic cord or a reactive hydrocele may obscure the diagnosis. The scrotal skin becomes erythematous and edematous. A minority of patients are febrile, but fever is more often present in epididymitis than in torsion. A patient may have dysuria and a urethral discharge, but the absence of these signs does not rule out the diagnosis. The affected testis is lower than the other testis, and its lie is normal. Elevation of the testicle may relieve pain. The cremasteric reflex is usually present. If the swollen epididymis cannot be clearly differentiated from the testicle, or if reactive edema and inflammation make the examination difficult, immediate urologic consultation and evaluation to rule out testicular torsion is mandated.
A patient's first-void urine (first 15 mL) should be examined for leukocytes. A culture and Gram stain of urine that has not been centrifuged may be helpful in identifying the cause of the infection, and Gram stain of urethral exudate or an intraurethral swab is recommended for diagnosis of urethritis. A presumptive diagnosis of gonococcal infection can be made if the Gram stain shows gram-negative intracellular diplococci. A culture of urethral exudate or the urethral swab specimen, or nucleic acid amplification testing of the swab material or urine, should be performed for C trachomatis and N gonorrhoeae. As epididymitis is a sexually transmitted disease, syphilis serology and HIV counseling and testing are also recommended.16
Empiric therapy is indicated in all cases of epididymitis. The Centers for Disease Control and Prevention guidelines recommend a single intramuscular injection of 250 mg of ceftriaxone plus 100 mg of doxycycline orally twice a day for 10 days. If epididymitis caused by enteric organisms is suspected, or if the patient is allergic to cephalosporins or tetracyclines, 300 mg of ofloxacin orally twice a day for 10 days is the recommended regimen.16 In severe cases, or with unreliable follow-up, hospitalization may be required.
Supportive care includes bed rest, nonsteroidal anti-inflammatory medications, scrotal support, and ice packs. Patients should be instructed to refer all sex partners from the prior 60 days for evaluation and treatment. Further sexual intercourse should be avoided until they and their sex partners have completed therapy and no longer have symptoms.16
Patients should begin to improve within 24 to 48 hours after starting therapy. Failure to improve within two days requires reevaluation of both the diagnosis and therapy. A urology consultation should be considered for further evaluation of a possible abscess, infarction, or testicular cancer. Tuberculosis or fungi are also rare infectious causes of epididymitis.
Epididymo-orchitis
Orchitis, or inflammation of the testicle, is rare among individuals who have received MMR vaccine and rarely affects only the testicle. As the epididymis is also affected, epididymo-orchitis is a more accurate term. Many viruses and bacteria can cause orchitis. Mumps is the most common infectious cause in adolescents. Up to 40% of postpubertal males infected with the mumps virus develop orchitis.17 Approximately 40% of all mumps orchitis cases occur in teenagers. Mumps orchitis remains a problem in the United States among underimmunized adolescents, and this diagnosis should be considered in any adolescent with testicular pain who has not received two doses of the MMR vaccine. Its incidence is highest in young men 15 to 29 years old.
Symptoms usually develop gradually, sometimes during or preceding a case of mumps. If orchitis follows parotitis, it usually does so four to eight days later. Vague systemic complaints such as malaise, myalgias, and headache followed by fever are often present. Typically patients have a fever at the end of the first week of illness, followed by testicular pain, swelling, and tenderness. When taking a history, it's important to ask if any other family members have been diagnosed with mumps recently.
On examination, one or both testicles and occasionally the epididymis are enlarged, indurated, and tender. Sixty-two percent to 83% of cases are unilateral. The patient's scrotal skin may become erythematous and edematous, and a reactive hydrocele may develop. The patient may find some relief from elevation of the testis.
The diagnosis of mumps can be confirmed serologically or by isolation of the virus in cell culture inoculated with throat washings, urine, or cerebrospinal fluid. Unfortunately, these tests are not very helpful during initial management, since getting the results takes time. While acute and convalescent titers are desirable, a single serum specimen containing complement-fixing antibody against the soluble component of mumps virus suggests recent infection.18 Skin testing with mumps antigen is unreliable. The white blood cell count may be mildly elevated and urinalysis may reveal pyuria. If parotitis is present, amylase levels may be elevated. Doppler flow studies of the scrotum reveal increased blood flow, which may help differentiate orchitis from torsion.
Symptomatic treatment is indicated. This may include nonsteroidal anti-inflammatory drugs, rest, ice packs, and scrotal support for the pain. Symptoms usually resolve within 10 days. Infection control measures should be instituted until the swelling subsides, as mumps can be contagious for as long as nine days after the onset of disease.
As part of infection control, children should stay home from school for nine days from the onset of parotid gland swelling. Mumps is spread by direct contact with respiratory secretions, so the patient should take "droplet precautions." Those who have not been exposed to the disease should be kept away from the sick patient so that he does not sneeze or cough on them. In addition, the patient and everyone who comes in contact with him should wash their hands thoroughly and frequently.
Thirty percent to 50% of affected testes have some atrophy, and impaired fertility is thought to occur in up to 10% of men. Since the majority of males remain fertile, it is important to counsel adolescent boys about the continued need for sexually responsible behavior. The incidence of malignancy in atrophied testes is not significantly increased.
The high rate of atrophy following mumps orchitis reinforces the need to prevent this illness. Any adolescent without a documented history of mumps or mumps vaccination should receive the live attenuated virus. It is estimated that in the US, 10% to 20% of adolescents over 15 years of age may still be susceptible to mumps.17
Summing up
The adolescent male may see a pediatrician with complaints about pain or swelling in the genital region. It is important for the pediatrician to have a thorough understanding of the common manifestations of genital diseases that occur during adolescence and to distinguish the potential surgical emergency from the normal variant or easily treated problem.
REFERENCES
1. Sheldon CA: Undescended testis and testicular torsion. Surg Clin North Am 1985;65(5):1318
2. Lewis AG, Bukowski TP, Jarvis PD, et al: Evaluation of acute scrotum in the emergency department. J Pediatr Surg 1995;30(2):277
3. Klein BL, Ochsenschlager DW: Scrotal masses in children and adolescents: A review for the emergency physician. Pediatr Emerg Care 1993;9:351
4. Jayson MA, Foster HE: Management of urologic emergencies for nonurologists. Resident and Staff Physician 1995;41(6):13
5. Keshava Murthy JH, Hiremagalur SR: Testicular torsion. Hospital Physician 1995;31(Sept):40
6. Kadish HA, Bolte RG: A retrospective review of pediatric patients with epididymitis, testicular torsion, and torsion of testicular appendages. Pediatrics 1998;102:73
7. Shaughnessy MO, Walsh TN, Given HF: Testicular torsion following orchidopexy for undescended testis. Br J Surg 1990;77:583
8. Chen DCP, Holder LE, Kaplan GN: Correlation of radionuclide imaging and diagnostic ultrasound in scrotal diseases. J Nucl Med 1986;27:1774
9. Chen DCP, Holder LE, Melloul M: Radionuclide scrotal imaging: Further experience with 210 patients. J Nucl Med 1983;24:735
10. Dewire DM, Begun FP, Lawson RK, et al: Color Doppler ultrasonography in the evaluation of the acute scrotum. J Urol 1992;147:89
11. Burks DD, Markey BJ, Burkhard TK, et al: Suspected testicular torsion and ischemia: Evaluation with color Doppler US and testicular scintigraphy. Radiology 1990;175:815
12. Stoller ML, Kogan BA, Hricak H: Spermatic cord torsion: Diagnostic limitations. Pediatrics 1985;76:929
13. Cass AS, Cass BP, Veeraraghan K: Immediate exploration of the unilateral acute scrotum in young male subjects. J Urol 1980;124:829
14. Likitnukul S, McCracken GH, Nelson JD, et al: Epididymitis in children and adolescents: A 20-year retrospective study. Am J Dis Child 1987;141:41
15. Siegel A, Snyder H. Duckett JW: Epididymitis in infants and boys: Underlying urogenital anomalies and efficacy of imaging modalities. J Urol 1987;138:1100
16. Centers for Disease Control and Prevention: 1998 Guidelines for treatment of sexually transmitted diseases. MMWR 1998;47(No. RR-1-116):86
17. Hofmann AD, Greydanus DE (eds): Adolescent Medicine, ed 3. Stamford, CT, Appleton & Lange, 1997, p 416
18. American Academy of Pediatrics: Mumps, in Peter G (ed): 1997 Red Book. Report of the Committee on Infectious Diseases, ed 24. Elk Grove Village, IL, American Academy of Pediatrics, 1997, p 366
DR. ADELMAN is a Fellow in Adolescent Medicine, Division of General Pediatrics and Adolescent Medicine, Johns Hopkins Medical Institutions, Baltimore.
DR. JOFFE is Director, Adolescent Medicine, and Associate Professor of Pediatrics, Johns Hopkins Medical Institutions, Baltimore.
William Adelman, Alain Joffe. The adolescent with a painful scrotum.
Contemporary Pediatrics
2000;3:111.