Boy With Multifaceted Acute Illness
A 9-year-old previously healthy boy presents to his pediatrician with acute onset of a nonproductive cough, left eye swelling without loss of visual acuity, persistent fever of 3 days’ duration, chills, headache, chest pain, vomiting, and left knee pain with inability to bear weight.
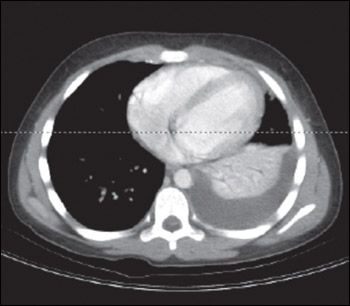
Figure 1 – This patient's chest CT scan showed a left-sided pleural effusion with consolidation. The cause of the pneumonia was invasive group A streptococcal infection.
A 9-year-old previously healthy boy presents to his pediatrician with acute onset of a nonproductive cough, left eye swelling without loss of visual acuity, persistent fever of 3 days' duration, chills, headache, chest pain, vomiting, and left knee pain with inability to bear weight. The child is admitted for further management; infectious disease and ophthalmology specialists are contacted for consultation.
HISTORY
There were multiple ill contacts at the patient's school; these children had a febrile illness whose symptoms-which included rhinorrhea and cough-appeared to be viral in origin. The patient does not have a history of allergies, and there is no travel history. The family history is noncontributory.
PHYSICAL EXAMINATION
The patient is in moderate distress, has a flushed face, and is febrile (temperature 39.3°C [102.7°F]). He has significant tachycardia (heart rate, 109 beats per minute) but stable blood pressure (82/56 mm Hg). Examination of the head, ears, eyes, nose, and throat reveals significant periorbital swelling of the left eyelid with injected nonpurulent conjunctiva but no discharge; intact extraocular movement; dry oropharynx with tacky mucous membranes; and 2+ pink, nonpurulent tonsils. There are no other palatal findings. He does not demonstrate meningism. Cardiopulmonary examination reveals a nonradiating 2/6 systolic murmur at the left upper sternal border, with no rubs or gallops; absent breath sounds throughout the left lung field; and no rales or rhonchi on percussion. A musculoskeletal examination demonstrates significant swelling of the left knee with inability to bear weight. There is no point tenderness. Range of motion in the swollen knee is limited: he can flex it to only 45 degrees, and he can extend it only about 20 degrees from neutral.
LABORATORY AND IMAGING RESULTS
A complete blood cell count reveals a white blood cell count of 21,500/μL, with a left shift (41% neutrophils, 17% band forms, 25% lymphocytes, 3% basophils, and 4% eosinophils). Liver transaminase levels are elevated (aspartate aminotransferase, 217 U/L; alanine aminotransferase, 398 U/L). Titers of anti-DNAse B and anti-streptolysin O (ASO) are markedly positive (ASO level, 1298 UI/mL). Culture of joint fluid obtained via arthrocentesis of the left knee grows group A β-hemolytic streptococci (Streptococcus pyogenes). Chest CT scan reveals a leftsided pleural effusion with consolidation (Figure 1).
Invasive, disseminated group A streptococcal (GAS) infection is diagnosed. Manifestations of the infection include left periorbital cellulitis with associated sinusitis, left-sided pneumonia with a parapneumonic effusion, and septic arthritis of the left knee.
Answer and discussion begin on Next Page
The correct answer is C.
From Hollm-Delgado MG, Allard R, Pilon PA. Invasive group A streptococcal infections, clinical manifestations and their predictors, Montreal, 1995-2001.
Emerg Infect Dis.
2005;11:77-82.
http://www.cdc.gov/ncidod/EID/vol11no01/03-0651.htm
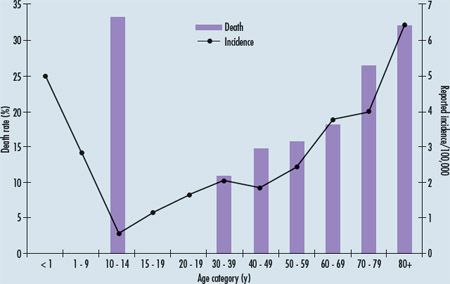
. Accessed July 13, 2010. Figure 2 – This graph shows both the annual incidence of and death rate for invasive group A streptococcal infection (IGASI) by age in Montreal between 1995 and 2001. Note that although the incidence of IGASI is lowest in children between the ages of 10 and 14 years, the death rate from IGASI is highest in that age-group.
The most common manifestations of GAS infection are pharyngitis and simple skin infections. Between 15% and 30% of cases of acute pharyngitis are caused by GAS; the highest incidence is in children aged 5 to 11 years. The incubation period for streptococcal pharyngitis is short (2 to 5 days), and transmission occurs via inhalation of organisms in large droplets or by contact with respiratory secretions. Because GAS pharyngitis is self-limited (typically resolving in 3 to 5 days without therapy), this diagnosis is unlikely in patients in whom symptoms last longer than 4 or 5 days. Scarlet fever, characterized by an erythematous, diffuse, sandpapertextured exanthema, can accompany GAS pharyngitis (as well as other streptococcal illnesses). The rash is concentrated at skin creases (Pastia lines), blanches with pressure, and spares the circumoral region.
However, group A streptococci also cause a wide range of more serious clinical syndromes, including severe suppurative infections; direct complications,a such as retropharyngeal abscesses and streptococcal toxic shock syndrome (TSS); and immune-mediated complications, a such as acute rheumatic fever and acute glomerulonephritis. In invasive GAS infections (IGASI), S pyogenes may be spread via bodily secretions as well as via respiratory droplets.
Practice Pearl 1: Group A streptococci can cause a wide variety of clinical symptoms; these range from simple skin infections and pharyngitis to suppurative infections and even toxic shock syndrome. Poll Results
Online Poll
Powered By
WebsiteGear
: Requires Javascript Enabled On Your Browser.
Typical manifestations of IGASI. A range of clinical identifiers are associated with IGASI, including pneumonia, bacteremia, soft tissue infections, streptococcal TSS, and death. Examples of typical soft tissue infections include fasciitis, myositis, cellulitis (as in this boy), and erysipelas. Bacteremia caused by IGASI is characterized by positive results on hemoculture in the absence of any identifiable source of infection. In pneumonia attributable to IGASI, a typical clinical picture might include streptococcal TSS without respiratory distress.
Risk factors for IGASI. Since the mid-1980s, concern has grown that IGASI has been increasing in severity and incidence. In particular, the emergence of streptococcal TSS has demonstrated the increasing severity of GAS infections. Infection with the M serotypes of S pyogenes (in particular, M1, M3, and M18) is more likely to result in severe disease. Other risk factors for IGASI include very young or very old age (Figure 2) and underlying medical conditions (including exposure to varicella).
Mortality in IGASI. According to the CDC, the mortality from IGASI is close to 15%; mortality is highest among patients aged 10 to 14 years and those older than 70 years (see Figure 2). The highest mortality rates, based on clinical manifestation, are seen in patients with pneumonia (almost 40%), followed by those with streptococcal TSS (35%), patients with bacteremia (20%), and those with soft tissue infections (10%). Of all the soft tissue IGASIs, necrotizing fasciitis is associated with the highest risk of death in all age groups.
Practice Pearl 2: Invasive group A streptococcal infections have been increasing in incidence and severity, as evidenced by the emergence of streptococcal shock.
Diagnosis of streptococcal infection. Throat culture has long been the gold standard for the diagnosis of GAS pharyngitis. It has a 90% to 95% sensitivity for identifying GAS in the nasopharynx. Diagnosis has improved with the development of rapid antigen detection systems that can identify GAS. Standard rapid antigen tests have very high specificity (95% to 98%); however, their sensitivity varies from 70% to 90%. Serological testing for GAS pharyngitis generally is not useful in the diagnosis of acute infection because antistreptococcal antibodies increase only weeks after infection. Antibodies against streptolysin O, DNAse B, hyaluronidase, and streptokinase are used to confirm a recent-but not a current-GAS infection.
Keep in mind that accurate detection and treatment of GAS pharyngitis is needed to prevent acute rheumatic fever. All the same, unnecessary testing can result in misdiagnosis in chronic GAS carriers who are presenting with an intercurrent viral illness.
Practice Pearl 3: When diagnosing group A streptococcal infection, standard rapid antigen tests have very high specificity but variable sensitivity; throat culture remains the gold standard. Serological testing is not useful in detecting current infection but can help confirm recent infection.
Management of IGASI. GAS remains universally sensitive to penicillin, and this agent is the first-line therapy once the causative organism has been identified and susceptibilities have been isolated. In patients who are allergic to penicillin, the drug of choice is erythromycin (or another macrolide). In patients with deep oropharyngeal abscesses, consider using ampicillin/sulbactam instead of penicillin to cover anaerobes and deep oropharyngeal flora. Antibiotic therapy for streptococcal TSS includes penicillin and clindamycin, along with intravenous immunoglobulin to neutralize toxins and ameliorate disease severity.
Practice Pearl 4: Group A streptococcal infections remain universally sensitive to penicillin, which is the first-line therapy.
Outcome of this case. The patient's GAS pharyngitis resulted in sinusitis, which led, in turn, to the development of orbital cellulitis. His pneumonia was also a complication of the pharyngitis. Hematogenous spread was responsible for the septic arthritis in his left knee.
The patient's orbital cellulitis resolved with antibiotic therapy. However, serial chest radiographs confirmed a worsening pneumonia and parapneumonic effusion, which eventually required surgical intervention and chest tube drainage. He initially received supplemental oxygen but was weaned to room air quickly.
Imaging studies of his left knee showed soft tissue swelling and an effusion but no evidence of bony deterioration. Intraoperative arthrocentesis with washout and synovial biopsy was performed, with good recovery. Unfortunately, at a follow-up visit in the infectious disease clinic shortly after discharge, it was noted that the patient's left knee was still warm and swollen. He was readmitted and orthopedics was consulted. An intraoperative arthrocentesis revealed a communicating anterior thigh abscess, which was drained. Because neutropenia had developed, his antibiotic regimen was switched from penicillin G to clindamycin. His white blood cell and neutrophil counts returned to normal, and he was discharged on a regimen of oral clindamycin, with a recommendation for close monitoring.
Complications of Group A Streptococcal Infection
Table – Criteria for streptococcal toxic shock syndrome
Hypotension or shock plus 2 of the following:
A definite case manifests hypotension, at least 2 of the above criteria, and isolation of group A streptococci from a sterile site. A probable case manifests hypotension, at least 2 of the above criteria, and isolation of group A streptococci from a nonsterile body site.
ARDS, acute respiratory distress syndrome.
Direct complications of streptococcal infections include retropharyngeal abscesses (abscess formation between the posterior pharyngeal wall and prevertebral fascia) and toxic shock syndrome (TSS). TSS can be caused by both streptococcal and staphylococcal bacteria. Criteria for establishing the diagnosis of TSS are shown in the Table.
The pathophysiology of streptococcal TSS involves massive cytokine release triggered by toxins that are produced by group A streptococci and that act as superantigens. Streptococcal TSS is often accompanied by a local infection, such as cellulitis or necrotizing fasciitis.
Indirect complications of group A streptococcal (GAS) infection include acute rheumatic fever and poststreptococcal glomerulonephritis, both of which follow acute untreated GAS infection after an asymptomatic latency period of about 7 to 10 days. These indirect complications can follow either a skin or a pharyngeal infection.
Acute rheumatic fever is a systemic illness characterized by carditis, polyarthritis, chorea, subcutaneous nodules, and erythema marginatum. Minor diagnostic criteria include fever, arthralgia, a prolonged PR interval, and elevated erythrocyte sedimentation rate and C-reactive protein level.
Acute poststreptococcal glomerulonephritis is characterized by edema, hematuria, proteinuria, and hypertension. It is an acute nephritis in which inflammation of the glomerulus is caused by cellular elements produced by an immunological mechanism.
References:
FOR MORE INFORMATION:
•
Jaggi P, Shulman ST. Group A streptococcal infections.
Pediatr Rev
. 2006;27: 99-105.
•
Stevens DL, Tanner MH, Winship J, et al. Severe group A streptococcal infections associated with a toxic shock-like syndrome and scarlet fever toxin A.
N Engl J Med
. 1989;321:1-7.
•
Weiss K, Laverdière M, Lovgren M, et al. Group A streptococcus carriage among close contacts of patients with invasive infections.
Am J Epidemiol
. 1999;149:863-868.
a For a discussion of the direct and immune-mediated complications of group A streptococcal infections, visit our Web site at www.ConsultantLive.com/pediatrics.
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.