Congenital malalignment syndrome
A 13-year-old girl presents with great toenails have become yellow, thickened, ridged, and crusted proximally on the left over the last 8 months.
The case
You are asked to evaluate asymptomatic toenail changes in a 13-year-old girl whose great toenails have become yellow, thickened, ridged, and crusted proximally on the left over the last 8 months. What’s the diagnosis?
Figure

Diagnosis: Congenital malalignment syndrome
Congenital malalignment syndrome or congenital malalignment of the great toes.
Congenital malalignment syndrome is a dystrophic nail disorder caused by the lateral rotation of the nail matrix. The malalignment results in altered growth of the nail plate that is not directed along the major axis of the distal phalanx.1 Clinical appearance presents as lateral deviation of the nail plate, nail plate thickening, nail discoloration (brown, black, green-brown, yellow), transverse grooves across the nail, and frequently only involving the great toes.1,2
Complications of the disorder include acute/chronic paronychia, onychogryphosis (hypertrophy of nail), onycholysis (detachment of the nail from bed), onychomadesis (shedding of a large portion of the nail), onychocryptosis (ingrown nail), hyperkeratosis (increased scaling of the nail bed), brachyonychia (short nail), and discoloration of the nail plate.1-3 Variations in the condition include medial deviation, the involvement of other toes and fingers, and single toe involvement.
The disorder is generally present at the time of birth. However, in individuals with minimal deviation, clinical manifestations may not be apparent until a child is older or begins to experience repetitive microtraumas or mechanical stress to the toenail from tight shoes, activities, and sports.1,3
The etiology and pathogenesis of congenital malalignment are debated in the literature. Etiology is thought to be due to autosomal dominant genetic factors, extrinsic factors including constriction of toes by amniotic bands, increased intrauterine pressure, vascular abnormalities during fetal life, or a combination of genetically determined malalignment plus superimposed cumulative effects of postnatal trauma.1,4 Pathological features are discussed as increased tension of the extensor tendon of the hallux and desynchronization in growth between the nail and the distal phalanx of the hallux, resulting in larger nail plates.1,2
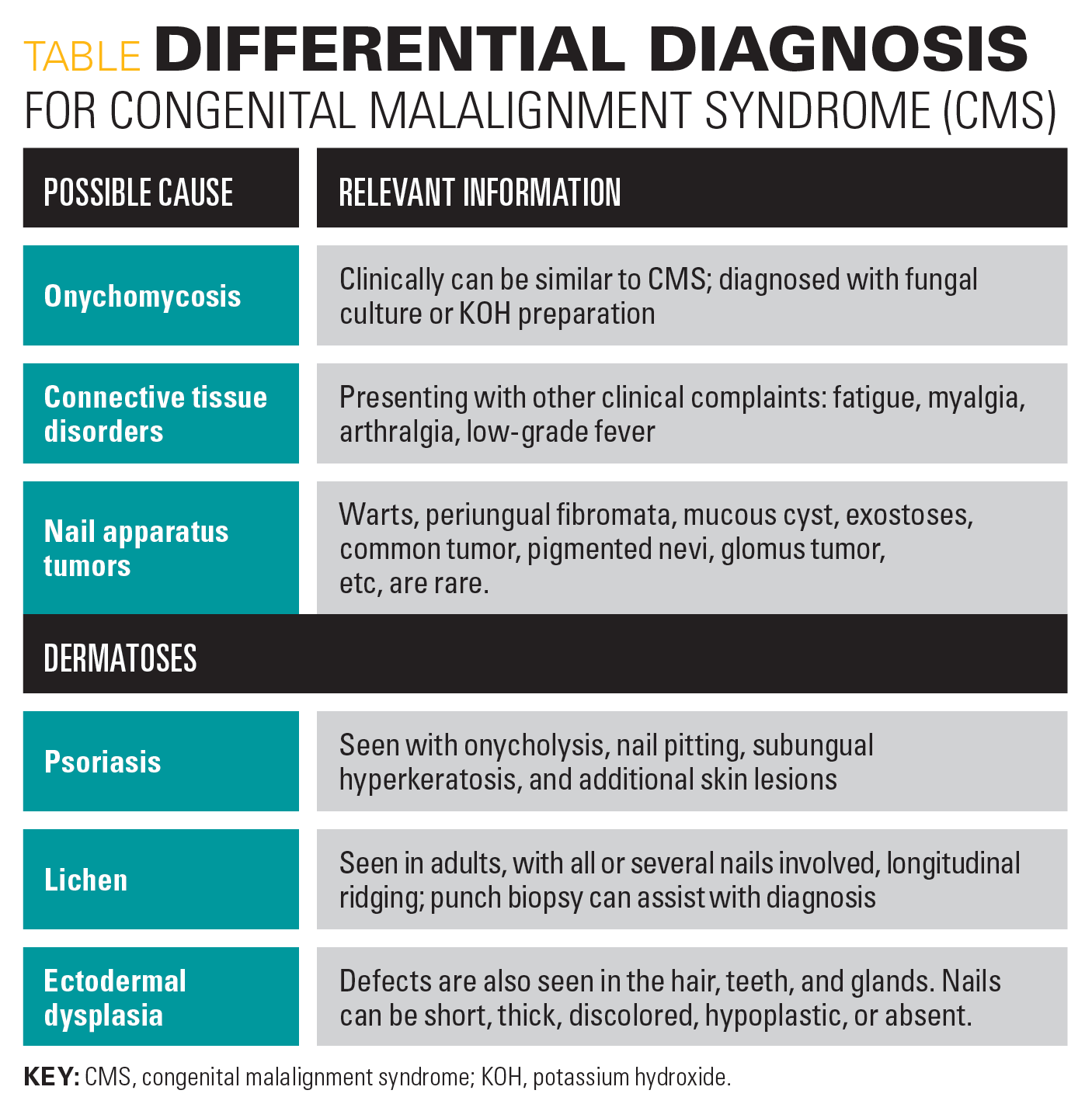
Differential diagnosis
The Table shows that a differential diagnosis would include onychomycosis, connective tissue disorders, nail apparatus tumors, and dermatoses with nail involvement (psoriasis, lichen, and ectodermal dysplasia).1,2
Table
Treatment
The treatment of congenital malalignment is based on the degree of deviation. Spontaneous improvement may occur in half of patients before age 10 years.2-4 Conservative treatment in an individual with minimal deviation involves managing complication and wearing proper-fitting, comfortable footwear.2,5 Severe deviations may call for surgery to align the nail matrix and nail plate, and positional correction or elongation of the extensor tendon of the hallux.2 Nail matrixectomy would be an option for those who would tolerate the cosmetic deficit.1,5
Our patient
There was no family history of any nail disorder in this family. The patient was not symptomatic, and subsequently, the patient and mother were educated on the diagnosis and treatment. It was recommended that she switch to wider, comfortable footwear and avoid high-heeled shoes. Complications such as fungal and bacterial infections can be treated as they arise.
A dermatology referral was offered for possible nail matrixectomy, or nail matrix and nail plate realignment. The patient was educated that spontaneous resolution sometimes happens but typically occurs in those younger than 10 years. She has had no subsequent follow-up visits for this specific issue.
References
- Catalfo P, Musumeci ML, Lacarrubba F, Dinotta F, Micali G. Congenital malalignment of the great toenails: a review. Skin Appendage Disord. 2018;4(4):230-235. doi:10.1159/000484943
- Batalla A, Curto JR. Congenital malalignment of the great toenail. Report of two cases. Dermatol Online J. 2014;20(1):21251.
- Pollack K, Zlotoff B, Wilson B. Hyperkeratosis and discoloration of the toenails in an 8-year old. J Pediatr. 2017;189:233. doi:10.1016/j.jpeds.2017.05.059
- Ҫayirli M, Parlak N, Parlak A, Ӧzenҫ S. Congenital malalignment of the great toenails. J Turk Acad Dermatol. 2016;10(1):16101l1. doi:10.6003/jtad.16101I1
- Decker A, Scher RK, Avarbock A. Acquired congenital malalignment of the great toenails. Skin Appendage Disord. 2016;1(3):147-149. doi:10.1159/000441391
Recognize & Refer: Hemangiomas in pediatrics
July 17th 2019Contemporary Pediatrics sits down exclusively with Sheila Fallon Friedlander, MD, a professor dermatology and pediatrics, to discuss the one key condition for which she believes community pediatricians should be especially aware-hemangiomas.