Daytime wetting: Getting to the bottom of the issue
When children are incontinent during the day, it's generally because of a functional bowel or bladder disorder. Successful treatment calls for a systematic evaluation to identify the disorder, followed by behavioral modification and medication. Strong motivation is a must.
Daytime wetting:
Getting to the bottom of the issue
By Anthony J. Casale, MD
When children are incontinent during the day, it's generally because of a functional bowel or bladder disorder. Successful treatment calls for a systematic evaluation to identify the disorder, followed by behavioral modification and medication. Strong motivation is a must.
Daytime wetting past the age of continence is never normal. This age varies with the child, with most children gaining control of urine during the day before they stop wetting at night. A few children develop urinary continence during the day at 18 months, while others are 4 years old before they achieve this control.1 By 5 years of age, 92% of children are consistently dry and 95% have been dry during the day for extended periods of time.2 During toilet training children have intermittent problems with wetting, and these transitional difficulties do not need treatment. In deciding if a child needs evaluation for urinary incontinence, pediatricians should consider the child's overall level of development and maturity and any other medical problems that may influence continence.
Daytime urinary incontinence (diurnal enuresis) is a different problem than simple nocturnal enuresis or bedwetting. Treatment of bedwetting alone usually fails when the child also has symptoms of urinary incontinence during the day. On the other hand, successful treatment of daytime incontinence often results in the simultaneous resolution of bedwetting. To address the problem of daytime wetting, pediatricians need to understand its causesmost often functionaland how to evaluate the child with a problem. Once the specific disorder is identified, treatment with behavioral modification and medication to make the bladder easier to control often succeedsif the child is highly motivated. The pediatrician can manage most daytime incontinence but should consider referral to a urologist when the cause of the condition is not clear or treatment fails to resolve the problem.
How functional disorders cause wetting
Urinary incontinence may be caused by uncommon anomalies such as ectopic ureter, neurogenic bladder, epispadias, posterior urethral valves, or strictures. Daytime wetting may also result from physical or sexual abuse, but this is rare. Most often children who wet during the day have normal urinary anatomy and nervous systems. In the vast majority, a functional disorder of bowel or bladder, a combination of behavioral and physiologic dysfunction, is causing the incontinence, not an anatomic or neurologic problem (Table 1). Urinary incontinence is much more common in girls than in boys.

Daytime wetting is often only one symptom of a dysfunctional voiding problem. Children who wet during the day commonly suffer from recurrent urinary infection, nighttime incontinence, hydronephrosis, and persistent vesicoureteral reflux. Pediatricians may refer a child with recurrent infections to a urologist without realizing that the infections are caused by an underlying bladder dysfunction. Frequently, children who have functional voiding disorders also have bowel problems, such as constipation and encopresis. Because this combination (dysfunctional elimination syndrome) is so common, the child with incontinence should be evaluated simultaneously for dysfunctional bladder and bowel.3 Treatment of functional bladder problems without attention to the bowel often fails.
Three common, and somewhat overlapping, forms of dysfunctional voiding most often lead to daytime wetting and infection: lazy bladder syndrome, bladder muscle instability, and detrusor sphincter dyssynergiaa failure in coordination between the bladder muscle and the sphincter (Table 2). In some patients one form of dysfunction seems to give way to another if the initial condition is not treated. A radiographic voiding cystourethrogram (VCUG) and urodynamics, which are volume pressure studies of the bladder with electromyography (EMG) of the sphincter, help define the problem.

Lazy bladder syndrome is characterized by habitual urinary retention.4 The patient, usually a girl, voids a large amount of urine only once or twice a day. The sensation of bladder fullness is diminished or absent, and bladder capacity is very large. Incontinence is caused by overflow and may be triggered by physical activity. The voiding pattern usually persists for some time before the child begins to have problems with urinary tract infection (UTI) and incontinence. The condition may start with learned behavior when a small child misinterprets a parent's encouragement to hold her urine and thinks that fewer trips to the bathroom are always better. Bladder retraining and antibiotic suppression of infection can improve and reverse the condition.
The VCUG reveals a large-capacity bladder, usually with smooth walls, and a large postvoid residual urine. The urethra is normal, and reflux is not a common finding. Urodynamics show decreased sensation with filling, low bladder pressures, relatively normal sphincter activity on EMG, and an intermittent urinary flow rate caused by poor bladder muscle contractions and valsalva voiding.5 The child voids three times or less in a 24-hour period.
The volume voided may vary considerably, depending on the child's effort and attention. Children often delay their first void in the morning for hours and avoid using the toilet at school under any circumstances. If wet long enough, they no longer are aware that their skin is damp and develop a characteristic odor of urine that even bathing does not remove. Lazy bladder is almost always accompanied by chronic constipation and often by encopresis. The child feels a decreased urge to empty her bowel and tends to retain her stool .
Bladder muscle instability (unstable bladder), resulting in uninhibited bladder contraction, is an important cause of daytime incontinence. Children with daytime wetting caused by bladder instability have a history of urgency and frequency. They often posture in ways that allow them to delay voiding with a full bladderholding their perineum, crossing their legs, or squatting to sit on their heels (Vincent's curtsy).6 With unstable bladder, incontinence is typically associated with urgency.
The VCUG usually reveals only mild trabeculation, an irregular outline of the bladder interior caused by uneven thickening of the bladder wall. Urodynamics demonstrate uninhibited contractions at low bladder volumes. Children with this condition have small-capacity bladders and sensation is variable. When the bladder is full, and sometimes during filling, the bladder muscle contracts and the sphincter relaxes spontaneously. The child cannot suppress this unwanted voiding.5
The voiding history reveals severe urinary frequency. Some children void every 30 minutes or even more often. Children with this condition usually wet several times during the day and have frequent episodes of posturing. The condition may be accompanied by infrequent stools and constipation.
Severe constipation also can be the cause of bladder instability and uninhibited contractions.7 In these instances, bladder function improves when the constipation is treated. Recurrent infections may irritate the bladder and cause bladder contractions. Some children with an unstable bladder have mild neurologic anomalies such as poor coordination or exaggerated deep tendon reflexes. There may be a family history of urgency, frequency, and incontinence.5
Detrusor sphincter dyssynergia. The loss of coordination between the sphincter and the bladder is the cause of this form of bladder dysfunction. Daytime wetting results when the sphincter is not sufficiently relaxed during voiding. When the bladder is full, the detrusor muscle contracts and urine is forced through the closed sphincter, resulting in an intermittent stream. Voided volumes are small and emptying is incomplete, leading to recurrent infection, urgency, frequency, and urge incontinence.
The VCUG shows a mildly trabeculated bladder, which may be small or enlarged. During voiding, the urethra resembles a spinning top, with dilation of the proximal urethra and narrowing at the membranous urethra. In the past this finding has been attributed to an anatomical narrowing of the urethra by a congenital stricture or ring in girls and by posterior urethral valves in boys. We now know that the narrowing is caused by contraction of the external sphincter during voiding.8 Urodynamics show a small bladder with increased pressures during filling, and especially during voiding. EMG of the sphincter shows increased sphincter activity during voiding.5
Don't forget the giggles
Other functional disorders that can cause daytime wetting include Hinman syndrome and post-void incontinence as well as giggle incontinence.
Hinman syndrome (nonneurogenic neurogenic bladder) is an uncommon cause of incontinence.9 Children with this condition have symptoms and radiographs similar to those of patients with neurogenic bladder (those with myelomeningocele or spinal cord injury) and an apparently normal nervous system. They urinate infrequently with an intermittent stream and have urge incontinence. These children usually suffer from recurrent infections and constipation. Imaging generally reveals thickened bladder walls with reflux and hydronephrosis. The external sphincter remains contracted with voiding. Urodynamics confirm a loss of coordination between the bladder and sphincter. The cause of this disorder is thought to be mostly psychologic.
Postvoid incontinence strikes girls when voided urine is trapped in the vagina either by labial fusion or when they urinate with their legs too close together. When the child stands upright to leave the toilet the urine drains into her underwear. Children with this problem are dry except just after they have urinated, and the VCUG sometimes documents vaginal voiding. Otherwise, the bladder functions normally. The child simply is instructed to spread her legs far apart when she urinates and to sit forward on the toilet to promote emptying.
Giggle incontinence is a rare cause of diurnal enuresis. Children with this condition, mostly girls, wet only when they are giggling. They have normal toilet habits and urinary tracts. They simply are unable to inhibit urination when they laugh. This is a self-limited condition and improves with age, but it can cause significant embarrassment and concern. Treatment success using methylphenidate hydrochloride (Ritalin) has been reported.
How bowel dysfunction affects the urinary tract
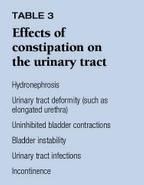
Three decades ago, researchers first observed that chronic constipation had an effect on urinary tract function and that when constipation was relieved, urinary tract function improved.10 Other investigators discovered that patients with functional constipation had significant urinary tract changes, such as elongated urethra, cone-shaped bladder neck, hydronephrosis, bladder wall changes, and reflux (Table 3).11 A more recent investigation of children with functional constipation and UTI revealed that when constipation was corrected, infections improved or resolved in 80%.12
Constipation has long been documented as a cause of wetting and uninhibited bladder muscle contractions. In a study of 234 children with chronic functional constipation, 89% of those who also had urinary incontinence became dry during the day and 63% became dry at night when the constipation resolved.13 In the children with an anatomically normal urinary tract, chronic UTI resolution was 100%. Other research shows that among children with vesicoureteral reflux, those with bowel and bladder dysfunction are the most likely to have breakthrough UTI and to need surgery. Reflux also resolves more slowly in these children, and they have a higher rate of UTI.1
The exact nature of the interaction between bowel and bladder dysfunction is not defined, but it is known that bacteria responsible for UTI arise predominantly from the colonic flora. Thus, infection may develop when a change in bowel habits results in more fecal soiling. Some of the effects of bowel on bladder function may result from physical displacement of the lower urinary tract by accumulated feces within the bony pelvis. A neurologic component also is likely because a distended colon alters bladder sensation and bladder contractility. In our pediatric urology clinic we frequently find a relationship between UTI, reflux, and urinary incontinenceall related to bowel and bladder dysfunction.
Making the evaluation
Evaluation of the child with daytime incontinence (Table 4) should include a through physical examination. Laboratory examination has a less important role, while a complete history of urinary and bowel function is mandatory. Imaging is also helpful.

Physical examination. Palpate the abdomen for masses that might represent a distended bladder, kidney, or colon. Observe the lower back for skin signs of spinal cord anomalies such as pigmented or hairy patches, sinuses, or masses caused by lipomas. Examine the external genitalia; in girls, a bifed clitoris may indicate epispadias, which can cause incontinence because the bladder neck is incompetent. The vaginal introitus may be covered by labial adhesions that lead to urine pooling after voiding and subsequent wetting. The appearance of the anus may give information about neurologic function, and a gaping anus may indicate poor pelvic floor enervation. Likewise, asymmetry of the buttocks, gluteal crease, or legs and feet may point to spinal cord problems. A simple neurologic exam is necessary to rule out nervous system pathology. Observation of walking gait and the ability to climb onto the examination table gives insight into coordination. Simple knee reflexes and examination of strength at the foot and ankle are also helpful.
Laboratory examination has limited value but a urinanalysis is mandatory to evaluate the white blood cell count and red blood cell count, detect nitrates, and rule out infection. The specific gravity of the urine will help rule out diabetes insipidus (either neurogenic or renal). Urine glucose will help rule out diabetes mellitus. Serum electrolytes, blood urea nitrogen, and creatinine may be helpful in patients suspected to have metabolic or renal disease.
History of urinary and bowel function. The history is usually more helpful than the physical exam and can be divided into these areas: normal development, associated urologic history, associated medical and behavioral problems, pattern of incontinence, and bowel function. Ask when the child was toilet trained and if there were physical or behavioral difficulties. Is the child at the proper developmental stage in other aspects of life, such as school? Was the child ever dry for an extended period of time? Urologic problems like infection, hematuria, and a history of reflux or hydronephrosis are also important in determining the cause of wetting. Other medical or behavioral problems may play a role, though the family may not immediately recognize them as relevant. Children who are performing poorly in school or who are in an abusive environment, for example, may exhibit incontinence. Inquire about medications and other problems that require attention and treatment. The family may not offer this information.
To define the pattern of incontinence, establish the age at which the problem began, when the child wets and how frequently, and how much urine is released. You can learn a lot from the behavior that is associated with wetting and voiding, such as posturing to prevent wetting and rushing to the bathroom only to wet on the way or not void on arrival because the urge passes. Is the wetting an isolated happening or does it always occur just before or after urinating?
What does the child seem to know about the need to void? Is she unable to feel when her bladder is full or can she suppress this feeling? Does the child see the incontinence as a problem? Does she wet while she is asleep as well as when she is awake? Does giggling precipitate incontinence?
Investigating the child's bowel habits is especially important. Is the child constipated and does he require treatment? Although parents may deny the child has encopresis and say he just doesn't wipe properly, closer questioning may reveal that the child frequently has stool in his pants. Ask about frequency and size of bowel movements and any accompanying pain or bleeding. Don't be surprised if parents display a startling lack of knowledge about their child's problem and toilet habits.
When children are referred to us, we ask the parents to keep a detailed voiding and bowel diary for several days. It records times of urination with the amount voided, bowel habits, bathroom behavior, and when and under what circumstances the child wets, with estimated amounts. We explain in detail the technique for collecting this information and then have a nurse repeat it. We also give the family written instructions and a container to measure voided urine. They may return the information by fax, mail, or in person at the next visit. Most normal children void four or five times a day and have a bowel movement every day or two.14
Imaging. Unlike children with purely nocturnal enuresis, children with daytime incontinence often merit imaging of the lower and upper urinary tract. Imaging is unnecessary when the pediatrician can manage the problem with simple behavioral modification techniques. If this treatment is ineffective, however, the child should be referred to a urologist, who will perform imaging studies. For the bladder and urethra we prefer a VCUG. A nuclear cystogram may be adequate for following vesicoureteral reflux but does not offer enough information for evaluating incontinent children. The VCUG provides a plain film of the abdomen, which reveals the spine, sacrum, and pelvic bones, along with the bowel gas pattern and amount of stool in the colon. The bladder films show the thickness of the bladder wall, shape and size of the bladder, and whether it is displaced or distorted by feces. This part of the study may also identify diverticuli, trabeculation, and reflux. The voiding films make it possible to visualize the urethra and bladder neck during urination and to rule out obstruction. The post-void film shows any urine retained in the bladder or vagina.
Upper tract imaging is now done almost exclusively with ultrasound. The size and shape of the kidneys and the presence of hydronephrosis or a duplication of the collecting system should be noted. Ultrasound of the pelvis can detect dilated ureters extending below the bladder neck or ureteroceles at the bladder level. If the clinician suspects that a duplicated system with an ectopic ureter is causing incontinence, an intravenous pyelogram or CT scan may help define the renal anatomy. The child with a spinal anomaly or neurologic findings should have magnetic resonance imaging of the back to evaluate the spinal cord.
Red flags. Certain warning signs indicate that the child has more than a common functional problem. Worsening of the incontinence or development of any neurologic sign, such as weakness or pain in the back or legs, requires neurosurgical evaluation. Any significant bleeding in the urine, stool, or introitus calls for more extensive evaluation by appropriate specialists. Signs of elevated urine volumes and dilute urine should lead to a nephrologic or endocrinologic evaluation.
Addressing the problem
The first step in treating childhood urinary incontinence is to educate the parents and child about its underlying cause. Also determine if the child perceives incontinence as a problem and if she is willing to cooperate with treatment. Sometimes the child is oblivious to the situation or has grown so frustrated with being wet that she has given up all hope. Treatment of functional incontinence is successful only if the child's motivation is strong because medication without behavioral change usually fails. Parental commitment also is important, and the family must understand that treatment will usually take a long time.
Behavioral modification and medication intended to improve bladder dynamics are the mainstays of therapy for dysfunctional voiding (Table 5). The voiding history determines treatment along with the VCUG and, sometimes, urodynamics. If the child has problems that are associated with the wetting, such as UTI or vesicoureteral reflux, she is managed with nightly antibiotic prophylaxis to keep the urine sterile. Trimethoprim-sulfamethoxazole or nitrofurantoin is used, generally in a dose that is 25% of the normal treatment dose. Routine urine checks may be necessary to ensure that the urine remains uninfected.

If the child has lazy bladder and voids infrequently, a simple timed voiding schedule with the goal of voiding a certain amount may be all that is necessary. In our practice, we ask parents to try and connect trips to the bathroom to routine, scheduled events, preferably mealtimes and bedtime. These four occasions break the day into almost equal segments, accounting for four voids a day. We review the amounts voided on the recorded record and the child's projected bladder capacity (volume in ounces equals age in years + 2) and try to have the child empty at least 75% of total bladder capacity at each trip.
For children in school, we do not require measuring the voids, but we ask the family to have the teacher remind the child to void at routine bathroom breaks. We like to avoid giving the child unlimited bathroom passes since it usually fails to help incontinence and disrupts school work. We ask the parents to record carefully when the child urinates at home and in what amount, along with how successful she is in staying dry. Parents should discuss this record with the child and focus on the positive behavior of voiding rather than episodes of wetting.
If the child has urinary frequency from bladder instability we use a voiding schedule but add anticholinergic and antispasmodic medication, such as oxybutynin chloride or hyoscyamine sulfate. Medication makes it easier for the child to void less often and to hold more urine in the bladder.
The child with poor sphincter-bladder coordination is also put on a schedule, but anticholinergics may or may not be helpful. Getting these children to empty their bladders is the biggest challenge. Biofeedback techniques used in conjunction with an EMG of the sphincter and a urinary flometer may be necessary to teach the child how to empty the bladder and relax during voiding. This is a time-consuming and expensive treatment and should be used only when more conservative measures fail. We have been studying the effects of a blocker drugs on children with voiding disorders and feel that they may have a place.
The child who has significant problems with constipation and bowel dysfunction should be managed with a high-fiber diet, stool softeners, and a schedule that calls for a daily bowel movement. Just as with the voiding schedule, the child often denies the need to go to the bathroom and may forcefully resist. We explain to parents the importance of emptying the bladder and rectum regularly and encourage them to remain positive and unemotional while maintaining the schedule and records.
Worth the effort
The child with daytime urinary incontinence suffers the discomfort of being wet, the skin odor that comes with constant urine exposure, and frequent rashes. The social problems that accompany daytime incontinence are an even greater burden. Continued incontinence strains the relationship between the child and parent, between child and teacher, and sometimes between parents. Wetting inhibits social development by embarrassing the child and promoting insecurity.
The pediatrician can manage many wetting problems with simple behavioral modification. Wetting that is associated with other problems or the failure of initial management suggests consultation with a pediatric urologist. Children with persistent daytime urinary incontinence often have functional disorders of bowel or bladder, frequently accompanied by UTI, vesicoureteral reflux, constipation, or encopresis. Successful treatment calls for a detailed history of the child's toilet habits and a VCUG to evaluate the bladder and urethra, along with an ultrasound of the kidneys. The history, urinanalysis, and physical exam should rule out other conditions that may cause incontinence, such as diabetes or neurologic problems. The voiding history usually identifies the type of bladder dysfunction the child has and indicates the management plan: a toilet schedule, medication to make the bladder easier to control, and treatment for constipation. Treatment requires time and commitmentby both the child and her parentsbut generally is successful.
REFERENCES
1. Yeats WK: Bladder function in normal micturition, in Kolvin I, MadKeith RC, Meadow SR (eds): Bladder Control and Enuresis. Philadelphia, PA, JB Lippincott, 1973, p 3
2. Elder J: Personal communication, 1998
3. Koff SA, Wagner TT, Jayanthi VR: Relationship among dysfunctional elimination syndromes, primary vesicoureteral reflux and urinary tract infections in children. J Urol 1998;160:1019
4. DeLuca FG, Swenson O, Fisher JH, et al: The dysfunctional "lazy" bladder syndrome in children. Arch Dis Child 1962;37:117
5. Bauer SB, Retik AB, Colodny AH, et al: The unstable bladder of childhood. Urol Clin North Am 1980;7:321
6. Vincent SA: Postural control of urinary incontinence. The curtsy sign. Lancet 1966;2:631
7. O'Regan S, Yazbeck S, Schick E: Constipation, bladder instability, urinary tract infection syndrome. Clin Nephrol 1985;23:152
8. VanGool JD, Tanagho EA: External sphincter and urinary tract infection in girls. Br J Urol 1977;10:348
9. Hinman F: Urinary tract damage in children who wet. Pediatrics 1974; 54:142
10. Swenson O: A new concept in the pathology of megaloureters. Surgery 1952;32:367
11. Schopfner CE: Urinary tract pathology associated with constipation. Radiology 1968;90:865
12. Neumann PZ, deDominic IJ, Nogrady MB: Constipation and urinary tract infection. Pediatrics 1973; 52:241
13. Loening-Baucke V: Urinary incontinence and urinary tract infection and their resolution with treatment of chronic constipation of childhood. Pediatrics 1997;100:228
14. Bloom DA, Seeley WW, Ritchey ML, et al: Toilet habits and continence in children: An opportunity sampling in search of normal paramaters. J Urol 1993; 149:1087
THE AUTHOR is Associate Professor, Pediatric Urology, Indiana University School of Medicine, Indianapolis.
Anthony Casale. Daytime wetting: Getting to the bottom of the issue. Contemporary Pediatrics 2000;2:107.
Having "the talk" with teen patients
June 17th 2022A visit with a pediatric clinician is an ideal time to ensure that a teenager knows the correct information, has the opportunity to make certain contraceptive choices, and instill the knowledge that the pediatric office is a safe place to come for help.