First seizure: Dispel the myths
When a child experiences a seizure for the first time, frantic parents turn to their pediatrician for answers about what just happened and what to do next. The conversation should begin by discussing exactly what a seizure is and what it is not.
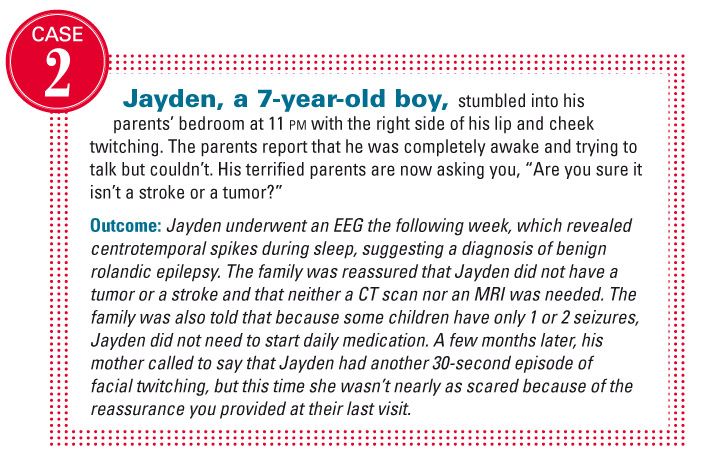
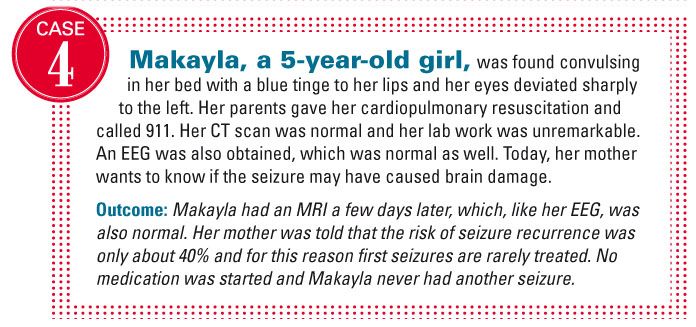
There are few things more terrifying for parents than witnessing their child having a seizure. Clinicians who work with these families can attest to the fact that one of the most commonly heard fears following a seizure is, “I thought my child stopped breathing and was going to die.” In many cases, these children are transported emergently to the hospital, have a computed tomography (CT) scan of the brain, have blood drawn, are observed for a few hours, and are then discharged home with instructions to follow up with their pediatrician. The parents, searching for answers, turn to their pediatrician for help and ask, “Now what do we do?” Meanwhile, the pediatrician may be wondering the same thing.
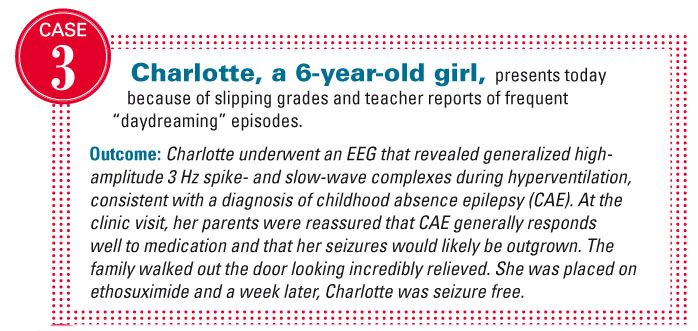
Following a first seizure, the pediatrician’s primary role is to provide accurate information, dispel myths, and address parental anxiety as quickly as possible. For children with a first unprovoked (nonfebrile, nontoxin-induced) seizure, a child neurologist consultation is warranted, but a 5-minute conversation with the pediatrician can prevent hours of worry. The conversation should begin by discussing exactly what a seizure is and what it is not.
What is a seizure?
A seizure is defined as a clinical (or subclinical) event caused by abnormal and excessive firing of neurons in the brain. We will often provide the analogy of “static on your television” to help children understand. Epilepsy, simply put, is diagnosed after 2 or more unprovoked (nonfebrile) seizures.1 Parents should be reassured right from the beginning that having a single seizure is not the same as having epilepsy, although sometimes epilepsy is diagnosed after a single seizure if the electroencephalogram (EEG) is abnormal and suggests a high likelihood of seizure recurrence. Inevitably, parents will ask what caused the seizure and often the answer to this question is unknown.
Many seizures are “idiopathic” and presumed to be genetic in etiology, with genetic factors accounting for 80% of idiopathic epilepsies.2 Parents will frequently worry that the seizure was brought on by a brain tumor. They should be reassured that a seizure alone is an extremely rare presentation for most tumors. They may also worry that their child stopped breathing during the seizure or was close to death, an understandable fear given that many children become cyanotic during a convulsion, with a blue tinge to the lips and eyelids. Caregivers should be reassured that although seizures are frightening and it appeared that their child was not breathing, there is no evidence that seizures lasting less than 30 minutes cause anoxic brain injury.
After the trauma of witnessing a seizure, it can be difficult for parents to view their child as “normal.” Parents need to hear that their child can, and should, resume normal activities. This means that the child should sleep alone in his or her own bed (but not on the top bunk), should still be in school, can play video games (unless photic stimulation on an EEG elicits events, which is rare) and watch movies, and should still take out the trash and do chores.
Children who have experienced a seizure can safely participate in almost all activities, with the exceptions being scuba diving, sky diving, and activities involving projectile weapons such as guns and bows and arrows. The concern regarding these sports stems from the possibility of harm to not only the child but also to another person in the case of a seizure. Most sports are fine as long as proper protective equipment is worn, such as harnesses when rock climbing, and a child can safely ride a bike as long as he or she is wearing a helmet. Parents should be informed that swimming is also safe as long as the child is fully supervised by an adult who is aware that the child has had a seizure.3
Evaluation
Following an unprovoked (nonfebrile) seizure, children often undergo an extensive workup, although it may not always be warranted. In 2000, the Quality Standards Subcommittee of the American Academy of Neurology published a practice parameter evaluating a first nonfebrile seizure in children to help guide clinical decision making and prevent unnecessary testing.4 A review of the literature showed that there was insufficient evidence to support performing routine laboratory testing on every child following a first unprovoked seizure. Blood studies, however, were recommended in children exhibiting other concerning clinical findings, specifically vomiting, diarrhea, dehydration, or failure to return to baseline alertness. Toxicology screenings are also recommended in infants, children, and teenagers when a toxic ingestion or exposure is in question. Finally, lumbar puncture was found to be of limited usefulness and is recommended only when there is concern for meningitis or encephalitis.
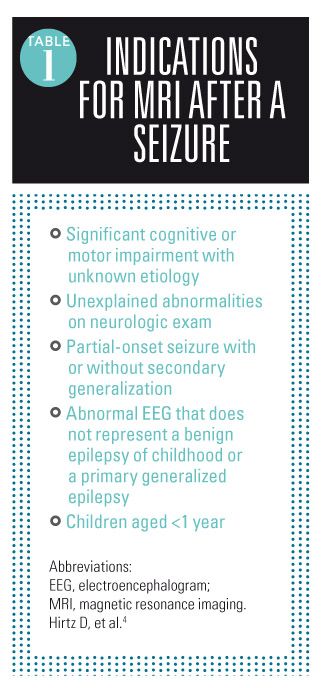
The utility of imaging studies was also assessed. Emergent neuroimaging (ie, CT) should be performed on any child who exhibits a prolonged postictal focal deficit (Todd’s paresis) or fails to return to baseline within several hours of the seizure.4 Nonurgent imaging should be considered for a child with an unexplained cognitive or motor delay, focal neurologic deficits, partial (focal) seizures, and EEG that does not represent a benign epilepsy of childhood, or in children aged younger than 1 year (Table 1).4 If imaging is warranted, magnetic resonance imaging (MRI), not a CT, should be ordered. More detail regarding brain structure is available from an MRI compared to a CT (and the former does not involve radiation).
Finally, the evidence supported obtaining an EEG on almost all children after a first unprovoked seizure.4 The EEG was found to be useful in predicting seizure recurrence (54% vs 25% in children with abnormal EEGs vs normal EEGs, respectively) and determining the need for subsequent neuroimaging studies. An EEG was also helpful in differentiating seizures from other nonepileptic events and critical for diagnosing an epilepsy syndrome. Obtaining the EEG in a center with pediatric epilepsy expertise is best.
Epilepsy syndromes
An epilepsy syndrome is defined as “a complex of signs and symptoms that define a unique epileptic condition.”5 Epilepsy syndromes have a specific presentation, both clinically and electrographically (on EEG), which includes the clinical signs of the events, the timing of the episodes, and the age at onset. A diagnosis of an epilepsy syndrome can be incredibly useful in determining the need for additional testing (eg, whether an MRI is truly needed), helping to guide treatment decisions, and allowing the clinician to provide a long-term prognosis to the family. Thus, when evaluating a child for seizures, assessing whether or not a child fits a particular syndrome is a good place to start.
Although many recognized epilepsy syndromes exist, there are 3 common syndromes frequently encountered by pediatricians about which they need to be especially aware: benign rolandic epilepsy (also known as benign epilepsy with centrotemporal spikes [BECTS]), childhood absence epilepsy (CAE)/juvenile absence epilepsy (JAE), and juvenile myoclonic epilepsy (JME). Representative EEGs are shown in the Figures.
Benign epilepsy with centrotemporal spikes
Benign rolandic epilepsy, or BECTS, is the most common idiopathic epilepsy syndrome seen in school-aged children.6 The majority of seizures (~80%) occur out of sleep or on awakening, but seizures may also occur during the day. Seizures are characterized by drooling and unilateral facial twitching of the tongue, lip, and cheek. Consciousness is generally preserved and the child may attempt to communicate, although speech arrest is common. The child may report full memory of the event, which can at times lead to confusion about whether the event was a true seizure.

FIGURE A EEG of benign rolandic epilepsy
Seizures can sometimes secondarily generalize, particularly in children aged younger than 5 years. Age at seizure onset can be anywhere between 3 and 13 years, with a median age of 7 years. This syndrome has an excellent prognosis, with 95% of children showing complete seizure resolution by 14 years. It is important to note that BECTS has been associated with cognitive, behavioral, and, particularly, language difficulties, which means that the child may require extra support in the form of an individualized education plan or 504 plan.7 The child may also benefit from neuropsychologic testing, if available.6 Academic progress may not be the most sensitive indicator of education-related problems, so further questioning about learning may be needed to diagnose these problems.
Treatment with medication for BECTS is not always required because many children experience only a handful of seizures before outgrowing them. However, if the seizures become frequent, if developmental or academic difficulties emerge, or if extreme parental anxiety is present (eg, “I NEVER want to see a seizure ever again!”), anticonvulsant drugs are an option. Most medications are very effective in controlling seizures, with useful first-line agents being levetiracetam and oxcarbazepine (Trileptal).8
Absence epilepsy
Absence seizures, historically referred to as “petit mal” seizures, are characterized by brief, 5- to 20-second episodes of staring and unresponsiveness, and can occur up to hundreds of times a day.9 A key feature that differentiates absence seizures from other types of staring seizures, such as complex partial seizures, is the lack of a postictal state, with children experiencing absence seizures returning immediately to baseline following the event. Children with absence epilepsy may also experience generalized tonic-clonic seizures, with approximately 30% of children presenting with a convulsion. Absence seizures can be safely diagnosed in the office by having the child hyperventilate (eg, by blowing on a pinwheel). This is absolutely safe and can lead to a rapid diagnosis.
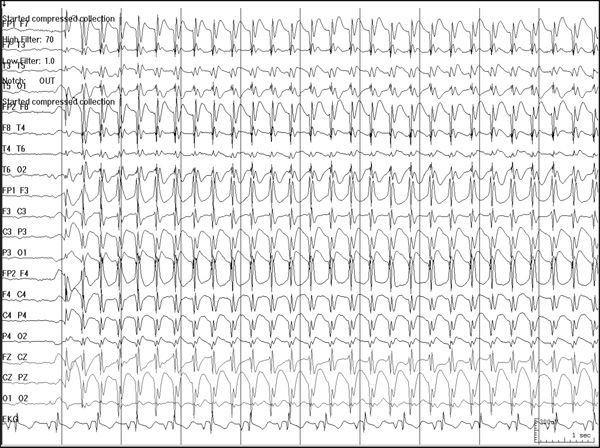
FIGURE B EEG of childhood absence epilepsy
Childhood absence epilepsy, or CAE, occurs in developmentally normal children aged between 4 and 10 years, with the peak incidence between 6 and 8 years. The prognosis is good and seizures are outgrown in approximately 80% of children by adolescence.9 It is important to note, however, that children with CAE have a greater risk of long-term cognitive, behavioral, and linguistic comorbidities as compared with children without epilepsy, making prompt diagnosis and treatment critical.10
Juvenile absence epilepsy, or JAE, on the other hand, is not usually outgrown, and spontaneous remission of seizures occurs far less frequently as compared with CAE, with the presence of generalized tonic-clonic seizures being a predictor of poorer outcome.9 Peak onset for JAE is between 10 and 12 years of age and is more strongly associated with photosensitivity than CAE. In JAE, seizures are most prominent on awakening, and generalized tonic-clonic seizures, often precipitated by sleep deprivation, are common.
First-line treatment for CAE is ethosuximide (Zarontin), followed by valproic acid (Depakote) and lamotrigine (Lamictal).11 Because of its teratogenic effects, valproic acid is rarely used as the initial anticonvulsant in girls aged older than 10 years, with zonisamide (Zonegran) or topiramate (Topamax) being good alternatives.
Juvenile myoclonic epilepsy
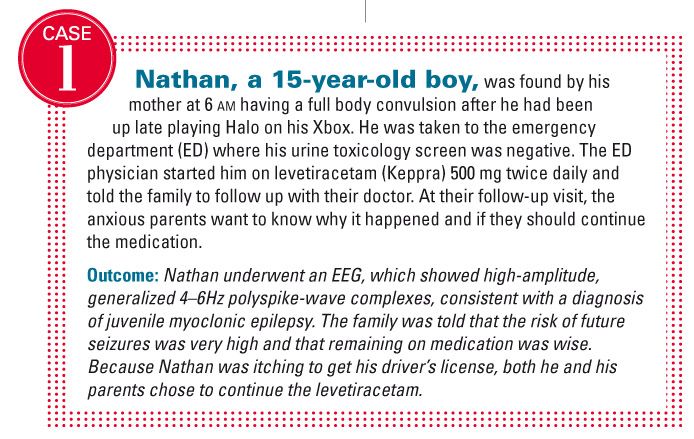
In JME, the most common idiopathic epilepsy syndrome presenting in adolescents and adults,12 a teenager typically presents after experiencing a generalized tonic-clonic seizure on awakening. After careful questioning, the adolescent may also report morning myoclonic jerks that resolve by breakfast. For example, he or she might report losing control of a spoon or toothbrush. This epilepsy syndrome rarely, if ever, remits without medication, but usually responds favorably to anticonvulsants. The most commonly used drugs are levetiracetam, valproic acid, lamotrigine, and zonisamide. Although medication is seldom started in children who have experienced a single seizure, adolescents with a diagnosis of JME are often an exception because of safety concerns such as driving and the high likelihood of recurrence.
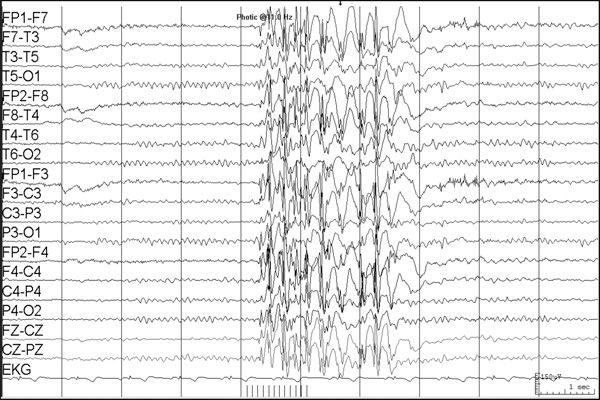
FIGURE C EEG of juvenile myoclonic epilepsy
After a first seizure, the issue of driving is often on the forefront of both the teenager’s and the parents’ minds. The family should be told that epilepsy does not necessarily preclude the teenager from driving, but that he or she must be seizure free to obtain and keep a driver’s license. Clinicians who work with patients with seizures should know the driving laws of their state that pertain to epilepsy, as well as the process for reporting their diagnosis to the state motor vehicle administration.
A frank conversation with teenagers about lifestyle factors is essential in helping them remain seizure free and feeling a sense of control over their epilepsy. Common seizure triggers in patients with JME are sleep deprivation, alcohol use, and, of course, failing to take medication. “But I forgot!” is an all-too-frequent explanation for breakthrough seizures, and teenagers should be given concrete strategies to minimize the chance of seizure recurrence. For example, placing the medication next to his or her toothbrush can be a good reminder, and for those mornings when he or she forgets, medication can be kept in the nurse’s office if permitted by the school. In addition, although schoolwork, extracurricular activities, and part-time jobs can make getting 9 to 10 hours of sleep a night seem impossible, the importance of getting sufficient sleep should be strongly emphasized. Finally, avoidance of alcohol and drugs, including illegally obtained prescription drugs, should be a key part of the discussion.
To treat or not to treat?
After a first seizure, many parents worry that starting medication is inevitable. They should be informed that treatment of a single seizure is rare (with the major exceptions of CAE, JAE, and JME as previously noted). Several prospective studies have found no evidence that treatment of the first seizure affects long-term prognosis, and there is consensus that it is not necessary to prescribe daily antiepileptic drug treatment after a single unprovoked epileptic seizure.13 In addition, it is not uncommon for children to experience a single unprovoked seizure and never have another, with most children having a 40% to 50% chance of recurrence (even if the first seizure was an episode of status epilepticus). Risk of recurrence depends on multiple factors including an abnormal EEG, seizure while asleep, Todd’s paresis, and history of febrile seizures.14
The decision to treat is made when the risks of treating are outweighed by the risks of not treating.15 Every drug carries with it some risk that must be balanced against the risk of harm, both physical and emotional, from seizure recurrence. Treatment with medication is also initiated when risk of seizure recurrence is high, based on the history and the abnormalities on EEG. In some cases, medicine may be started after a first seizure if the EEG clinches a diagnosis of an epilepsy syndrome such as JME.
Primary care provider as 'hero'
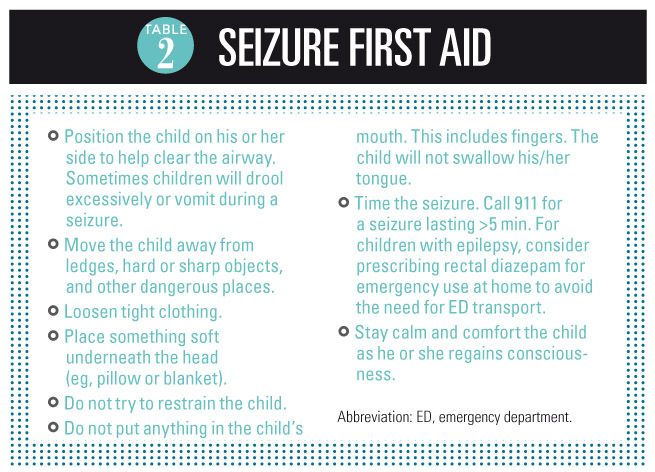
After a first seizure, the pediatrician, armed with some basic knowledge, can be the hero! Providing reassurance and easing parental anxiety is an essential part of managing a child after a first seizure, and the act of doing so can be incredibly rewarding for the pediatrician. Seizure first aid should be discussed with the family, including when to call 911 (Table 2). Having brochures and printed-out information from websites ready to distribute to families can also be very helpful. If the child has had a seizure lasting longer than 5 minutes, the clinician may want to consider prescribing rectal diazepam (Valium). It is safe and easy to prescribe, and with proper parental counseling can prevent unnecessary trips to the emergency department.
Also, when referring a child to a neurologist, consider ordering the EEG in advance, ideally at the center where the child will be seen. If this is not possible, then the closest institution that cares for pediatric patients is acceptable. Note that EEGs that capture sleep tracings are preferable; families should be told to keep the child up late the night before the EEG or instructed to schedule the test during a young child’s naptime. It is important to be aware that the EEG does not need to be done immediately. Although the EEG is more likely to be abnormal within the first 24 hours after a seizure, it will often remain abnormal in children with epilepsy syndromes, and obtaining a good-quality, sleep-deprived EEG is often worth the wait in some cases.16,17
Finally, do not hesitate to ask for help from the child neurologist with whom the child has an appointment, particularly if the child’s case is perceived as urgent. Most neurologists will offer advice, including when to watch and when to worry.
REFERENCES
1. Fisher RS, van Emde Boas W, Blume W, et al. Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE). Epilepsia. 2005;46(4):470-472.
2. Kjeldsen MJ, Corey LA, Christensen K, Friis ML. Epileptic seizures and syndromes in twins: the importance of genetic factors. Epilepsy Res. 2003;55(1-2):137-146.
3. Freeman JM, Vining EPG, Pillas DJ. Seizures and Epilepsy in Childhood: A Guide. 3rd ed. Baltimore, MD: Johns Hopkins University Press; 2002:345-349.
4. Hirtz D, Ashwal S, Berg A, et al. Practice parameter: evaluating a first nonfebrile seizure in children: report of the quality standards subcommittee of the American Academy of Neurology, the Child Neurology Society, and the American Epilepsy Society. Neurology. 2000;55(5):616-623.
5. Muthugovindan D, Hartman AL. Pediatric epilepsy syndromes. Neurologist. 2010;16(4):223-237.
6. Guerrini R, Pellacani S. Benign childhood focal epilepsies. Epilepsia. 2012;53(suppl 4):9-18.
7. Boatman DF, Trescher WH, Smith C, et al. Cortical auditory dysfunction in benign rolandic epilepsy. Epilepsia. 2008;49(6):1018-1026.
8. Kossoff EH, Los JG, Boatman DF. A pilot study transitioning children onto levetiracetam monotherapy to improve language dysfunction associated with benign rolandic epilepsy. Epilepsy Behav. 2007;11(4):514-517.
9. Wirrell EC. Natural history of absence epilepsy in children. Can J Neurol Sci. 2003;30(3):184-188.
10. Caplan R, Siddarth P, Stahl L, et al. Childhood absence epilepsy: behavioral, cognitive, and linguistic comorbidities. Epilepsia. 2008;49(11):1838-1846.
11. Glauser TA, Cnaan A, Shinnar S, et al; Childhood Absence Epilepsy Study Group. Ethosuximide, valproic acid, and lamotrigine in childhood absence epilepsy. N Engl J Med. 2010;362(9):790-799.
12. Auvin S. Treatment of juvenile myoclonic epilepsy. CNS Neurosci Ther. 2008;14(3):227-233.
13. Arts WF, Geerts AT. When to start drug treatment for childhood epilepsy: the clinical-epidemiological evidence. Eur J Paediatr Neurol. 2009;13(2):93-101.
14. Shinnar S, Berg AT, Moshe SL, et al. The risk of seizure recurrence after a first unprovoked afebrile seizure in childhood: an extended follow-up. Pediatrics. 1996;98(2 pt 1):216-225.
15. Haut SR, Shinnar S. Considerations in the treatment of a first unprovoked seizure. Semin Neurol. 2008;28(3):289-296.
16. Gandelman-Marton R, Theitler J. When should a sleep-deprived EEG be performed following a presumed first seizure in adults? Acta Neurol Scand. 2011;124(3):202-205.
17. Shinnar S, Kang H, Berg AT, Goldensohn ES, Hauser WA, Moshé SL. EEG abnormalities in children with a first unprovoked seizure. Epilepsia. 1994;35(3):471-476.
MS DOERRER is a certified pediatric nurse practitioner, John M Freeman Pediatric Epilepsy Center, Johns Hopkins Hospital, Baltimore, Maryland. She has nothing to disclose in regard to affiliations with or financial interests in any organizations that may have an interest in any part of this article.
DR KOSSOFF is associate professor of neurology and pediatrics, Johns Hopkins Hospital, Baltimore. He discloses grant support from Nutricia Inc and consulting for Atkins Nutritionals, Eisai Inc, and Upsher-Smith Laboratories Inc.